ABSTRACT
OBJECTIVES: to analyze and synthesize the available evidence on the effect of parental cannabis use on the risk of sudden infant death syndrome (SIDS).
METHODS: a systematic review was conducted in PubMed/MEDLINE, Embase, Scopus, Web of Science, and the Cochrane Library, from inception to December 2023. The search terms included "marijuana," "cannab*," "Sudden Infant Death," "Sudden Infant Death Syndrome," "SIDS," "Crib Death," and "Cot Death." Study selection was performed independently by two reviewers, with disagreements resolved by a third author.
RESULTS: nine studies were included, all from developed countries. Statistical analyses specifically addressing the association between cannabis use and SIDS were available in seven studies, four of which suggested a positive association. However, limitations included the absence of detailed data on frequency, route, and intensity of cannabis use, with substantial variation in exposure assessment across studies, which hinders comparability.
CONCLUSIONS: Although there is evidence of an association between cannabis use and SIDS, methodological limitations prevent us from inferring causality. More robust research is needed to explore the mechanisms underlying cannabis use during pregnancy and postpartum by mothers and fathers in order to inform preventive recommendations.
Keywords:
Cannabis, Marijuana use, Sudden infant death, Infant health
RESUMO
OBJETIVOS: analisar e sintetizar evidências disponíveis sobre o efeito do consumo parental de cannabis no risco de síndrome da morte súbita do lactente (SMSL).
MÉTODOS: realizou-se revisão sistemática nas bases: Pubmed/MEDLINE, Embase, Scopus, Web of Science e Cochrane Library, desde a origem da fonte até dezembro/2023. Os descritores utilizados foram "marijuana", "cannab*", "Sudden Infant Death", "Sudden Infant Death Syndrome", "SIDS", "Crib Death" e "Cot Death". A seleção dos estudos foi realizada por dois pesquisadores de forma independente, e divergências foram definidas por um terceiro autor.
RESULTADOS: nove estudos foram incluídos, todos realizados em países desenvolvidos. Uma análise estatística correlacionando, especificamente, a SMSL com o uso de cannabis estava disponível em sete estudos, e, em quatro deles, os resultados sugeriram uma associação entre exposição e desfecho. No entanto, há limitações relacionadas a ausência de dados sobre frequência, via e intensidade do uso de cannabis, com variação entre os estudos na forma de avaliação dessa exposição, o que compromete a comparabilidade entre estudos.
CONCLUSÕES: embora haja indícios de associação entre consumo de cannabis e SMSL, as limitações metodológicas impedem inferir causalidade. São necessárias pesquisas mais robustas, que explorem mecanismos subjacentes ao uso de cannabis na gestação e pós-parto, pela mãe e pelo pai, a fim de subsidiar recomendações preventivas.
Palavras-chave:
Cannabis, Uso da maconha, Morte súbita do lactente, Saúde do lactente
IntroductionSudden infant death syndrome (SIDS) is defined as the sudden death during sleep of any child under one year of age that remains unexplained after a thorough investigation of the case with review of the medical history, including postmortem examination and examination of the place of death, and is characterized as a preventable event.
1 In Brazil, there is still a lack of knowledge about the prevalence of this disease, mainly due to failure in diagnosis and reporting. According to data from the
Departamento de Informática do SUS (DATASUS) (Public Health System Computing Department), 863 deaths from SIDS were recorded in Brazil between 2015 and 2020.
2The risk factors associated with this disease are broad and challenging. However, some are well established and can be categorized as intrinsic—such as the male sex, prematurity, genetic predisposition, and prenatal exposure to cigarettes and/or alcohol—and extrinsic—such as sleeping in prone or lateral decubitus positions, passive smoking, bed sharing with parents, excessive clothing and blankets causing overheating of the infant, soft mattresses, soft objects in the crib, and face covering.
3 Extrinsic factors are considered modifiable.
There is evidence that associate cannabis use during pregnancy with direct harm to the fetus. The proven harmful effects are low birth weight and being small for gestational age, as well as associations with harmful effects for premature birth and admission to the neonatal intensive care unit.
4 In relation to SIDS, there might be a direct relationship between increased risk of SIDS and parental cannabis use; however, the underlying mechanisms have not yet been fully clarified, and the correlation is limited and subject to further investigation.
