ABSTRACT
OBJECTIVES: to investigate the effect of oropharyngeal colostrum immunotherapy (OCI) on death incidence in preterm newborns.
METHODS: this is a systematic review with meta-analysis, a study protocol registered in PROSPERO. The databases used were: Lilacs, Pubmed, Web of Science, Portal Capes, Scopus, REBEC and Clinical Trial; and, included studies published from 2007 to 2024, without language limitations. Randomized clinical trials that used OCI in premature infants and had death as an outcome, were selected. The review stages consisted of: protocol production, registration, study eligibility, data extraction, study quality assessment, data synthesis and meta-analysis. The software used was: Rayyan and Stata 10.0.
RESULTS: 15 studies were included for qualitative and quantitative analysis. Regarding the assessment of global risk, the studies were considered to have a high risk of bias. In the quantitative analysis, the sample consisted of 1,497 premature infants; and, the meta-analytic measure showed a difference from the mean of RR=0.750 (95%CI=0.582-0.967), without evidence of heterogeneity between studies I2=0.0%; p=0.649 and positive trend in preventing the incidence of death in the intervention group compared to the control group.
CONCLUSION: the meta-analytic measurement suggests a possible positive effect of OCI in reducing neonatal mortality in premature infants.
Keywords:
Immunotherapy, Colostrum, Premature newborn, Perinatal death, Meta-analysis
RESUMO
OBJETIVOS: investigar o efeito da imunoterapia orofaríngea de colostro (IOC) na incidência de morte em recém-nascido pré-termo.
MÉTODOS: trata-se de uma revisão sistemática com metanálise, com protocolo do estudo registrado no PROSPERO. As bases de dados utilizadas foram: Lilacs, Pubmed, Web of Science, Portal CAPES, Scopus, REBEC e Clinical Trial; e, incluídos estudos publicados de 2007 a 2024, sem limitação de idiomas. Foram selecionados ensaios clínicos randomizados que utilizaram IOC em prematuros e apresentaram como desfecho morte. As etapas da revisão consistiram em: produção do protocolo, registro, elegibilidade dos estudos, extração dos dados, avaliação da qualidade dos estudos, síntese dos dados e metanálise. Os softwares utilizados foram: Rayyan e Stata 10.0.
RESULTADOS: foram incluídos 15 estudos para análise qualitativa e quantitativa. No que concerne a avaliação do risco global, os estudos foram considerados como alto risco de viés. Na análise quantitativa, a amostra foi composta por 1.497 prematuros; e, a medida meta-analítica mostrou uma diferença da média de RR= 0,750 (IC95%= 0,582-0,967, sem evidências de heterogeneidade entre os estudos (I2=0,0%; p=0,649).
CONCLUSÃO: a medida meta-analítica sugere um possível efeito positivo da IOC na redução da mortalidade neonatal de prematuros.
Palavras-chave:
Imunoterapia, Colostro, Recém-nascido prematuro, Morte perinatal, Metanálise
IntroductionPrematurity is defined as birth before 37 completed weeks of gestation and is a sensitive marker on living and health conditions of a population that is considered a public health priority.
1 The World Health Organization has estimated that 152 million children were born prematurely in the last decade worldwide; and in 2020, around 1 million preterm newborns (PTNB) died from prematurity complications.
1 In 2020, 308,702 premature births were recorded in Brazil;
2 of these, 1,416 died of prematurity.
3Over the last few decades, various studies and strategies have been developed to understand and reduce the neonatal mortality rate in the world and in Brazil. One relevant measure is breastfeeding, as in addition to its nutritional characteristics, it contains immunobiological components that play an important role against morbidities and mortality.
4-7 Colostrum, in turn, stands out for its richness in immunomodulatory biofactors, which stimulate the cells of lymphoid tissues and can favor the maturation of the gastrointestinal tract and the immune system, an aspect that is especially relevant for PTNB, as they have immature immune systems and digestive tracts.
4The use of colostrum as immunological therapy - Oropharyngeal colostrum immunotherapy (OCI) - is a clinical practice using raw colostrum in small doses in the oropharynx of premature newborns, especially very low birth weight (VLBW) newborns, for immunological and non-nutritional purposes.
6 OCI is associated with a reduction in necrotizing enterocolitis,
8-11 ventilator-associated pneumonia,
11,12 late-onset sepsis,
10,11 feeding intolerance,
10 time to full enteral feeding,
7,10,11,13 length of hospital stay
9,11,14 and faster recovery of birth weight.
