ABSTRACT
OBJECTIVES: to evaluate cesarean taxes by looking at Robson classification on 10 groups (G) and the principal indications at the prevalent groups and at G10.
METHODS: cross-sectional, observational, retrospective study, including all deliveries performed in a public hospital in Distrito Federal in 2019. Data were collected from medical records and pregnant women were classified in 10 groups. Pearson’s chi-squared test was used to calculate the p-value. The risk estimate for cesarean was defined by common odds ratio of Mantel-Haenszel, with calculation of odds ratio (OR) and 95% confidence interval (CI95%).
RESULTS: there were 2,205 deliveries, 1,084 (49.1%) of which were cesarean and 1,121 (50.9%) vaginal deliveries. The principal factors for cesarean were G5 (39.3%), G2 (21.2%) and G1 (13.6%). At G10, cesarean had 51.5% of births, not differing statistically from the other groups (p>0.05). Considering all preterm births, G6 to G10 and the other groups, there is a bigger chance of cesarean happening in relation to normal labor (OR=1.4; CI95%= 1.011-2.094; p=0.042). Dystocia remained at G1 and G2, previous cesarean at G5 and hypertensive syndrome at G10.
CONCLUSION: cesarean was most prevalent delivery route, showing elevated rates even in primiparous and preterm births. Preponderance of dystocia and acute fetal distress suggests better evaluation of the diagnostic criteria, mainly in G1, G2 and G10.
Keywords:
Cesarean section, Vaginal birth after cesarean, Term birth, Premature birth, Delivery obstetric
RESUMO
OBJETIVOS: avaliar as taxas de cesárea pela classificação de Robson em 10 grupos (G) e as principais indicações nos grupos prevalentes e no G10.
MÉTODOS: estudo transversal, observacional, retrospectivo, incluindo todos os nascimentos em um hospital público do Distrito Federal em 2019. Dados coletados de prontuários eletrônicos e as parturientes categorizadas em dez grupos. Teste qui-quadrado de Pearson para o valor de p e razão de chances comum de Mantel-Haenszel para estimativa de risco, com OR e IC95%.
RESULTADOS: ocorreram 2.205 nascimentos, 1.084 (49,1%) cesáreas e 1.121 (50,9%) partos normais. Os principais contribuintes para a cesárea foram G5 (39,3%), G2 (21,2%) e G1 (13,6%). No G10, cesárea teve 51,5% dos nascimentos, não diferindo estatisticamente dos demais grupos (p>0,05). Considerando todos os prematuros, G6 ao G10 e demais grupos, há maior chance de cesárea em relação ao parto normal (OR=1,4; IC95%= 1.011-2.094; p=0,042). Distócia prevaleceu nos G1 e G2, Cesárea prévia no G5 e Síndromes hipertensivas no G10.
CONCLUSÃO: a cesárea mostrou taxas elevadas inclusive nas primíparas e nos prematuros. Predomínio de Distócia e Sofrimento fetal sugerem melhor avaliação destes critérios diagnósticos, principalmente em G1, G2 e G10.
Palavras-chave:
Cesárea, Nascimento vaginal após cesárea, Nascimento a termo; Nascimento prematuro, Parto obstétrica
IntroductionThe cesarean section is a procedure that, with adequate indication, reduces maternal and fetal morbidity and mortality. However, when performed unnecessarily, it brings different risks, for both the pregnant woman and the fetus, in the short and long term.
1,2 Between maternal endings, one can mention death, hemorrhage (can require hysterectomy or blood transfusion), uterine rupture, anesthetic complications, and shock, among other things, it could also lead to compromising the future generations due to placental abnormality and uterine rupture. To the newborn, one can mention laceration, breathing problems and hospitalization in the Intensive Care Unit (ICU).
2The World Health Organization (WHO) recommends a cesarean rate between 10 and 15%, higher values, did not imply a reduction in maternal or neonatal mortality.