3,5Nevertheless, the American Academy of Pediatrics (AAP) recommendations for reducing the risk of SIDS emphasize that exposure to nicotine, alcohol, marijuana, opioids, and illicit drugs should be avoided.
6 In Brazil, few studies have evaluated cannabis use during pregnancy, and the most recent data showed use by approximately 4.2% of the pregnant women in a low-income population, suggesting that this is an important public health issue.
7Therefore, this systematic review aims to analyze and synthesize the available evidence on the effect of parental cannabis use on the risk of SIDS, providing an overview of the current state of knowledge in this area. It is hoped that the results of this review will contribute to a better understanding of the risk factors for SIDS and inform effective preventive interventions.
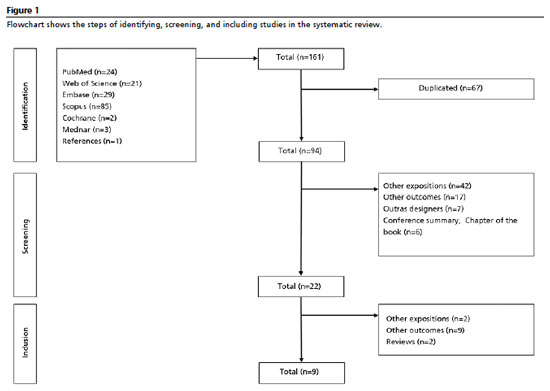
MethodsThis review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)
8 guidelines and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42024560749.
To define the guiding question, the following strategy was adopted: Population (children up to two years of age), Exposure (parental use of cannabis during pregnancy and/or postnatal), Comparison (absence of passive exposure to cannabis during pregnancy and/or postnatal), Outcome (occurrence of sudden infant death syndrome). The guiding question of the research was: "Is there an association between passive exposure to cannabis during pregnancy or after birth and the risk of sudden infant death syndrome?", with passive exposure defined as inhalation of smoke or aerosol from burnt cannabis, or exposure via transplacental.
The research was conducted in December 2023, independently by two researchers, with no restrictions on publication period or language. The consulted databases were: Pubmed/MEDLINE, Embase, Scopus, Web of Science, and Cochrane Library. The search key used was: (marijuana) OR (cannab*) AND (Sudden Infant Death) OR (Sudden Infant Death Syndrome) OR (SIDS) OR (Crib Death) OR (Cot Death).
The selection of studies was performed by two researchers with the aid of Microsoft Excel® in an independent and standardized manner, and possible discrepancies were resolved by a third author. First, the titles and abstracts were read, and in a second phase, the full articles were read. The inclusion criteria were: (i) studies that evaluated exposure to cannabis, at any dose or via any route, during the gestational or postnatal period, (ii) studies that had sudden infant death syndrome as an outcome, and (iii) studies with a case-control, cohort, or retrospective cross-sectional design. The exclusion criteria were: (i) studies with exposures or outcomes other than those determined in the inclusion criteria, (ii) review studies, clinical protocols, case reports, and (iii) studies published in the form of book chapters, conference abstracts, letters to the editor, or editorials.
For the qualitative analysis, the following information was extracted from the studies: authors, year of publication, country where the research was conducted, study design, quantification of the exposed population, type of cannabis exposure, main results, and conclusions.
The risk of bias was assessed using the critical appraisal tools recommended by The Joanna Briggs Institute (JBI), using the checklist for cohort studies, cross-sectional studies, and case-control studies.
9 These classifications were not used as criteria for excluding studies.
ResultsA total of nine studies were included in this systematic review. Of these, five (55.6%) were published in the last five years. It should be noted that 66.7% of the studies were conducted in the United States, and none of them evaluated data from developing countries. Table 1 summarizes the characteristics of these studies.
In the studies included in the systematic review, the method of assessing cannabis exposure varied, with the use of interviews, medical records, and toxicological testing. There was also variation in the timing of exposure, with the possibility of use at conception, during pregnancy, or in the postnatal period. Information on frequency, dose, and route of use was not available in the studies analyzed. Only two studies assessed parental cannabis use. The use of medical cannabis was not addressed by any of the researches.
