ABSTRACT
OBJECTIVES: to analyze the correlation between oral stimulation, the sucking pattern and feeding performance of premature newborns.
METHODS: systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement guidelines. The databases consulted included PubMed-Central, Cielo, LILACS, and via EBSCOHost, with no temporal or language restrictions. The research process was carried out from October to November 2023. The selection, screening, and integration of studies were conducted using the Rayyan® software, in collaboration with another researcher. Evidence analysis was performed using the Quality Assessment Tool for Quantitative Studies instrument.
RESULTS: 358 articles were found, of which 13 were selected after eliminating duplicates and application of the qualification criteria. Three additional articles were included through reference analysis, totaling a sample of 16 original studies. Evidence levels varied, with one study classified as weak, three as moderate, and twelve as strong. The results obtained demonstrated that oral stimulation improved the sucking pattern and feeding performance, contributing to early hospital discharge.
CONCLUSION: the literature supports that oral stimulation techniques, non-nutritive sucking and Premature Infant Oral Motor Intervention have beneficial effects on the premature newborns' feeding process.
Keywords:
Infant premature, Feeding methods, Sucking, Sucking behavior, Deglutition
RESUMO
OBJETIVOS: analisar a relação entre a estimulação oral, o padrão de sucção e o desempenho alimentar de recém-nascidos prematuros.
MÉTODOS: revisão sistemática seguindo as diretrizes do Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement. Foram consultadas as bases PubMed-Central, SciELO, LILACS e CINA-HL Complete, Cochrane Collection Plus, Nursing & Allied Health Collection e Medic Latina via EBSCOHost, sem restrições temporais ou de idioma. A pesquisa foi realizada entre outubro a novembro de 2023. O processo de seleção, triagem e integração dos estudos foi conduzido no programa Rayyan®, em colaboração com outro pesquisador. A análise de evidências foi feita através do instrumento Quality Assessment Tool For Quantitative Studies.
RESULTADOS: foram encontrados 358 artigos, dos quai 13 foram selecionados após eliminação de duplicados e aplicação dos critérios de qualificação. Três artigos adicionais foram incluídos pela análise de referências, totalizando uma amostra de 16 estudos originais. O nível de evidência variou de fraco (n=1), moderado (n=3) e forte (n=12). Os resultados obtidos demonstraram que a estimulação oral melhorou o padrão de sucção, o desempenho alimentar e contribuiu para alta hospitalar precoce.
CONCLUSÃO: a literatura apoia que técnicas de estimulação oral, sucção não nutritiva e a Premature Infant Oral Motor Intervention têm efeitos benéficos no processo alimentar de recém-nascidos prematuros.
Palavras-chave:
Recém-nascido prematuro, Métodos de alimentação, Sucção, Comportamento de sucção, Deglutição
IntroductionPrematurity refers to all live newborns who are younger than 37 weeks.
1 A premature newborn has an underdeveloped nervous system as a result of neurological immaturity, and for this reason, changes in the coordination of the sucking-swallowing-breathing pattern.
2 As the sucking pattern is usually reduced, oral motor skills will be compromised and consequently oral feeding can become challenging for these children.
2It is important to note that clinical practice has shown that premature infants do not suddenly start sucking efficiently, and there is a need for preparation and training so that their sucking and swallowing patterns become coordinated. This training period must be constantly evaluated and stimulated, with the aim of preparing the newborn for more robust and effective sucking.
3 The proper coordination of sucking, swallowing and breathing is a determining factor in ensuring safe feeding. Compromising any of these three functions can put the newborn at risk, specifically aspiration, pneumonia, oxygen desaturation, apnea and bradycardia.
4Due to the use of an alternative feeding route, these newborns often present difficulties and alterations in oro-motor functions, hindering the safe and efficient transition to the oral route.
5The stimulation for nutritive and non-nutritive sucking are forms of oral sensorimotor stimulation. The framework for their use is related to the development of the phonoarticulatory organs, which occurs due to the occurrence of muscular pressure during the babies' sucking function.
6 By performing nutritive or non-nutritive sucking, the newborn will be developing the phonoarticulatory organs properly, thus promoting the correct functioning of the oromotor structures due to the relationship that exists between the stomatognathic system and the other organs and functions.
7The technique of non-nutritive sucking with the gloved little finger
8 is one of the most common routine in the neonatal intensive care units, followed by non-nutritive sucking with a pacifier.