1 For a long time, these rates have been aimed without taking into account relevant population determinants such as socioeconomic factors. In 2015, an instrument validated by the WHO was developed to adjust these values to demographic, clinical, and obstetric characteristics of the population, reaching rates of 25 to 30% of cesarean sections for Brazil, a rate well below the 58.2% found at the time, reaching 38.1% in public hospitals and 92.8% in private hospitals.
3–5 The prevalence of high rates of cesarean sections in private hospitals is also common in other countries in Latin America. One hypothesis for such an increase is that medical indications have become more permissive, leading to higher elective cesarean sections. Among these possible causes, a fact that is a worldwide trend, we can mention maternal, cultural, obstetric, and healthcare-related factors.
6–9One of the most common practices resulting from elective cesarean sections was the interruption above 37 weeks of gestational age (GA), given the classification of preterm births before 37 weeks of GA. However, current studies have observed that pregnancies of ≥ 37 and < 39 weeks of GA implied greater risks of adverse events when compared to later pregnancies, that is, of ≥ 39 weeks of GA. These studies highlight the existence of heterogeneity in the group of full term pregnancies, proposing that pregnancies with GA of 37 ≥ and < 39 weeks should be classified as an early term.
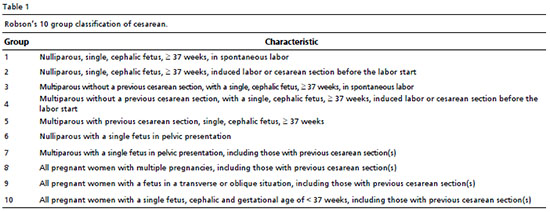
10,11In 2001, Robson developed a simple methodology classification that categorizes pregnant women into ten groups using the information on five obstetric characteristics: parity, previous obstetric history, gestation type, onset of labor, fetal presentation, and gestational age. It is a practical, reproducible, fully inclusive, and mutually exclusive method that allows an understanding of the internal structure of cesarean rates in a health institution and the identification of strategic groups that can be addressed to prevent unnecessary cesareans.
3,12 In this line, in 2015 the WHO recommends its use to analyze and compare cesarean rates over time in the same hospital and between different hospitals and, with that, to propose intervention strategies.
1Considering the importance of knowing not only cesarean taxes but also specific groups to lead intervention politics, this study had as a principal objective to know about cesarean taxes and identify the groups that were more tax helpers, looking from Robson Classification. As secondary objectives, assess cesarean rates on premature newborns, considering Group 10, same as the other groups, including Groups 6 to 9, and know the indications on more prevalent cesarean groups.
MethodsCross-sectional, observational, retrospective study, including all deliveries performed in a public hospital of the Unified Health System (SUS) of the State Department of Health of the Federal District (SES-DF), located in the city of Brasília, Brazil, which is a reference for five of the thirty-one Administrative Regions of the DF, in the period from 01/01/2019 to 12/31/2019.
13 The convenience sample included all deliveries that took place in the studied hospital over a period of one year, totaling 2,205 deliveries.
The data were collected from electronic medical records, through Intersystems trakCare™ system, from SES-DF, Brasília/Brazil, based on the ratio of discharge of newborns (NB) issued by the SUS Information Collection and Analysis Center. Parturients who had a home birth, in transit, or another health institution were excluded from the study.
Gestational Age was evaluated in completed weeks at the time of delivery by early ultrasound examination or by the date of the last menstrual period and, in the absence of one of these data, by Capurro. Type of pregnancy, classified as single, multiple, cephalic, pelvic or oblique. For obstetrict history, as nulliparous or multiparous, subdivided in the presence or absence of uterine scarring. The start of labor as spontaneous, induced, or cesarean out of labor, thus being classified according to the 10 Robson Groups (Table 1). Group 1 (G1). For the presence or not of complications during gestation, were utilized data from forms of neonate and considered as yes, every presence information of pathology as infection on the urinary tract (IUT), vulvovaginitis, vaginal bleeding, gestational hypothyroidism, anemia, Mellitus diabetes or gestational diabetes, hypertensive syndrome, tobacco use, psychiatric sickness, between other complications.