10,13Thus, OCI prevents unfavorable clinical outcomes that contribute to an increase in the mortality rate of PTNBs. However, there is controversy in the literature as to the positive effect of OCI on neonatal mortality.
9,10,15 The current study aimed to investigate the effect of OCI on the death incidence in PTNB, a relevant intervention that prevents health problems in premature infants.
MethodsThis is a systematic review with meta-analysis of studies that evaluated the use of OCI in the death incidence in PTNBs, which followed the recommendations of PRISMA 2020
16 and the "Methodological guidelines: design of systematic review and meta-analysis of randomized clinical trials".
17A search was carried out in the following databases: Cochrane Library, VHL Cochrane Library, Center for Reviews and Dissemination (CRD), Clinical Queries, PubMed and International Prospective Register of Ongoing Systematic Reviews (PROSPERO), to check for registered protocols on the subject. The protocol for this study was self-authored and registered in the PROSPERO international database of systematic reviews, under the number CRD42022313945.
Inclusion and exclusion criteria of the studiesAs eligibility criteria, human studies were considered, clinical trials being randomized, which used OCI in PTNB with gestational age less than 37 weeks, with the incidence of death as the outcome, without language limitation. Studies conducted in animal models and which dealt with colostrum intervention in aspects other than death were excluded. Studies published between 2007 and 2024 were selected in order to identify the first studies published on the subject under investigation.
Selection and eligibility of the studies The databases used were: Lilacs, Pubmed, Web of Science, Portal Capes/MEC, Scopus,
Registro Brasileiro de Ensaios Clínicos (REBEC) and Clinical Trial. The search strategy was constructed by the authors, with keywords, Boolean operators, filters and limiters used in the different electronic databases (Table 1). The selection of studies in journals indexed in the aforementioned databases was carried out until March 20, 2024, and included full texts and abstracts. In addition, during the search, other articles were identified in the list of references of published studies that had already been captured, which met the inclusion criteria and were possibly not captured by the strategies used.
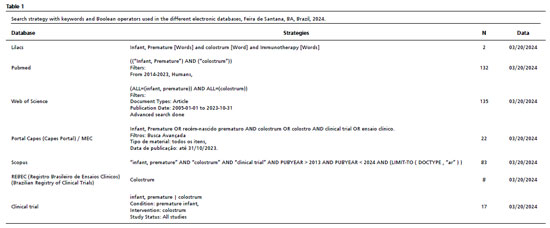
The selection of studies was carried out by two reviewers independently (JRS and CCM), using the combination of descriptors that make up the PICO acronym for this study (P - Preterm newborn, I - OCI, C - Preterm newborn not treated with OCI (delimited by clinical trial) and O - Mortality among preterm infants) (Table 1); and with the help of the Rayyan application to eliminate duplicates and check for agreement between reviewers. The title and abstract were then read to select references and discard those that did not meet the eligibility criteria established for this review. Finally, the two reviewers read the selected articles in full.
For articles not available in the databases, contact was made with the authors; and if the title was suggestive of including the outcome researched, but the abstract was not available, the article remained in the application and moved on to the full text reading phase. If there was disagreement between the reviewers as to the eligibility of the article, a third reviewer (MSXR) was required for the final assessment.
Data extraction and assessment of the quality of the study Data was extracted and consolidated in a structured Excel table with the following information: type of publication, author, year of publication, title of article, objective, method of analysis, results, duration of follow-up, conclusions, journal, journal Qualis, year of research, research funding, type of funding, country of study, continent of study, statistical analysis of studies such as: crude RR,
p-value, adjusted RR. Inclusion and exclusion criteria, sample size, mean age of participants, description of intervention and control, duration of OCI, confounding variables and study outcome.
The methodological quality of the selected studies was assessed using the Cochrane Collaboration's recommended risk-of-bias tool for randomized trials (RoB 2),
18 with regard to potential biases grouped into five domains (risk of bias arising from the randomization process, risk of bias in the blinding of participants and staff regarding allocation or adherence, incompleteness of data regarding outcomes, risk of bias in the evaluation of the outcome measure and risk of selective reporting of outcomes). An overall risk of bias was presented for each domain as: high (when at least one domain was judged to be at high risk of bias), some concern (when at least one domain raised some concern) and low (when all domains were at low risk).