8 This technique can be used alone or combined with other strategies in specific intervention programs.
The oral stimulation program
9 can be implemented for this purpose. This program includes 15 minutes of intervention, in which the first 12 minutes consist of stimulating the cheeks, lips, gums and tongue, and the last three minutes consist of non-nutritive sucking on a pacifier commonly used in the nursery.
9 Oral sensorimotor stimulation in premature newborns accelerates the maturation process of oral reflexes, helping to develop the ability to feed orally in a safe and effective way.
10In particular, the Premature Infant Oral Motor Intervention (PIOMI) is an oral stimulation program created by Lessen
11 that provides (i) assisted movements to activate muscle contraction of the phonoarticulatory organs (ii) against resistance to increase strength.
11 Given the difficulties that prematurity brings, it is important to understand how different techniques can facilitate the feeding pattern on premature newborns, since it is essential for them to be able to make the feeding transition in a safe and effective way.
Therefore this study aims to examine the effects of oral stimulation on the feeding performance of premature newborns. The aim is to analyze the relationship among oral stimulation, the sucking pattern and the feeding performance of these newborns.
MethodsThis study is of a methodological nature and consists of a systematic review of the literature that aims to analyze the importance of oral stimulation in the performance of the premature newborns' on feeding pattern and sucking. This review has been registered on the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) under the registration number INPLASY2024100083.
The question of the present study was carried out in PICO format, i.e. Population (P), Intervention (I), Comparator (C) and Outcome (O), considering the question: "What is the importance of oral stimulation (I) compared to the standard procedure (C) in the feeding performance (O) of preterm newborns (P)?". In particular, for the outcome under study (i.e. feeding performance), measures of i) milk transfer rate, ii) overall milk intake volume, iii) feeding performance/sucking pattern, iv) oral feeding initiation time, v) independent oral feeding, vi) effective breastfeeding and vii) early hospital discharge were analyzed.
Eligibility criteria were established for this study, as follows. Regarding the inclusion criteria, primary studies were included with premature newborns who presented feeding difficulties, born between 25-36 weeks of gestation who were stable and did not require mechanical ventilation, subject to oral stimulation programs and non-nutritive sucking. Articles duplicated in the database, letters to the editor, gray literature articles, case reports, secondary reports, studies integrating newborns with primary diagnoses and studies that did not answer the research question were excluded. Articles were not excluded based on the level of evidence.
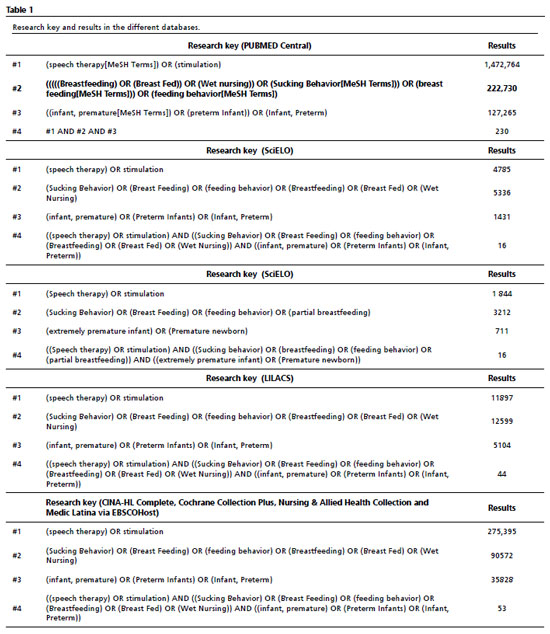
The search for the present investigation was carried out by two independent researchers through the PubMed Central, SciELO, LILACS databases and a search of the following databases through the EBSCOHost platform: CINA-HL Complete, Cochrane Collection Plus, Nursing & Allied Health Collection and Medic Latina. No time or language restrictions were set. The specific descriptors and search keys for each database are shown in Table 1. Four key terms were used for the search key: speech therapy, premature newborns and sucking pattern. The Medical Subject Headings (MeSH term) "speech therapy" and the natural language term "stimulation" were used for the concept "speech therapy". For "premature newborns", the MeSH term "infant, premature" and the natural language terms "preterm infant" and "infant, preterm" were used. For "sucking pattern", the MeSH terms "sucking behavior", "breast feeding", "feeding behavior" and the natural language terms "breastfeeding", "breast fed" and "wet nursing" were used. The descriptors were combined with Boolean operators AND and OR and proximity operators "" and (). To increase comprehensiveness during the search, no filters were used in the databases (e.g. time period of publication, type of study).