For the assessment of fetal maturity, the complete GA in weeks during delivery was divided into premature or preterm infants born att < 37 weeks of GA, early term at 37 ≥ and < 39, and full term at ≥ 39 weeks. In the analysis of cesarean indications, these were grouped according to the consensus of obstetric care of the American College of Obstetricians and Gynecologists (ACOG), defining five groups of cesarean indications: labor dystocia, fetal distress, previous cesarean scar, maternal hypertensive disorder, and other indications.
14The statistical analysis was performed using the IBM SPSS Statistics v.22 software. Pearson’s chi-squared test was used to calculate the
p-value. The risk estimate for the cesarean sections was defined by the common odds ratio of Mantel-Haenszel, with calculation of odds ratio (OR) and 95% confidence interval (CI95%). For all statistical tests, the 95% significance level (
p < 0.05) was defined
The study was approved by the Research Ethics Committee of the Health Sciences Teaching and Research Foundation (FEPECS/SES), under Opinion No. 3,590,309.
ResultsDuring the study period, there were 2,205 deliveries, 1,084 (49.1%) of which were cesarean and 1,121 (50.9%) vaginal in a reference public hospital in a city of Brasília-DF. Women aged between 20 and 34 years, predominated, accounting for 69.3% of the total. Multiparous, without previous cesarean, with unique gestations, cephalic fetus, spontaneous start of labor that informed some gestation complications, also prevailed.
Table 2 presents the main characteristics of these parturients.
According to Robson’s Groups, groups G1, G5 and G2 accounted for 69.2% of the deliveries. Groups G5 and G2 contributed with more than 50% of cesarean sections, with 39.3% and 21.2% respectively. Within the groups, G5 had 81.1% of their deliveries being cesarean, followed by groups G2 with 77.4% and G10 with 51.5% according to Table 3.
In groups that contributed the most to cesarean rates, complications on the gestation were related by 63,9% of women on G1, 58,7% on G2, 59,2% on G5, and 86,5% on G10. Dystocia appeared as a cesarean indicator prevalent on G1 (68,7%) and G2 (59,6%), for G5 previous cesarean prevailed (81,5%) and G10 hypertensive syndrome (32,7%). Still on G10, 53 (52,5%) started labor spontaneously, 48 (47,2%) were submitted to induction or cesarean before labor and 24 (23,8%) presented precious surgical scars. (Table 4).
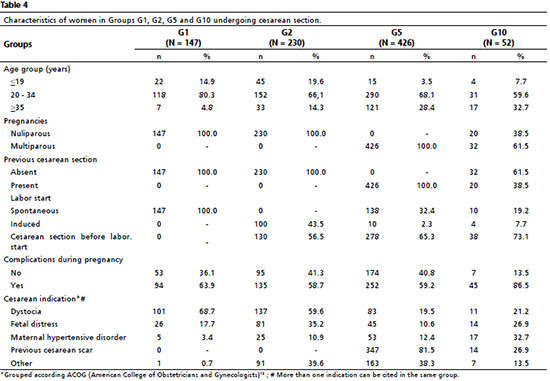
On G10, it was characterized by a unique gestation, cephalic fetus and IG < 37 weeks, including with previous surgical scar, 52 (51,5%) were submitted to cesarean and 57 (56,4%) were multiparous. In relation to labor manners, the G10 does not statistically differ compared to the other groups. Although, when all the premature (< 37 weeks) were reunited, including the groups G6 to G9, we have a total of 126 births. Of these, 73 (58%) were cesarean and 53 (42%) were normal labors. The statistical analysis between the three categories did not show the difference, but, when comparing the births with < 37 weeks with the births with ≥ 37 weeks, one can see the significant statistic difference, being that the births with < 37 years old had 1,4 more chances of having cesarean when compared with births with ≥ 37 weeks (Table 5).