Regarding to the outcome of SIDS death, the studies mainly used information from autopsy reports or medical records. The number of SIDS deaths evaluated in each study ranged from four to 1,549. Altogether, the studies included in the systematic review evaluated 3,132 SIDS deaths.
A statistical analysis specifically correlating SIDS with cannabis use was available in seven of the nine studies included. In four of these seven studies, the results suggested an association between exposure and outcome. In the other three studies, although a trend toward association was suggested, the confidence intervals did not allow confirmation.
Table 2 shows the results of the risk of bias analysis of the studies included in the systematic review. It can be observed that the studies included in the review met most of the requirements for a lower risk of bias, according to the assessment scales used.
DiscussionBased on the analysis of the studies selected in this systematic review, it was demonstrated that most of the available literature presented results suggesting a correlation between parental cannabis use and SIDS.
Given the increasing legalization of cannabis in the Western world, its use is becoming more prevalent each year, involving women of childbearing age and, consequently, pregnant women.
18 Data from the 2016 and 2017 US National Surveys of Drug Use and Health showed that 12% of the pregnant women in their first trimester and about 4% in their second and third trimesters reported using cannabis in the past 30 days.
18In the same survey, 20% of the pregnant women who reported cannabis use met the criteria for drug dependency.
19Tetrahydrocannabinol (THC), the main psychoactive component of cannabis, is lipophilic and easily crosses the placenta, where it can accumulate in the fetus.
20 Studies suggest that prenatal exposure to THC can disrupt the endocannabinoid system, which is crucial for placental implantation and fetal development.
20 A 2022 meta-analysis associated cannabis use during pregnancy with a 61% increase in the risk of small babies for gestational age, a 106% increase in the risk of low birth weight, a 28% increase in the risk of premature birth, and a 38% increase in the risk of admission to a neonatal intensive care unit.
21Considering the specific relationship between perinatal cannabis use and the risk of SIDS, the study by Bandoli et al.
14 showed that a diagnosis related to cannabis use during pregnancy conferred a 2.7-fold increased risk of SIDS, including adjustment for maternal nicotine use.
14 The results of a new research by the same group in 2023 showed that the incidence of infant death in the first year of life was higher among those diagnosed with maternal cannabis use disorder compared to those without this diagnosis.
17A French study evaluated the postmortem toxicological analysis of 398 cases of infants who died of SIDS between 2015 and 2018. The main substances isolated were illicit drugs (43%), with cannabis and opiates being the main drugs identified.
13 However, specific statistics for cannabis alone were not reported, preventing conclusions about this possible association. Similarly, the study by Rosen and Johnson
10 did not evaluate cannabis individually, but in only one of the SIDS cases analyzed, the infant was the child of a mother with a history of marijuana use and mild alcohol abuse.
10Klonoff-Cohen and Lam-Kruglick study
12 was the only one selected to analyze the influence of paternal cannabis use on SIDS, highlighting that the role of paternal use of psychoactive drugs is an understudied area. Paternal cannabis use during conception, pregnancy, and the postnatal period, considering smoking in the presence of or near the baby, was significantly associated with SIDS in univariate and multivariate analyses. According to the authors, this result can be attributed to the higher prevalence of men who smoke cannabis compared to women, as well as the greater amount, frequency, and duration of use among men.
12Another research, conducted in the United States in 2021, concluded that the use of alcohol, cocaine, and cannabis during pregnancy increases the risk of SIDS, with maternal cannabis use during pregnancy increasing the risk of SIDS fivefold.
15 However, cannabis use became insignificant in the multivariate model, considering sociodemographic variables.
15In contrast, other studies analyzed
11,13 showed that the relationship between parental cannabis use and SIDS may not be so direct, presenting other correlated factors that must be taken into account. A research conducted in New Zealand showed that recent cannabis use by caregivers, when considered in isolation, was not statistically significantly associated with SIDS.
16 However, exposure to potentially correlated risk factors, such as sleeping on the couch or recent use of alcohol and/or other drugs by caregivers, was associated with a significantly increased risk of SIDS.
16Ostrea
et al.