Following the literature search, it was necessary to remove duplicates and assess the titles and abstracts of the remaining results, in order to judge whether they should be included. At this stage, the program Rayyan
Ò was used,
12 thus facilitating the organization of the studies and the screening process. This selection was carried out independently by two researchers. Studies that met the inclusion criteria were selected and those that did not fit the topic under study were removed after reading the titles and abstracts. This program also made it possible to obtain basic bibliometric information, helping to reduce bias among researchers, attach full texts, resolve duplicates and justify the exclusion of studies through labeling.
12 In the event of non-consensus, the collaboration of a third researcher was predicted.
Once all the studies that met the previously defined criteria had been included, their bibliographic references were consulted in order to examine possible additional sources of information that had not been detected in the initial search. Subsequently, the studies selected after a consensus meeting were read in full by a researcher and a detailed analysis was carried out.
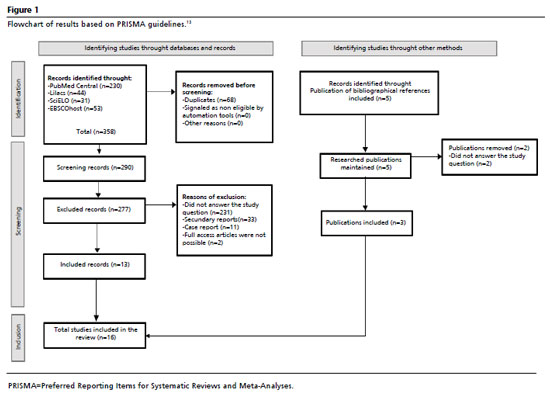
The selection of studies was described in a flowchart, following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA)
13 (Appendix 1). The evidence analysis was carried out for each study according to the Quality Assessment Tool For Quantitative Studies.
14 This tool allows the final classification of the quality of studies by assigning sub-classifications (strong, moderate or weak) to a set of six topics: sample representativeness, study design, confounding factors, blinding, data collection and retention (dropouts). An overall classification was determined based on the sub-classifications assigned: strong if there were no weak sub-classifications; moderate if there was one weak sub-classification; weak if there were more than two weak sub-classifications.
14 The results obtained are organized in Table 2, which includes the reference of each one, the types of study, the population, the methodology, the results, the conclusions and the evidence analysis.
14 Table 3 organizes the different outcomes studied at the end of each investigation.
ResultsFigure 1 shows the flowchart that integrates the process of integrating the studies for the present investigation, which contains information on the process of identifying and screening studies. It also shows the reasons for excluding records. The results of the search in the different databases (n=358) were imported into the program Rayyan
Ò. Secondary reports (n=33), case reports (n=11) and those that did not answer the study question (n=231) were then excluded, with the titles first being analyzed and, if there were any doubts, the abstract. Articles which could not be accessed in full were also excluded (n=2). The researchers of these studies were contacted, but no reply was received. As a result, 13 studies were integrated and three were added by analyzing the bibliographical references of the studies already selected, giving a total of 16 articles as a sample of original studies. When the sample of original studies was reviewed with a second researcher, there was total consensus and agreement.
Of the 16 studies analyzed, one had a weak level of evidence, three had a moderate level of evidence and 12 were classified as having a strong level of evidence. The evidence analysis is present in all the columns of Table 1. All the integrated studies made comparisons with control groups that were made up of sham (simulated procedures) or standard neonatal care, which refers to the set of practices and interventions carried out to promote the health and well-being of newborns. This care includes medical assistance, monitoring and support for newborns, focusing on the prevention, early diagnosis and treatment of conditions that may threaten their life or development.
The 16 studies selected for this investigation date from between 2002 and 2022, with the majority originating from the United States (Fucile
et al.
9; Fucile
et al.
15; Lessen
11; Fucile
et al.
16), with some from Brazil (Rocha
et al.,
17 Costa
et al.
18), India (Arora
et al.
19; Thakkar
et al.,
20; Kore and Mathew
21), Iran (Ghomi
et al.
22; Mahmoodi
et al.
23; Ostadi
et al.
24), Luxembourg (Bache
et al.
25), China (Lyu
et al.
