ABSTRACT
OBJECTIVES: describe the frequency of maternal stress and psychic risk indicators in newborns who were exposed to the neonatal intensive care unit (NICU) after hospital discharge.
METHODS: observational, analytical, cohort study, sample of 26 participants (13 exposed and 13 not exposed to the NICU). Maternal stress was assessed by Inventário de Sintomas de Stress para Adultos de Lipp (ISSL) (Lipp’s Stress Symptoms Inventory for Adults) and psychological risk by Indicadores Clínicos de Risco para o Desenvolvimento Infantil (IRDI) (Clinical Risk Indicators for Child Development), 15 days after hospital discharge and at 4 months of corrected age.
RESULTS: the study found a frequency of stress of 23.1% in mothers of newborns who were exposed to NICUs and 38.5% of psychological risk in these newborns. The following associations were found: maternal stress and newborn exposure to the NICU (p=0.037); maternal stress and newborn exposure time to NICU (p=0.031); psychological risk and prematurity (p=0.014). There were no association between psychic risk and maternal stress; and there was no difference in the frequency of psychological risk between the groups of newborns.
CONCLUSIONS: newborn hospitalization in the NICU is associated with maternal stress, but not with psychological risk. Prematurity can cause psychological risk. Maternal stress was not associated with psychological risk.
Keywords:
Maternal stress, Psychic risk, Maternal and child mental health, Psychological development, Preterm newborn
RESUMO
OBJETIVOS: descrever a frequência de estresse materno e indicadores de risco psíquico em recém-nascidos que foram expostos à unidade de terapia intensiva neonatal (UTIN).
MÉTODOS: estudo observacional, analítico, coorte, amostra de 26 participantes (13 expostos e 13 não expostos a UTIN). O estresse materno foi avaliado pelo Inventário de Sintomas de Stress para Adultos de Lipp e o risco psíquico pelo IRDI (Indicadores Clínicos de Risco para o Desenvolvimento Infantil), 15 dias após a alta hospitalar e aos quatro meses de idade corrigida.
RESULTADOS: o estudo encontrou frequência de estresse de 23,1% nas mães de RN que foram expostos a UTIN e 38,5% de risco psíquico nestes bebês. Encontrou as seguintes associações: estresse materno e exposição do RN à UTIN (p=0,037); estresse materno e tempo de exposição do RN à UTIN (p=0,031); risco psíquico e prematuridade (p=0,014). Não encontrou associação entre risco psíquico e estresse materno; e não encontrou diferença na frequência de risco psíquico entre os grupos de RN.
CONCLUSÕES: a internação do RN em UTIN está associada a estresse materno, mas não a risco psíquico. A prematuridade pode causar risco psíquico. O estresse materno não apresentou associação com risco psíquico.
Palavras-chave:
Estresse materno, Risco psíquico, Saúde mental materno infantil, Desenvolvimento psicológico, Recém-nascido pré-termo
IntroductionCare in the neonatal intensive care unit (nicu) is marked by high technology and the urgency and precision of actions to maintain the lives of newborns (nbs). advances in neonatal care technology have made it possible for extremely low birth weight, preterm infants and those affected by perinatal diseases to survive.
1According to data from the World Health Organization,
1 annually about 30 million premature and/or sick newborns need hospital care beyond those involving childbirth. Of these NBs, between eight and ten million need care in the NICU so that they can survive and develop. In the field of mental health, some studies show an increase in the incidence of psychological problems in premature infants, such as attention deficit, socialization problems, difficulty in emotional control, pervasive developmental disorders and auditory and visual processing deficits.
2,3Some authors also relate the separation of the NB andhis/her mother during the stay in the NICU, whereas problems in the process of establishing the subjective bond between them. It is through this bond that the experiences of the NBs are elaborated and gain meaning. The absence of this relationship would place the NBs in a situation in which various physical sufferings resulting from hospitalization in the NICU would remain uninterpreted, which could constitute a trauma, hindering their relationship with their own body and, consequently, with themselves and with other people.
4-6Studies suggest that not only NBs suffer from the passage through the NICU, but also their parents, which is evident by their high level of stress.
7-11 NBs’parents, weakened by hospitalization, present, in addition stress, depressive symptoms, anxiety, anguish, difficulty of mothers to perform their maternal role and interrupt interactions with the NBs.
12-14 Therefore, the treatment for parents is also essential.