11 evaluated 2,964 infants in the United States at birth for exposure to various drugs through meconium analysis. However, mortality rates in the drug-positive group, specifically including cannabinoids, were not significantly different from those in the drug-negative groups.
11 In contrast, another study in New Zealand found a strong relationship between cannabis use since birth and SIDS. However, after adjusting for ethnicity and smoking, the main associations with cannabis use, the risk fell to 1.73, and to 1.47 with all confounding factors, remaining significant.
5 However, the results suggest that cannabis is a weak risk factor for SIDS, and that the risk associated with frequent cannabis use (weekly or more) by mothers is similar to that of tobacco (daily) and equally influenced by sociodemographic factors.
5The AAP notes in its recommendations that parents who use illicit substances become less vigilant, which prevents them from promptly noticing situations that pose a risk to their child and reduces their ability to wake up in an emergency. The risk is even greater in situations of bed sharing, where impaired alertness can lead to serious incidents, such as accidental suffocation when rolling over on the child.
6 In addition, these parents may fall asleep with the infant in their arms, increasing the risk of falls and suffocation. Impaired lucidity caused by substance use also predisposes parents to situations of negligence, such as leaving objects near the baby's face, positioning the baby improperly for sleep, or overheating the child, all of which are factors that can lead to suffocation or other fatal risks.
6The review identified important limitations in the available studies: geographic bias due to the predominance of research in developed countries; use of inaccurate indicators of cannabis exposure, often based only on maternal diagnostic codes; wide variation in how consumption is measured (frequency, intensity, route of use), without considering oral intake or postnatal exposure through breast milk; and inconsistencies in the classification of consumption frequency, which reduces comparability between studies.
Final considerationsOverall, the studies analyzed in this systematic review suggest a possible association between cannabis use and the risk of SIDS. However, the limitations of this review highlight the need for more comprehensive studies on the isolated use of cannabis by mothers and fathers and its relationship with SIDS, with more accurate data on frequency, intensity, and route of use. Most studies focus on developed countries and lack adequate analysis of socioeconomic variables that influence the results. Therefore, future studies are needed to explore the mechanisms underlying cannabis use during pregnancy and postpartum, by both mothers and fathers, to establish a more accurate correlation with SIDS. These studies should replicate the findings in new contexts and identify mediating variables in the causal pathway between cannabis use and infant mortality. In addition, it is imperative to develop effective interventions to treat cannabis use disorder during pregnancy, as well as to implement national recommendations for investigative examinations in light of the national infant mortality registry. This will contribute to a better understanding and mitigation of the risks associated with parental cannabis use and SIDS.
References1. Wojcik MH, Krous HF, Goldstein RD. Sudden Unexplained Death in Childhood: Current Understanding. Pediatr Emerg Care. 2023 Dec; 39 (12): 984-5.
2. Braga GGS, Martelli ABS, Gomes CB, Gianoto NR, Cardoso IK. Síndrome da morte súbita infantil: um estudo da prevalência nas regiões brasileiras dos anos de 2015 a 2020, associação com os fatores de risco e formas de prevenção. Revista Ibero-Americana De Humanidades, Ciênc Educ. 2024 Jan; 10 (1): 155-67.
3. Trachtenberg FL, Haas EA, Kinney HC, Stanley C, Krous HF. Risk Factor Changes for Sudden Infant Death Syndrome After Initiation of Back-to-Sleep Campaign. Pediatrics. 2012 Apr; 129 (4): 630-8.
4. Solmi M, De Toffol M, Kim JY, Choi MJ, Stubbs B, Thompson T,
et al. Balancing risks and benefits of cannabis use: umbrella review of meta-analyses of randomised controlled trials and observational studies. BMJ. 2023 Aug; 382: e072348.
5. Scragg RK, Mitchell EA, Ford RP, Thompson JM, Taylor BJ, Stewart AW. Maternal cannabis use in the sudden death syndrome. Acta Paediatr. 2001 Jan; 90 (1): 57-60.
6. Moon RY, Carlin RF, Hand I; AAP Task Force on Sudden Infant Death Syndrome; AAP Committee on Fetus and Newborn. Sleep-Related Infant Deaths: Updated 2022 Recommendations for Reducing Infant Deaths in the Sleep Environment. Pediatrics. 2022 Jul; 150 (1): e2022057990.