26), Thailand (Lessen
et al.,
27), and Spain (Aguilar-Rodríguez
et al.
28).
As mentioned above, in order to better organize the integrated studies and the results, three tables were drawn up: Table 1 contains the different results of each study and Table 2 presents a compilation of the outcomes studied in all the articles analyzed.
DiscussionConsidering that this study aimed to study the importance of oral stimulation in the sucking/feeding process of premature newborns, it should be noted that the vast majority of the articles included showed that the oral stimulation program,
10 non-nutritive sucking
8 and PIOMI
11 had a beneficial effect not only on the feeding performance of premature newborns, but also on independent oral feeding. The studies by Fucile
et al.,
9 Fucile
et al.,
15 Rocha
et al.,
17 and Lyu
et al.
26 showed positive effects through the oral stimulation program
10 and non-nutritive sucking. With the intervention of the oral stimulation program alone, the studies by Bache
et al.,
25 Fucile
et al.,
16 Aguilar-Rodríguez
et al.,
28 and Kore and Mathew
21 proved that the application of this program brings benefits to premature newborns. Through the implementation of PIOMI, the studies by Lessen,
11 Arora
et al.,
19 Thakkar
et al.,
20 Ghomi
et al.,
22 Lessen
et al.,
27 and Mahmoodi
et al.,
23 demonstrated significant improvements with the use of this program. When interpreting the results of the studies analyzed, more outcomes were visible that are directly related to the programs under study. Thus, in addition to the outcomes initially studied (i.e. improved feeding performance and feeding independence of premature babies), the rate and volume of milk ingested, time to first feeding, breastfeeding rate and early hospital discharge were also analyzed. Therefore, these outcomes will be considered for this discussion.
i)Milk transfer rateWith regard to the milk transfer rate (i.e. the volume of milk ingested in relation to the duration of oral feeding session), one of the results found in the studies by Fucile
et al.,
9 Fucile
et al.,
15 showed that the oral stimulation program and non-nutritive sucking had a beneficial effect, causing these newborns to have a higher milk transfer rate precisely because of the improved sucking pattern. On the other hand, in the studies by Costa
et al.,
18 Lyu
et al.
26 and Thakkar
et al.,
20 this same effect could not be observed and there was no increase in the milk transfer rate. Regarding this relationship, the literature has shown that there is an increase in the rate of milk transfer in newborns who undergo an oral stimulation program, suggesting that these babies are better able to suck more effectively.
29 These findings are congruent with the studies by Fucile
et al.,
9 Fucile
et al.,
15 which point to a benefit of these techniques.
ii)Volume of milk swallowedRegarding the increase in the volume of milk swallowed (i.e. the volume consumed as a percentage of the prescribed volume) by premature newborns, the studies by Fucile
et al.,
9 Fucile
et al.,
15 Thakkar
et al.,
20 and Lessen
et al.,
27 showed favorable results, with a greater amount of milk volume swallowed by babies who received the stimulation program. However, the study by Costa
et al.
18 did not show any changes in the volume of milk swallowed by the babies, which may be due to the fact that the experimental group weighed less at the different assessment times than the control group. The literature also attests to the positive relationship between the oral stimulation program and the increase in the volume of milk swallowed by these newborns, which is justified by the improvement in the sucking pattern, allowing the babies to swallow more milk due to stronger and more effective sucking.
30 This is in line with the studies by Fucile
et al.,
9 Fucile
et al.,
15 Thakkar
et al.,
20 and Lessen
et al.,
27 analyzed in this study.
iii)Feeding performance/sucking patternWith regard to feeding performance/sucking pattern, one of the outcomes to be studied in this study, the studies by Fucile
et al.,
9 Fucile
et al.,
15 Rocha
et al.,
17 Bache
et al.,
25 Lyu
et al.,
26 Arora
et al.,
19 Thakkar
et al.,
20 Ghomi
et al.,
22 Lessen
et al.,
27 Ostadi
et al.
24 and Kore and Mathew
21 have shown that an oral stimulation program has promising results in relation to the feeding performance and sucking pattern of premature babies. According to the information found in other studies, it was possible to conclude that the feeding performance of these babies improved because the techniques used helped to coordinate the sucking-breathing-deglutition pattern during the different sucks, providing a maturation of the different structures.