Meta-analysisAll the published studies that met the inclusion criteria were included in the meta-analysis; and, as this is a new topic, there were few studies addressing the association investigated. Statistical heterogeneity was assessed using the i-squared (I
2) of the overall measure of association to identify the magnitude of the indicator and then the meta-analysis was carried out. The measures of association estimated were the relative risk and their respective 95% confidence intervals, obtained with fixed effect analysis using the Mantel-Haenszel method for binary variables using the STATA 16.0 statistical package. Sensitivity analysis was carried out using the risk of bias and the value of evidence and strength of recommendations were verified using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
ResultsA total of 399 studies were retrieved from the databases, plus five studies identified by an active search of the study reference list. Fifteen of these were selected to make up the systematic review and meta-analysis, as can be seen in the study input-output flow diagram shown in Figure 1. The data extracted from the 15 studies in the systematic review is shown in Table 2.
Characteristics of the selected studiesThe randomized clinical trial studies selected were published between 2007 and 2024 on the American (5), African (1) and Asian (9) continents. The intervention used was OCI, and the control groups used distilled water, exclusive parenteral fluids, routine care or standardized feeding regimens in the respective neonatal units. The routes of delivery of the intervention reported in the studies were: gastric lavage,
19 syringe drips
8,20-31 or oral hygiene with a swab.
32It should be noted that all the studies aimed to assess the efficacy of OCI on outcomes related to some health condition in newborns, with four presenting death as the primary outcome
23,29,31,32 and eleven as a secondary outcome.
8,19-22,24-28,30 None of the studies used found a statistically significant result for the investigation on the death outcome, and four of these studies did not report a
p-value.
22,25,28,31 In addition, fourteen studies were published in the form of scientific articles in journals and one of the studies was an abstract presented at the European Society of Pediatric Gastroenterology, Hepatology and Nutrition congress.
31The risk of bias of the studies was assessed using Cochrane's RoB 2 tool (Figure 2) and showed that three studies were at low risk;
23,26,32 two were of some concern
24,25 and ten of the fifteen studies were at high risk of bias.
8,19-22,27,28,30 The judgment of the risk of bias was assessed as an overall high risk of bias, due to the incompleteness of the outcome data (Domain 3) and the risk of bias in the assessment of the outcome measure (Domain 4) presented by the articles. Added to this factor is the diversity of OCI protocols between all the studies and the disparities in sample sizes. There was also insufficient description of the randomization, concealment and allocation of the samples, or even no description at all.
8,21,22,28,30,31 All the studies stated that the treatment was randomly allocated; however, five studies
21,22,25,28,31 did not specify the method used to generate the random sequence. Similarly, six studies did not mention allocation concealment methods;
8,19,25,27,29,31 of these, three reported that blinding of the intervention was not applicable due to the nature of the intervention;
8,25,29 and one study, despite presenting allocation concealment, did not mention blinding.
30 Among the studies, six were blinded to conduct the OCI.
20,22-24,26,32Probable methodological weaknesses were identified in most of the included studies, when assessed by RoB 2
22,25-30 (Figure 2). The quality of the studies included in this meta-analysis is presented graphically with percentages for each domain and the result of each RoB 2 assessment (Figure 2).
Meta-analysisThe meta-analysis showed a positive influence of OCI administration on reducing the incidence of death in PTNBs (Figure 3). The total sample size was 1,497 participants. The effect on the all-cause mortality rate between the groups was carried out with a total sample of 197 PTNB deaths between the intervention (83) and control (114) samples combined. All the studies showed deaths among the intervention and control samples, except for the studies by Sohn
et al.
25 and Romero-Maldonado
et al.
22 which showed no deaths in the treatment group; and no deaths in the control group were found in the articles by Rodriguez
et al.
20 and Easo
et al.
24 The heterogeneity test between the studies showed an I
2=0.0%. The Q test showed
p=0.649, which accepts the null hypothesis of homogeneity of the studies, so we can opt for a fixed-effect meta-analysis. The meta-analytical measure of the studies was RR= 0.750 (95%CI=0.582-0.967), showing that there was a protective effect of OCI on the incidence of death in PTNBs between the intervention and control groups. The analysis was dominated by three studies
27,29,30 which had a weight of 53.81%. The graph shows that there is an effect of the OCI intervention in preventing death in PTNBs.