7. Shu JE, Huang H, Menezes PR, Faisal-Cury A. Prevalence and risk factors for cannabis use in low-income pregnant women in São Paulo, Brazil. Arch Womens Ment Health. 2016 Feb; 19: 193-6.
8. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for Systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul; 6: e1000097.
9. Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editors. JBI Manual for Evidence Synthesis. JBI; 2024. [
Internet]. [access in 2024 Jun 21]. Available from:
https://synthesismanual.jbi.global10. Rosen TS, Johnson HL. Drug-addicted mothers, their infants, and SIDS. Ann N Y Acad Sci. 1988; 533: 89-95.
11. Ostrea EM Jr, Ostrea AR, Simpson PM. Mortality within the first 2 years in infants exposed to cocaine, opiate, or cannabinoid during gestation. Pediatrics. 1997 Jul; 100 (1): 79-83.
12. Klonoff-Cohen H, Lam-Kruglick P. Maternal and paternal recreational drug use and sudden infant death syndrome. Arch Pediatr Adolesc Med. 2001 Jul; 155 (7): 765-70.
13. Claudet I, Visme S, Duthoit G, Barnet L, Marchand-Tonel C, Chever M,
et al; OMIN Study Group. Prevalence of positive toxicology analysis from the French national registry for sudden unexpected infant death (Tox-MIN). Clin Toxicol (Phila). 2022 Jan; 60 (1): 38-45.
14. Bandoli G, Baer RJ, Owen M, Kiernan E, Jelliffe-Pawlowski L, Kingsmore S,
et al. Maternal, infant, and environmental risk factors for sudden unexpected infant deaths: results from a large, administrative cohort. J Matern Fetal Neonatal Med. 2022 Dec; 35 (25): 8998-9005.
15. Hauck FR, Blackstone SR. Maternal Smoking, Alcohol and Recreational Drug Use and the Risk of SIDS Among a US Urban Black Population. Front Pediatr. 2022 May; 10: 809966.
16. MacFarlane ME, Thompson JMD, Wilson J, Lawton B, Taylor B, Elder DE,
et al. Infant Sleep Hazards and the Risk of Sudden Unexpected Death in Infancy. J Pediatr. 2022 Jun; 245: 56-64.
17. Bandoli G, Delker E, Schumacher BT, Baer RJ, Kelly AE, Chambers CD. Prenatal cannabis use disorder and infant hospitalization and death in the first year of life. Drug Alcohol Depend. 2023 Jan; 242: 109728.
18. Volkow ND, Han B, Compton WM, McCance-Katz EF. Self-reported Medical and Nonmedical Cannabis Use Among Pregnant Women in the United States. JAMA. 2019 Jul; 322 (2): 167-9.
19. Alshaarawy O, Anthony JC. Cannabis use among women of reproductive age in the United States: 2002-2017. Addict Behav. 2019 Dec; 99: 106082.
20. Gesterling L, Bradford H. Cannabis Use in Pregnancy: A State of the Science Review. J Midwifery Womens Health. 2022 May; 67 (3): 305-13.
21. Marchand G, Masoud AT, Govindan M, Ware K, King A, Ruther S,
et al. Birth Outcomes of Neonates Exposed to Marijuana in Utero: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022 Jan; 5 (1): e2145653.
Authors' contributionsBignoto LLC, Fernandes PC, Bastida ACF: data extraction, writing of the original draft.
Alvim VF: coordination of the research, final writing of the manuscript.
Grunewald STF: research design and coordination, data analysis, final manuscript writing.
All authors approved the final version of the article and declare no conflict of interest.
Data availabilityThe entire dataset supporting the results of this study has been published in the article itself.
Received on August 13, 2024
Final version presented on September 15, 2025
Approved on September 16, 2025
Associated Editor: Karla Bomfim
 ; Paula da Costa Fernandes2
; Paula da Costa Fernandes2 ; Ana Cecília Finamore Bastida3
; Ana Cecília Finamore Bastida3 ; Vitor Fernandes Alvim4
; Vitor Fernandes Alvim4 ; Sabrine Teixeira Ferraz Grunewald5
; Sabrine Teixeira Ferraz Grunewald5