31 This information is in line with the results obtained in the studies by Fucile
et al.,
9 Fucile
et al.,
15 Rocha
et al.,
17 Bache
et al.,
25 Lyu
et al.,
26 Arora
et al.,
19 Thakkar
et al.,
20 Ghomi
et al.,
22 Lessen
et al.,
27 Ostadi
et al.
24 and Kore and Mathew
21 demonstrating that the stimulation program effectively shows beneficial results in relation to the feeding performance of these premature infants.
iv)Time to start oral feedingWith regard to the time taken to start oral feeding, the studies by Rocha
et al.,
17 Ghomi
et al.,
22 Lessen
et al.,
27 Mahmoodi et al.
23 and Aguilar-Rodríguez
et al.
28 and Ostadi
et al.
24 showed that the stimulation program reduced the time normally required for premature newborns to start oral feeding. This information is in line with the results found in the literature, in particular in the study by Neiva and Leone
32 which aimed to investigate and analyze the effects of non-nutritive sucking stimulation on the age of onset of oral feeding in premature newborns, and showed that this technique accelerated the process of starting the first oral feeding. These results are similar to those obtained in the studies by Rocha
et al.,
17 Ghomi
et al.,
22 Lessen
et al.,
27 Mahmoodi
et al.,
23 Aguilar-Rodríguez
et al.
28 and Ostadi
et al.,
24 which show that the stimulation program plays an important role in anticipating the first oral feeding of premature babies without the presence of a feeding tube.
v)Independent oral feedingIndependent oral feeding was studied by the authors Fucile
et al.,
9 Fucile
et al.,
15 Rocha
et al.,
17 Costa
et al.,
18 Lessen,
11 Bache
et al.,
25 Lyu
et al.,
26 Fucile
et al.,
16 Thakkar
et al.,
20 Ghomi
et al.,
22 Mahmoodi
et al.
23 and Aguilar-Rodríguez
et al.
28 who obtained the results of earlier total oral feeding by premature newborns who benefited from the stimulation program. However, Costa
et al.
18 and Bache
et al.
25 who also studied this factor, obtained different results, and there were no differences in the time needed to transition from tube feeding to independent oral feeding. According to the literature, as can be seen in the study by Pereira
et al.
33 which aimed to assess the effect of the oral stimulation program on oral feeding performance and the transition time from the tube to total oral intake, this program showed important results with regard to the time needed to make the transition from the tube to independent oral feeding, with a reduction in time having been demonstrated in this study. In this way, the studies by Fucile
et al.,
9 Fucile
et al.,
15 Rocha
et al.,
17 Lessen,
11 Lyu
et al.,
26 Fucile
et al.,
16 Thakkar
et al.,
20 Ghomi
et al.,
22 Mahmoodi
et al.,
23 and Aguilar-Rodríguez
et al.
28 are supported by the results obtained in the research by Pereira
et al.
33 in which the oral stimulation program revealed that babies who were submitted to this technique showed a reduction in the transition time between the feeding tube and independent oral feeding. This may be related to the improvement in the sucking pattern of premature newborns which, because it is more efficient, allows babies to make the transition from the feeding tube to independent oral feeding sooner.
vi)Breastfeeding ratesWith regard to breastfeeding rates, Bache
et al.
25 and Fucile
et al.
16 found that the oral stimulation program helped to improve breastfeeding rates. In this context, the study by Balci
et al.
34 which aimed to understand the benefits of oromotor stimulation in relation to the transition to breastfeeding, concluded that the oral stimulation program has beneficial effects on feeding skills and the transition to breastfeeding in premature newborns. These data are in line with the results obtained in the studies by Bache
et al.
25 and Fucile
et al.,
16 demonstrating once again that oral stimulation of babies provides a number of benefits.
vii) Early hospital dischargeEarly hospital discharge was one of the outcomes studied in the different studies analyzed in this investigation. It should be noted that this result is linked to the different results studied so far, since hospital discharge is directly related to oral feeding independence and also to feeding performance.In this way, different authors have studied this factor, Rocha
et al.,
17 Arora
et al.,
19 Fucile
et al.,
16 Thakkar
et al.,
20 Ghomi
et al.,
22 Mahmoodi
et al.
23 and Aguilar-Rodríguez
et al.
28 showing that the oral stimulation program has positive effects on hospital discharge, and where the newborns studied were discharged earlier than those who were not subjected to this technique. Authors such as Song
et al.