A sensitivity analysis was carried out for the risk of bias, omitting three studies
20,22,24 which were at the extremes of the distribution of results (outliers) from the forest plot; and two of them 20,24 with less weight in the final analysis. The data remained unchanged, with homogeneity maintained (I
2=0.0%,
p=0.835) and a meta-analytical measure of RR= 0.750 (95%CI=0.58-0.98), very similar to that of the final analysis.
The value of the evidence and the strength of the recommendations was verified using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, and it was concluded that the ranking of the studies used in this meta-analysis, being clinical trials randomized, makes the evidence, a priori, classified as of moderate confidence. Thus, it is likely that additional research will have an important impact on our confidence in the estimate of the effect, and we believe that in the future it may change the estimate to high confidence in favor of the treatment.
DiscussionThe current study, which included 1,497 PTNB, showed a trend towards a positive effect of OCI in reducing mortality in premature infants, by statistically synthesizing the numerical results of 15 randomized clinical trials, the primary studies that made up this meta-analysis.
8,19-32The findings of this meta-analysis are confirmed by the recent clinical trial conducted by Martins
et al.
11 and two other meta-analyses recently published.
10,33 However, the meta-analyses by Huo
et al.,
12 Peng
et al.
9 and Slouha
et al.
34 did not observe a reduction in the incidence of death in the treatment group compared to the control group.
It is worth noting that, among the studies evaluated, the positive effect of OCI on various events that contribute to health problems and neonatal death was demonstrated, such as: late onset sepsis,
19,22,26,28 feeding intolerance,
28 shorter time to obtain full enteral feeding,
20,27 a significant reduction in the time taken to use parenteral fluids,
19 shorter hospitalization time
8,19,20,27,32 and shorter time to recover birth weight.
20 Immunological benefits were also found, such as: higher IgA levels,
20,22 inhibition of inflammatory cytokine secretion,
26 increased circulating levels of immunoprotective factors
26 and establishment of beneficial oral microbiota,
25 when comparing the respective intervention groups, which used OCI, with the controls.
The findings of these studies reinforce the biological plausibility of OCI in reducing the incidence of neonatal deaths, since it has been shown to have a protective effect against various clinical disorders that contribute to PTNBs deaths, especially those with very low birth weight. The World Health Organization stresses that, in order to reduce mortality in premature infants, it is necessary to prevent infectious diseases and ensure adequate nutrition, as these are important risk factors for this population,
1 whose vulnerabilities include immaturity of the immune system and digestive tract.
5,35The results also contribute to prior knowledge of the value and importance of colostrum in the first days of life. When a full-term newborn is breastfed directly, the lymphoid tissue in the oropharynx can absorb the immunoactive components of colostrum, thus favoring immune protection. For premature infants who cannot be fed orally, the immune protection of colostrum can be effectively provided by administering oropharyngeal colostrum.
5,35,36 PTNB who received oropharyngeal colostrum had lower levels of pro-inflammatory factors (IL-6, IL-8, TNF-α and IFN-γ) and higher levels of anti-inflammatory factors (IL-10), indicating that this route of administration plays an active role in the immune regulation of premature infants,
36 provided by the contact of protective biofactors present in colostrum with the lymphoid tissue of the oropharynx of premature infants.
5,35,36The results of the 15 studies that made up this meta-analysis also showed that OCI is a safe procedure for PTNBs.
8,19,21,28,30 Furthermore, as it is a simple, feasible and low-cost procedure, OCI can be used as a primary prevention measure, a strategy that can help to mitigate the risk factors inherent to prematurity, such as immaturity of the immune system,
20,22,25,26 immaturity of the digestive tract,
5,35 delay in starting enteral feeding
4,20,27 and length of hospital stay.
8,19,22,27,32We found a lack of standardization in terms of the technique used to manage OCI. Most of the studies (13) used an oropharyngeal colostrum administration protocol; however, the study by Patel and Shaikh
19 used gastric lavage with the mother's own milk, and the study by Jain
et al.
32 administered colostrum through oral hygiene with a swab. The volume, frequency and duration of daily applications differed between the protocols, ranging from 0.1 to 0.3 mL; frequencies were every two, three, four, six or eight hours; and the minimum duration of the intervention was up to 48 hours and the maximum until enteral feeding began.