DiscussionThis study evaluated 2,205 deliveries, 1,084 (49.1%) of which were cesarean and 1,121 (50.9%) vaginal deliveries in a public hospital in the Federal District that, although a reference for deliveries, it is not a reference for premature births due to the absence of a neonatal ICU. Therefore, it was expected that cesarean rates would not reach values above the 25-30% rate recommended for Brazil.
4 Similar rates were found in China, with values of 50.9% in secondary hospitals and 55.9% in tertiary hospitals.
15 Women between 20 and 25 years old, multiparous, single fetus, cephalic, and with spontaneous start labor predominated, criteria considered to be of lower risk for cesarean section.
16Although around 55% of the women had related some complication on the labor, one can understand that the majority is not a determinant of labor, and many are passive of therapeutic intervention during prenatal
16. We can mention urinary infections, vulvovaginitis, the first quarter complications (seasickness, bleeding, menstrual cramps), and the risk of premature labor between others, for example. The actions of prenatal care will undoubtedly have a positive or negative impact during labor, but the method of delivery, in public institutions in the Federal District, is most often decided in the hospital environment. The literature describes well the absolute indications for abdominal delivery, such as cephalopelvic disproportion, chorioamnionitis, maternal pelvic deformity, eclampsia, and HELLP syndrome, fetal asphyxia or acidosis, umbilical cord prolapse, total placenta previa, abnormal fetal presentation that makes vaginal delivery impossible, and uterine rupture. Indications considered relative such as altered fetal cardiotocography, failure to progress labor, and previous cesarean section, among others, must be individually assessed and discussed among the assisting professionals of the parturient.
5There was a predominance of cesarean sections in Robson’s G1, G2, and G5 groups, which together account for 74.2% of all cesarean sections. G5 had the most expressive numbers, with the highest proportion of cesarean sections within its group (81.1%), in addition to being the one that most contributed to the total rate of cesarean sections in the hospital (39.3%), data already well corroborated by the literature.
17,18 Although women in G5 could present other indications for cesarean section, this study found that 35.7% of cesarean sections had a previous cesarean section as one of their indications. This is worrying, as it reinforces in these patients the culture that it is safer or that they would not be able to have a succeeding vaginal delivery.
6,19 It is noteworthy that the presence of a previous uterine scar is not an absolute indication for a new surgery, this indication being better supported when it comes to 2 or more previous cesareans,
4,14 having the need for the first two to wait for spontaneous labor start or even perform the procedure of trial of labor. This recommendation is based on studies that demonstrated that for G5, when well indicated, cesarean sections were associated with a lower chance of mortality, however, its indiscriminate practice was associated with a greater chance of adverse outcomes.
20,21The nulliparous, represented by G1 and G2, had, respectively, 27% and 77,4% of cesarean in the groups, representing 34,8% of cesarean done and contributing with 17,1% of all cesarean births. This data becomes even more relevant when we consider that the method of delivery of the first pregnancy will have consequences for the woman’s reproductive life, and may negatively affect future pregnancies, be it because of the adverse events that may arise, due to limitation of reproductive life due to recurrent cesarean sections corroborated by the high indices presented here by the G5.
17,18,22 Different strategies have been proposed to avoid cesarean sections in these groups, such as: using Robson’s classification to assess, monitor, and compare cesarean rates; perform more efficient labor screening; wait for adequate time for the progression of labor to occur; careful choice of patients who are going to undergo labor induction; not accepting cesarean indications given by other specialists when there is no evidence to support the procedure; provide training for problematic vaginal deliveries; use fetal monitoring methods during childbirth; seek for a second opinion in controversial situations.
2,6,21,23 As it is a public institution, with responsibility for professional training (internship and medical and multi-professional residency), these strategies should be discussed and implemented, as the success shown in other researches of cesarean rate reductions, from 3,1% to 0,1% on G1 and from 42% to 16,9% on G2.