35 reported that newborns who had the oral stimulation program as an intervention had fewer days in hospital than the control group who did not have any type of intervention. However, in the studies by Fucile
et al.,
9 Bache
et al.
25 and Lyu
et al.
26 the same results were not found, showing that babies who underwent the oral stimulation program had no differences in the length of stay until hospital discharge. These results may be due to the fact that the experimental group studied had a lower birth weight, which may have biased the effects.According to Medeiros
et al.,
36 more premature newborns with lower birth weights stay in hospital longer because they need more care and specific interventions.
Thus, after analyzing the results and comparing them with the literature, we can highlight a beneficial effect of the oral stimulation program in improving the feeding performance of premature newborns and the early transition between tube and total oral feeding, information that answers the initial question of this research. Newborns submitted to this program show improvements related to feeding, which is decisive for their development and growth.
Study limitationsIt is important to recognize some limitations regarding this work, especially those inherent to primary studies. Some methodological weaknesses (i.e. small samples, variability in the type of control group) influenced the analysis of the evidence. In addition, there were difficulties related to the heterogeneity of the studies which made it difficult to synthesize the data, especially as the analysis measures varied significantly. As an example of this factor, it can be seen that the sample size varied from 19 to 112 premature newborns and their characteristics were not homogeneous, namely in terms of gestational age and birth weight. Another limitation observed was the time and frequency of administration of the different stimulation techniques. In some studies it was administered for five minutes once a day, while in others it was administered more times a day. In some studies, the intervention was carried out for seven days, while in others, it was prolonged until the baby began to feed himself or herself orally. It should also be noted that when interpreting the outcomes of the studies, the technique used was not always the same, and it was possible to verify the use of oral stimulation, PIOMI and non-nutritive sucking. This heterogeneity made it difficult to carry out a more comprehensive analysis and generalize the results found. There were no studies excluded because they were in a language not mastered by the researchers, so it is considered that there was no risk of language bias.
ConclusionThe literature supports the notion that oral sensorimotor stimulation has beneficial effects on the feeding process of premature newborns. This study underlines its relevance to clinical practice by demonstrating that oral sensorimotor stimulation is associated with an improvement in feeding patterns and promotes autonomy in newborns, which supports the recommendation to implement it in neonatal units. In addition, the results indicate a trend towards a reduction in the length of stay, which could contribute to a reduction in the costs associated with managing neonatal care services. The combination of different techniques could enhance the therapeutic effect in terms of the feeding transition, but more studies are needed to consolidate this statement.
References1. World Health Organization (WHO). Who: Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Acta Obstet Gynecol Scand. 1977 Jan; 56 (3): 247-53.
2. Denucci MAM, Williams EMO, Badoca MEG, Souza CHM. Atuação fonoaudiológica na amamentação: aspectos sobre a prematuridade / Speech-language pathology action in breastfeeding: aspects about prematurity. Braz J Dev. 2021 Ago; 7 (8): 82123–36.
3. Caetano LC, Fujinaga CI, Scochi CGS. Sucção não nutritiva em bebês prematuros: estudo bibliográfico. Rev Lat Am Enfermagem. 2003 Mar; 11 (2): 232-6.
4. Lau C, Hurst N. Oral feeding in infants. Curr Probl Pediatr. 1999 Abr; 29 (4): 105-24.
5. Bauer MA, Prade LS, Keske-Soares M, Haëffner LSB, Weinmann ARM. The oral motor capacity and feeding performance of preterm newborns at the time of transition to oral feeding. Braz J Med Biol Res. 2008 Out; 41 (10): 904-7.
6. Severino AD, Caricilli BB, Borges MC, Magosso WR, Ribeiro JPQS, Franco RC,
et al. Importância do aleitamento materno para o amadurecimento dos órgãos fonoarticulatórios: uma revisão literária / Importance of breastfeeding for the maturation of phonoarticulatory bodies: a literary review. Braz J Dev. 2021 Jun; 7 (5): 48282–93.7.
7. Bernardo GMB, Gonçalves LF, Haas P, Blanco-Dutra AP. Relação entre aleitamento e desenvolvimento do sistema estomatognático: revisão sistemática. Res Soc Dev. 2021; 10 (11): e499101120011.
8. Lemes EF, Silva THMM, Correr ADMA, Almeida EOCD, Luchesi KF. Estimulação sensoriomotora intra e extra-oral em neonatos prematuros: revisão bibliográfica. Rev CEFAC. 2015 Jun; 17 (3): 945-55.