Of the fifteen studies, the intervention protocol of 0.2 mL every two hours for up to 48 hours predominated, and could be extended until the start of oral feeding in five studies.
21-23,25,27 In contrast, the data found by Fu
et al.
10 suggests that the appropriate application of colostrum should be administered every four hours and the duration of treatment should be between eight and ten days. There is agreement between the studies on the benefits of early intervention.
A fundamental requirement in a meta-analysis is to ensure homogeneity in terms of clinical and methodological aspects between the individual studies that make up the data in the systematic review. We found that the test for heterogeneity between the studies included in the meta-analysis showed no heterogeneity, i.e. the individual studies evaluated showed homogeneity and consistency of results between them.
As for limitations, the main one is inherent to the methodology of meta-analysis, as it is based on published primary studies, which may have methodological restrictions. This limitation is in line with similar studies using the same methodology. On the other hand, what sets this study apart is that it specifically assessed the influence of OCI on the incidence of death among PTNBs, systematically followed research strategies using a protocol validated by PROSPERO, included 15 randomized clinical trials with homogeneity and consistency of results between them, making up a sample of 1,497 PTNBs; these measures can offset the limitations inherent in the studies on which it is based.
ConclusionIt can be concluded that the quantitative analysis of the 15 primary studies, comprising 1,497 PTNBs, included in the systematic review with meta-analysis, confirmed the assumption of the positive effect of OCI in reducing neonatal mortality in PTNBs. However, further primary research with higher statistical power is needed to prove this and other benefits related to OCI. The results of this study can provide a basis for the clinical implementation of OCI in neonatal units, as a way of preventing neonatal deaths, as well as supporting future studies. All of the above strengthen the use of OCI for PTNBs, which is a safe, simple and easy-to-implement measure.
References1. World Health Organization (WHO). Born too soon: decade of action on preterm birth. Geneva: WHO; 2023. [access in 2024 Mar 1]. Available from:
https://www.who.int/publications-detail-redirect/97892400738902. Ministério da Saúde (BR). Banco de dados do Sistema Único de Saúde - DATASUS. Informações de Saúde, Sistema de Informações sobre Nascidos Vivos (SINASC). Brasília (DF): Ministério da Saúde; 2020. [access in 2024 Mar 2]. Available from:
https://svs.aids.gov.br/daent/centrais-de-conteudos/paineis-de-monitoramento/natalidade/nascidos-vivos/3. Ministério da Saúde (BR). Banco de dados do Sistema Único de Saúde - DATASUS. Informações de Saúde, Sistema de Informações sobre Mortalidade (SIM). Brasília (DF): Ministério da Saúde; 2020. [access in 2024 Mar 1]. Available from:
https://svs.aids.gov.br/daent/centrais-de-conteudos/paineis-de-monitoramento/mortalidade/infantil-e-fetal/4. Garofalo NA, Caplan MS. Oropharyngeal mother's milk. Clin. Perinatol. 2019 Mar; 46 (1): 77–88.
5. Gila-Diaz A, Arribas SM, Algara A, Martín-Cabrejas MA, López De Pablo ÁL, Sáenz De Pipaón M,
et al. A review of bioactive factors in human breastmilk: a focus on prematurity. Nutrients. 2019 Jun; 11 (6): 1307.
6. Da Cruz Martins C, De Santana Xavier Ramos M, Viana Cardoso Amaral M, Santos Passos Costa J, Souza Cerqueira E, De Oliveira Vieira T,
et al. Colostrum oropharyngeal immunotherapy for very low birth weight preterm infants: protocol of an intervention study. BMC Pediatr. 2020 Aug; 20 (1): 371.
7. Ramos MDSX, Martins CDC, Souza ES, Vieira GO, Gomes-Filho IS, Figueiredo ACMG,
et al. Oropharyngeal colostrum immunotherapy and nutrition in preterm newborns: meta-analysis. Rev Saúde Pública. 2021 Dec; 55: 59.
8. Sharma D, Kaur A, Farahbakhsh N, Agarwal S. Role of oropharyngeal administration of colostrum in very low birth weight infants for reducing necrotizing enterocolitis: a randomized controlled trial. Am J Perinatol. 2020 Jun; 37 (7): 716-21.
9. Peng B, Yu L, Qian J, Zheng B, Zhang Y, Zhu C. Oral application of mother's own milk for reducing necrotizing enterocolitis in preterm infants: an updated meta-analysis of RCTs. Evid Based Complement Alternat Med. 2023 Apr; 2023: 7378064.