20,23Considering cesarean sections in all groups, 52.2% were performed before going into labor. Labor involves a series of physiological mechanisms, with consequences for both the mother and the fetus, which have the purpose of preparing both of them for the moment of delivery and preparing the pregnant woman for the puerperium. When a cesarean section is performed before going into labor, many of these mechanisms are lost, and the newborn needs to undergo a sudden transition from intra to extrauterine life.
6 Therefore, cesarean sections before going into labor should be avoided, unless there is a precise indication for it.
G8, characterized by all multiple pregnancies, as it represents a small part among all deliveries (1.5%), has little influence on the final percentage of the hospital. However, it is important to note that 93% of births in this group were by cesarean section, although twin pregnancies alone are not an indication for this route since the cesarean section with the first fetus in the cephalic presentation did not reduce the risk of adverse perinatal events, both maternal and fetal.
4,24 On the other hand, it has been reported that vaginal delivery would imply a greater risk of maternal morbidity, especially concerning hemorrhage.
25 However, a good evaluation of the pregnant woman, vitality, and position, especially of the first fetus, if in good conditions in this institution, which trains obstetric professionals, guaranteeing the safety of these deliveries, should encourage the parturients to have normal births.
2At G10, 51,5% of women were submitted to cesarean, 23,8% had a previous cesarean and 47,2% were submitted to induction or cesarean before entering labor, even though more than half of the women from G10 were multiparous. When comparing the types of labor between preterm (< 37 weeks), precocious term (37 ≤ and < 39 weeks) and term (≥ 39 weeks) there was no statistically significant difference, but when comparing preterm (< 37 weeks) and the others (both early term and full term), the data showed that preterm neonates (< 37 weeks) were more likely to be born by cesarean sections than by vaginal deliveries (OR = 1.4; CI95% = 1.011-2.094;
p < 0.05). In preterm pregnancies without risk factors, having a cesarean section does not imply an improvement in the maternal or neonatal outcome. Studies have shown that high cesarean rates are associated with worse neonatal outcomes.
26,27 When the presence of risk factors is taken into account, with the presence of important maternal and fetal comorbidities, cesarean sections improve neonatal outcomes.
26,27 In our study, a high rate of complications in pregnancy was found in this group (86.5%), thus being able to explain, at least partially, its high rate of cesarean section.
Studies point out that the presence of a previous cesarean section is a risk factor for the occurrence of premature births.
28,29 In a cohort carried out in the Netherlands with 268,495 women, it was shown that the incidence of premature birth in the second pregnancy was higher in women with a previous cesarean section than in women with a previous vaginal delivery (adjusted OR = 1.14; CI95% = 1.07-1.21). Such incidence is increased both in pregnant women for whom a cesarean section was planned (adjusted OR = 1.86; CI95% = 1.58-2.18) and in those for which a cesarean section was not planned (adjusted OR = 1.40; CI95% = 1.24-1.58).
29 A Chinese meta-analysis with 10 cohort studies totaling 10,333,501 pregnant women obtained a similar result in which pregnant women with previous cesarean sections are more prone to premature births compared to pregnant women with a history of vaginal delivery (RR = 1.10; CI95% = 1.01-1.20).
28 Thus, the prevention of cesarean sections should always be considered, especially in nulliparous women, considering that cesarean sections can cause the incidence of subsequent premature births.
Although the researchers had access to data on all deliveries, the study in question has some limitations. The databases are secondary and the indications for cesarean sections given by the obstetricians on duty, being part of a subjective character due to the lack of more accurate information, making it impossible to know the criteria used in the indication. Even though the studied hospital is not a referee on premature births, the birth rate on G10 of 4,6% was the highest rate on this group on DF in 2019, which was 2,1%, enabling the analysis of this study.
30During the study period, the predominant labor manner in a hospital was cesarean, with a rate of 49,1%, a number that passed the recommended by WHO, although in agreement with data about cesarean in Brazil. The main contributors to this number were grups G1, G2, and G5, reinforcing the care for women in these groups, with priority given to primiparous women. Within G10, more than half of these pregnant women underwent cesarean sections, and the chance of cesarean section increased when all premature infants were grouped together. As stated by the WHO, “Every effort should be made to provide caesarean sections to women in need, rather than striving to achieve a specific rate”.