9. Fucile S, Gisel E, Lau C. Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. J Pediatr. 2002 Ago; 141 (2): 230-6.
10. Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2007 Ago; 97 (1): 61-7.
11. Lessen BS. Effect of the Premature Infant Oral Motor Intervention on Feeding Progression and Length of Stay in Preterm Infants. Adv Neonatal Care. 2011 Abr; 11 (2): 129-39.
12. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan - a web and mobile app for systematic reviews. Syst Rev. 2016 Dez; 5 (1): 210.
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD,
et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar; 372: 71.
14. Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004 Jun; 1 (3): 176-84.
15. Fucile S, Gisel EG, Lau C. Effect of an oral stimulation program on sucking skill maturation of preterm infants. Dev Med Child Neurol. 2005 Mar; 47 (3): 158-62.
16. Fucile S, Milutinov M, Timmons K, Dow K. Oral Sensorimotor Intervention Enhances Breastfeeding Establishment in Preterm Infants. Breastfeed Med. 2018 Set; 13 (7): 473-8.
17. Rocha AD, Moreira MEL, Pimenta HP, Ramos JRM, Lucena SL. A randomized study of the efficacy of sensory-motor-oral stimulation and non-nutritive sucking in very low birthweight infant. Early Hum Dev. 2007 Jun; 83 (6): 385-8.
18. Costa PP, Ruedell AM, Weinmann ÂRM, Keske-Soares M. Influência da estimulação sensório-motora-oral em recém-nascidos pré-termo. Rev CEFAC. 2011; 13 (4): 599-606.
19. Arora K, Goel S, Manerkar S, Konde N, Panchal H, Hegde D,
et al. Prefeeding Oromotor Stimulation Program for Improving Oromotor Function in Preterm Infants — A Randomized Controlled Trial. Indian Pediatr. 2018 Ago; 55 (8): 675-8.
20. Thakkar PA, Rohit HR, Ranjan Das R, Thakkar UP, Singh A. Effect of oral stimulation on feeding performance and weight gain in preterm neonates: a randomised controlled trial. Paediatr Int Child Health. 2018 Aug; 38 (3): 181-6.
21. Kore AM, Mathew S. Effect of oral stimulation on feeding performance of preterm babies. J Pharm Negat Results. 2022 Nov; 13: 1174-80.
22. Ghomi H, Yadegari F, Soleimani F, Knoll BL, Noroozi M, Mazouri A. The effects of premature infant oral motor intervention (PIOMI) on oral feeding of preterm infants: A randomized clinical trial. Int J Pediatr Otorhinolaryngol. 2019 Mai; 120: 202-9.
23. Mahmoodi N, Lessen Knoll B, Keykha R, Jalalodini A, Ghaljaei F. The effect of oral motor intervention on the oral feeding readiness and feeding progression in Preterm Infants. Iran J Neonatol. 2019; 10(3): 58-63.
24. Ostadi M, Jokar F, Armanian AM, Namnabati M, Kazemi Y, Poorjavad M. The effects of swallowing exercise and non-nutritive sucking exercise on oral feeding readiness in preterm infants: A randomized controlled trial. Int J Pediatr Otorhinolaryngol. 2021 Mar; 142: 110602.
25. Bache M, Pizon E, Jacobs J, Vaillant M, Lecomte A. Effects of pre-feeding oral stimulation on oral feeding in preterm infants: A randomized clinical trial. Early Hum Dev. 2014 Mar; 90 (3): 125-9.
26. Lyu T chan, Zhang Y xia, Hu X jing, Cao Y, Ren P, Wang Y jue. The effect of an early oral stimulation program on oral feeding of preterm infants. Int J Nurs Sci. 2014 Mar; 1 (1): 42-7.
27. Lessen BS, Daramas T, Drake V. Randomized Controlled Trial of a Prefeeding Oral Motor Therapy and Its Effect on Feeding Improvement in a Thai NICU. J Obstet Gynecol Neonatal Nurs. 2019 Mar; 48 (2): 176-88.
28. Aguilar-Rodríguez M, León-Castro JC, Álvarez-Cerezo M, Aledón-Andújar N, Escrig-Fernández R, Rodríguez De Dios-Benlloch JL,
et al. The Effectiveness of an Oral Sensorimotor Stimulation Protocol for the Early Achievement of Exclusive Oral Feeding in Premature Infants. A Randomized, Controlled Trial. Phys Occup Ther Pediatr. 2020 Jul; 40 (4): 371-83.