10. Fu ZY, Huang C, Lei L, Chen LC, Wei LJ, Zhou J,
et al. The effect of oropharyngeal colostrum administration on the clinical outcomes of premature infants: A meta-analysis. Int J Nurs Stud. [Internet]. 2023 Aug; 144: 104527.
11. Martins CDC, Ramos MDSX, Lyrio AO, Vieira TDO, Cruz SSD, Vieira GO. Oropharyngeal colostrum immunotherapy and risk reduction of mortality in very low birth weight premature newborns: a clinical trial. J Pediatr. (Rio J.). 2024 Jan; 100 (1): 32–9.
12. Huo M, Liu C, Mei H, Zhang Y, Liu C, Song D,
et al. Intervention effect of oropharyngeal administration of colostrum in preterm infants: a meta-analysis. Front. Pediatr. 2022; 10: 895375.
13. Silva ADP, Machado RCM, Nascimento BF, Da Cunha LVS, Padilha PDC. Analysis of clinical outcomes of oropharyngeal colostrum administration in very low-birth-weight preterm newborns. Nutrition. 2021; 90: 111292.
14. Vieira TDO, Martins CDC, Ramos MDSX, Lyrio AO, Cruz SSD, Costa MGR,
et al. Colostrum immunotherapy and length of hospital stay in preterm infants: an intervention study. Rev Bras Saúde Mater Infant. 2024; 24: e20230074.
15. Tao J, Mao J, Yang J, Su Y. Effects of oropharyngeal administration of colostrum on the incidence of necrotizing enterocolitis, late-onset sepsis, and death in preterm infants: a meta-analysis of RCTs. Eur J Clin Nutr. 2020 Aug; 74 (8): 1122-31.
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD,
et al. A declaração PRISMA 2020: uma diretriz atualizada para relatar revisões sistemáticas. Rev Panam Salud Pública. 2021 Dez; 46: 1.
17. Ministério da Saúde (MS). Secretaria de Ciência, Tecnologia, Inovação e Insumos Estratégicos em Saúde. Departamento de Gestão e Incorporação de Tecnologias em Saúde. Diretrizes metodológicas: elaboração de revisão sistemática e meta-análise de ensaios clínicos randomizados [
Internet]. Brasília (DF): Ministério da Saúde; 2021. 93 p. [access in 2021 Nov 12]. Available from:
http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_elaboracao_revisao_sistematica_meta-analise.pdf18. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors).Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane [
Internet]. 2023 [access in 2023 Nov 12]. Available from: www.training.cochrane.org/handbook
19. Patel AB, Shaikh S. Efficacy of breast milk gastric lavage in preterm neonates. Indian Pediatr. 2007 Mar; 44 (3): 200–03.
20. Rodriguez NA, Groer MW, Zeller JM, Engstrom JL, Fogg L, Du H,
et al. A Randomized Controlled Trial of the Oropharyngeal Administration of Mother's Colostrum to Extremely Low Birth Weight Infants in the First Days of Life. Neonatal Intensive Care. 2011 July/Aug; 24 (4): 31-5.
21. Ferreira DMLM, Oliveira AMM, De Leves DV, De Bem ÉB, Fatureto GG, Navarro NF,
et al. Randomized Controlled Trial of Oropharyngeal Colostrum Administration in Very-low-birth-weight Preterm Infants. J Pediatr Gastroenterol Nutr. 2019 Jul; 69 (1): 126-30.
22. Romero-Maldonado S, Soriano-Becerril DM, García-May PK, Reyes-Muñoz E, Muñoz-Ortíz EG, Carrera-Muiños S,
et al. Effect of Oropharyngeal Administration of Colostrum in Premature Newborns ≤32 Weeks of Gestation on the Immune Response and Neonatal Morbidity: A Double-Blind Randomized Clinical Trial. Front Pediatr. 2022; 10: 891491.
23. Rodriguez NA, Moya F, Ladino J, Zauk A, Prazad P, Perez J,
et al. A randomized controlled trial of oropharyngeal therapy with mother's own milk for premature infants. J Perinatol. 2023 May; 43 (5): 601-7.