1 Thus, this study proposes that each institution reviews and develops its cesarean rate target based on ensuring the quality of excellence in maternal and neonatal care.
References1.World Health Organization (WHO). WHO Statement on Caesarean Section Rates. Geneva: WHO; 2015. [access in 2021 abr 15]. Available from:
https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf2.Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014 Mar; 210 (3): 179-93.
3.Souza JP, Betran AP, Dumont A, Mucio B, Gibbs Pickens CM, Deneux-Tharaux C,
et al. A global reference for caesarean section rates (C-Model): a multicountry cross-sectional study. BJOG Int J ObstetGynaecol. 2016 Feb; 123 (3): 427-36.
4.Comissão Nacional de Incorporação de Tecnologias no SUS (CONITEC). Diretrizes de atenção à gestante: a operação cesariana: Brasília (DF): Ministério da Saúde; 2015. [access in 2021 abr 15]. Available from:
https://www.gov.br/conitec/pt-br/midias/relatorios/2016/relatorio_diretrizes-cesariana_final.pdf5.Guimarães RM, Silva RLPD, Dutra VGP, Andrade PG, Pereira ACR, Jomar RT,
et al. Fatores associados ao tipo de parto em hospitais públicos e privados no Brasil. Rev Bras Saúde Matern Infant. 2017; 17 (3): 571-80.
6.Mariani GL, Vain NE. The rising incidence and impact of non-medically indicated pre-labour cesarean section in Latin America. Semin Fetal Neonatal Med. 2019; 24 (1): 11-7.
7.Nakamura-Pereira M, Carmo Leal M, Esteves-Pereira AP, Domingues RMSM, Torres JA, Dias MAB,
et al. Use of Robson classification to assess cesarean section rate in Brazil: the role of source of payment for childbirth. Reprod Health. 2016 Oct; 13 (Supl. 3): 128.
8.Vogel JP, Betrán AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J,
et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. 2015 May; 3 (5): e260-70.
9.Lavender T, Hofmeyr GJ, Neilson JP, Kingdon C, Gyte GM. Caesarean section for non-medical reasons at term. Cochrane Database Syst Rev. 2012 Mar; 2012 (3): CD004660.
10. Fleischman AR, Oinuma M, Clark SL. Rethinking the Definition of “Term Pregnancy”. 2010 Jul; 116 (1): 136-9.
11. Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW,
et al. Timing of Elective Repeat Cesarean Delivery at Term and Neonatal Outcomes. N Engl J Med. 2009 Jan; 360 (2): 111-20.
12. Robson MS. Classification of caesarean sections. Fetal Mater Med Rev. 2001; 12: 23-39.
13. Distrito Federal (BR). Secretaria de Estado de Saúde. Relatório Anual de Gestão 2017. Brasília (DF): Secretaria de Estado de Saúde; 2017. 308 p. [Internet]. [access in 2021 abr 15]. Available from:
http://www.saude.df.gov.br/wp-conteudo/uploads/2017/11/RAG-2017_CSDF_10.12.2018.pdf14. ACOG Practice bulletin Nº 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010 Aug; 116 (2 Pt 1): 450-63.
15. Wang X, Hellerstein S, Hou L, Zou L, Ruan Y, Zhang W. Caesarean deliveries in China. BMC Pregnancy Childbirth. 2017 Feb;17 (1): 54.
16. Peixoto S. Manual de assistência pré-natal. 2
nd ed. São Paulo: Federação Brasileira das Associações de Ginecologia e Obstetrícia; 2014.
17. Begum T, Rahman A, Nababan H, Hoque DME, Khan AF, Ali T,
et al. Indications and determinants of caesarean section delivery: Evidence from a population-based study in Matlab, Bangladesh. PLoS One. 2017 Nov; 12 (11): e0188074.
18. Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. Am J Obstet Gynecol. 2018 Jul; 219 (1): 105.e1-105.e11.
19. Conselho Federal de Medicina (CFM). Resolução CFM nº 2.144/2016. É ético o médico atender à vontade da gestante de realizar parto cesariano, garantida a autonomia do médico, da paciente e a segurança do binômio materno fetal. Brasília (DF): DOU de 22 de junho de 2016; (118 Seção 1): 138. [access in 2021 mai 2]. Available from:
https://sistemas.cfm.org.br/normas/visualizar/resolucoes/BR/2016/214420. Sabol B, Denman MA, Guise JM. Vaginal birth after cesarean: an effective method to reduce cesarean. Clin Obstet Gynecol. 2015 Jun; 58 (2): 309-19.
21. Zhang JW, Branch W, Hoffman M, De Jonge A, Li SH, Troendle J,
et al. In which groups of pregnant women can the caesarean delivery rate likely be reduced safely in the USA? A multicentre cross-sectional study. BMJ Open. 2018 Aug; 8: e021670.
22. Miller ES, Hahn K, Grobman WA; Society for Maternal-Fetal Medicine Health Policy Committee. Consequences of a primary elective cesarean delivery across the reproductive life. Obstet Gynecol. 2013 Apr; 121 (4): 789-97.
23. Blomberg M. Avoiding the first cesarean section--results of structured organizational and cultural changes. Acta Obstet Gynecol Scand. 2016 May; 95 (5): 580-6.
24. Barrett JFR, Hannah ME, Hutton EK, Willan AR, Allen AC, Armson BA,
et al. A randomized trial of planned cesarean or vaginal delivery for twin pregnancy. N Engl J Med. 2013 Oct; 369 (14): 1295-1305.
25. Easter SR, Robinson JN, Lieberman E, Carusi D. Association of Intended Route of Delivery and Maternal Morbidity in Twin Pregnancy. Obstet Gynecol. 2017 Feb; 129 (2): 305-10.
26. Bannister-Tyrrell M, Patterson JA, Ford JB, Morris JM, Nicholl MC, Roberts CL. Variation in hospital caesarean section rates for preterm births. Aust N Z J Obstet Gynaecol. 2015 Aug; 55 (4): 350-6.
27. Lee HC, Gould JB. Survival rates and mode of delivery for vertex preterm neonates according to small- or appropriate-for-gestational-age status. Pediatrics. 2006 Dec; 118 (6): e1836-44.
28. Zhang Y, Zhou J, Ma Y, Liu L, Xia Q, Fan D,
et al. Mode of delivery and preterm birth in subsequent births: A systematic review and meta-analysis. PLoS One. 2019 Mar 14; 14 (3): e0213784.
29. Visser L, Slaager C, Kazemier BM, Rietveld AL, Oudijk MA, Groot C,
et al. Risk of preterm birth after prior term cesarean. BJOG. 2020 Apr;127 (5): 610-7.
30. Ministério da Saúde (BR). Sistema de Informações sobre Nascidos Vivos - SINASC. [Internet]. [access in 2022 abr 20]. Available from:
http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sinasc/cnv/nvuf.def.Received on May 29, 2021
Final version presented on May 16, 2022
Approved on 27 August, 2022
Authors’ contribution: Moresi EH, Moreira PP, Ferrer IL, Baptistella MKCS e Bolognani CV: elaborated, analyzed and interpreted the data, and wrote and reviewed the manuscript.
The authors approved the final version of the article and declare no conflict of interest.
 ; Pedro Piancastelli Moreira2
; Pedro Piancastelli Moreira2 ; Isabela Lemos Ferrer3
; Isabela Lemos Ferrer3 ; Melorie Kern Capovilla Sarubo Baptistella4
; Melorie Kern Capovilla Sarubo Baptistella4 ; Cláudia Vicari Bolognani5
; Cláudia Vicari Bolognani5