29. Bala P, Kaur R, Mukhopadhyay K, Kaur S. Oromotor stimulation for transition from gavage to full oral feeding in preterm neonates: A Randomized controlled trial. Indian Pediatr. 2016 Jan; 53 (1): 36-8.
30. Neiva FCB, Leone CR. Sucção em recém-nascidos pré-termo e estimulação da sucção. Pró-Fono Rev Atual Cient. 2006 Ago; 18: 141-50.
31. Calado DFB, Souza RD. Intervenção fonoaudiológica em recém-nascido pré-termo: estimulação oromotora e sucção não-nutritiva. Rev CEFAC. 2011 Fev; 14 (1): 176-81.
32. Neiva FCB, Leone CR. Efeitos da estimulação da sucção não-nutritiva na idade de início da alimentação via oral em recém-nascidos pré-termo. Rev Paul Pediatr. 2007 Jun; 25 (2): 129-34.
33. Pereira K, Levy DS, Procianoy RS, Silveira RC. Impact of a pre-feeding oral stimulation program on first feed attempt in preterm infants: Double-blind controlled clinical trial. Allegaert K, editor. Plos One. 2020 Set; 15 (9): e0237915.
34. Balci N, Takci S, Seren HC. Improving feeding skills and transition to breastfeeding in early preterm infants: a randomized controlled trial of oromotor intervention. Front Pediatr. 2023 Set; 11: 1252254.
35. Song D, Jegatheesan P, Nafday S, Ahmad KA, Nedrelow J, Wearden M,
et al. Patterned frequency-modulated oral stimulation in preterm infants: A multicenter randomized controlled trial. Allegaert K, editor. Plos One. 2019 Fev; 14 (2): e0212675.
36. Medeiros AMC, Almeida DMS, Meneses MO, Sá TPLD, Barreto IDDC. Impacto da intervenção fonoaudiológica na introdução de dieta via oral em recém-nascidos de risco. Audiol Commun Res. 2020 Set; 25: e2377.
Authors' contribution: Figueiredo IF: conceptualization, data collection and analysis, research, visualization and writing of the manuscript. Grilo M: supervision, validation and revision of the manuscript. Campos SG: data collection and analysis, revision of the manuscript. Rodrigues IT: project management, methodology, supervision, validation and revision of the manuscript. All the authors have approved the final version of the article and declare no conflict of interest.
Received on April 22, 2024
Final version presented on November 11, 2024
Approved on December 13, 2024
Associated Editor: Raphael Perrier-Melo
ERRATUMIn "
Effect oral stimulation on premature newborns' feeding performance: a systematic review". Rev Bras Saúde Matern Infant. 2025; 25: e20240131, RBSMI corrects authors' affiliations.
In Page 1,
Where it reads: Inês Ferreira Figueiredo
1https://orcid.org/0009-0007-7334-7362
Margarida Grilo
2https://orcid.org/0000-0003-2187-8253
Susana Garcia Campos
3https://orcid.org/0009-0007-0867-3292
Inês Tello Rodrigues
4https://orcid.org/0000-0001-9953-8529
1-4 Escola Superior de Saúde do Alcoitão. Rua Conde Barão, 2649-506. Alcabideche, Portugal. E-mail: ines.f.figueiredo2001@gmail.com
Reading:Inês Ferreira Figueiredo
1https://orcid.org/0009-0007-7334-7362
Margarida Grilo
1https://orcid.org/0000-0003-2187-8253
Susana Garcia Campos
1https://orcid.org/0009-0007-0867-3292
Inês Tello Rodrigues
1,2https://orcid.org/0000-0001-9953-8529
1 Escola Superior de Saúde do Alcoitão. Rua Conde Barão, 2649-506. Alcabideche, Portugal. E-mail: ines.f.figueiredo2001@gmail.com
2 Center for Innovative Care and Health Technology (ciTechcare), IPL Leiria, Portugal.
https://doi.org/10.1590/1806-9304202400000131err-en
 ; Margarida Grilo1
; Margarida Grilo1 ; Susana Garcia Campos1
; Susana Garcia Campos1 ; Inês Tello Rodrigues1,2
; Inês Tello Rodrigues1,2