24. Easo S, Naqeeb N, Tolba A, John A, Azab A, Ata S,
et al. A randomized controlled trial of oral immunotherapy therapy with colostrum or breast milk and clinical outcomes among preterm babies. Iran J Neonatol. 2021 Jan; 12 (2): 14-20.
25. Sohn K, Kalanetra KM, Mills DA, Underwood MA. Buccal administration of human colostrum: impact on the oral microbiota of premature infants. J Perinatol. 2016 Feb; 36 (2): 106–11.
26. Lee J, Kim HS, Jung YH, Choi KY, Shin SH, Kim EK,
et al. Oropharyngeal colostrum administration in extremely premature infants: An RCT. Pediatrics. 2015; 15 (2): e357–66.
27. Abd-Elgawad M, Eldegla H, Khashaba M, Nasef N. Oropharyngeal administration of mother's milk prior to gavage feeding in preterm infants: a pilot randomized control trial. J Parenter Enteral Nutr. 2020 Jan; 44 (1): 92-104.
28. Hariharan D, Veluswami G, Balasubramanium L, Kannappan V. Oropharyngeal breastmilk administration in extreme prematurity reduces gram negative sepsis and feed intolerance. J Pediatr Gastroenterol Nutr. 2017; 64: 784-5.
29. Aggarwal R, Plakkal N, Bhat V. Does oropharyngeal administration of colostrum reduce morbidity and mortality in very preterm infants? A randomised parallel-group controlled trial. J Paediatr Child Health. 2021 Apr; 57 (9): 1467-72.
30. Sudeep KC, Kumar J, Ray S, Dutta S, Aggarwal R, Kumar P. Oral Application of Colostrum and Mother's Own Milk in Preterm Infants - A Randomized, Controlled Trial. Indian J Pediatr. 2022 Jun; 89 (6): 579–86.
31. Mannan MA, Sihan MN, Afreen S, Rahman T, Shahidullah M, Moni SC,
et al. Administration colostrum in preventing mortality and morbidity in preterm infants. Int J Contemp Pediatr. 2023 May; 10 (6): 761–8.
32. Jain S, Kumar M, Tripathi S, Singh SN. Oral application of mother's own milk for prevention of late onset sepsis in preterm very low birth weight neonates: a randomized controlled trial. Breastfeed Med, 2022 Jan; 17 (1): 59-64.
33. Anne RP, Kumar J, Kumar P, Meena J. Effect of oropharyngeal colostrum therapy on neonatal sepsis in preterm neonates: A systematic review and meta-analysis. J Pediatr Gastroenterol Nutr. 2024 Mar; 78 (3): 471–87.
34. Slouha E, Anderson ZS, Ankrah NMN, Kalloo AE, Gorantla VR. Colostrum and preterm babies: a systematic review. Cureus. 2023; 15 (7): e42021.
35. Chen LL, Liu J, Mu XH, Zhang XY, Yang CZ, Xiong XY,
et al. Oropharyngeal administration of mother's own milk influences levels of salivary sIgA in preterm infants fed by gastric tube. Sci Rep. 2022 Feb; 12 (1): 2233.
36. Martín-Álvarez E, Diaz-Castro J, Peña-Caballero M, Serrano-López L, Moreno-Fernández J, Sánchez-Martínez B,
et al. Oropharyngeal colostrum positively modulates the inflammatory response in preterm neonates. Nutrients. 2020 Feb; 12 (2): 413.
Authors' contribution: Silva JR, Brandão HV, Ramos MSX, Costa MGR and Martins CC: conception, analysis and interpretation of the data, writing and revision of the manuscript. Vieira TO and Vieira GO: study design and critical revision of the manuscript. Silva JR is the researcher responsible for the study, working from conception to writing and revising the final version. All the authors have approved the final version of the article and declare no conflicts of interest.
Received on April 22, 2024
Final version presented on December 2, 2024
Approved on December 3, 2024
Associated Editor:Gabriela Sette
 ; Heli Vieira Brandão2
; Heli Vieira Brandão2 ; Michelle de Santana Xavier Ramos3
; Michelle de Santana Xavier Ramos3 ; Tatiana de Oliveira Vieira4
; Tatiana de Oliveira Vieira4 ; Matheus Gomes Reis Costa5
; Matheus Gomes Reis Costa5 ; Camilla da Cruz Martins6
; Camilla da Cruz Martins6 ; Graciete Oliveira Vieira7
; Graciete Oliveira Vieira7