15 Taking care of parents is important to preserve their mental health and the NBs, studies suggest that the emotional state of the parents interfere in the child’s psychic development . French researchers concluded that depressed mothers have a qualitatively lower relationship with their newborns/infants when compared to mothers without depression.
7Studies show that with psychoanalytically oriented interventions, individual or in groups, it is possible to reposition the parents in relation to their subjective functions with the NBs.
16 The intervention should start during hospitalization in the NICU
15 and continue after hospital discharge.
1 The work involves both parents and the NB from the beginning because it is understood that psychological development takes place from the NB’s bodily and psychic relationship with the mother figure (or another person who performs this function) and the environment that surrounds him/her. Early intervention is based on activities that make the baby move from pure sensory perception to the field of meaning.
17,18The intervention will strengthen the relationship between the mother and the NB, stimulating the development of mothering, that is, the ability to transform maternal speech into an act in front of the NB, so that the development takes place. It is necessary to support the mother’s emotions, such as her fears and fantasies regarding the motivations of the event that led the NB to be admitted to the NICU. This reduces anxiety levels, provides symbolization of the Real, reorganization of the Imaginary and elaboration of trauma, which allows the installation of maternal discourse.
15At the same time, it will be necessary for the psychologist/analyst to anticipate the parents’ ability to perform maternal and paternal roles, even before they are prepared to do so. This anticipation takes place through the psychologist’s discourse. This provides the organization of conscious and unconscious elements of the parents for the establishment of desire in the exercise of their functions.
16 This whole process can be strengthened by experiences such as those described by Cheng
19 where the mother stays with the NB for up to six hours every day during the admission to the NICU, resulting in a greater bond between the mother and the NB and a reduction in their levels of stress.
In addition to understanding and intervening on the emotional state of the parents, it is necessary to assess the NB’s mental state to guide the intervention on him/her as well. However, it appears that the instruments described in the literature for this purpose are rare, extensive and complex to perform.
8In Brazil, between 2000 and 2008, a group of researchers characterized “psychic indicators” to assess babies aged 0 to 18 months their psychological development and guide the professionals’ work in mental health. The
Indicadores Clínicos de Risco para o Desenvolvimento Infantil (IRDI) (Clinical Risk Indicators for Child Development) Research defined and validated these psychological risk indicators based on Freud, Winnicott and Lacan’s theories. There are 31 observable risk indicators in the first 18 months of a child’s life – the IRDIs. By observing and interviewing the parents, looking for signs that the NB/baby’s development is occurring in a healthy way. The absence of these signs indicates the need for intervention. The indicators are organized in four axes: subject’s assumption, where there is a bet of a psychic subject even before its constitution; the establishment of demand, which are interpretations that the NBs unintentional acts are requests directed to the mother figure; alternation presence/absence, space of creation and development that occurs between the small intervals of absence of the caregiver; paternal function, which is the insertion of a third element in the mother/child relationship.
4The present study aimed to describe the frequency of maternal stress and psychological risk indicators in newborns who were exposed to the NICU, in a city in the State of Santa Catarina.
MethodsThis was an observational, analytical, cohort, ambispective study. with data collected from december 2017 to december 2018 in the nb’s follow-up on This was an observational, analytical, cohort, ambispective study. With data collected from December 2017 to December 2018 in the NB’s follow-up on
Risco para o Desenvolvimento da Secretaria Municipal de Saúde de Mafra,Santa Catarina, (Risk for Development of the Municipal Health Department of Mafra), composed of a psychologist, speech therapist and nutritionist from
Núcleo de Ampliado de Saúde da Família (NASF) (Expanded Family Health Center). The follow-up occurred up to four months of corrected age of the infants. The sample was taken from a population at risk for development, in public health.
The distribution of the population source, according to the latest update available on DATASUS, at the time of the study design, in 2015 was: 3.017.668 live births in Brazil, of which 0.68% (20.388) had Apgar scores below 7 in the fifth minute, 10.83% (326.879) were born premature and 8.44% (254.688) were born weighing less than 2.500 grams; 97.223 live births in Santa Catarina, of these 0.60% (579) had Apgar scores lower than 7 in the fifth minute, 10.82% (10.515) were born prematurely and 7.72% (7.503) were born weighing less than 2.500 grams; 777 live births in Mafra, 0.77% (3) had Apgar scores below 7 in the fifth minute, 11.33% (88) were born prematurely and 7.98% (62) were born weighing less than 2.500 grams.
20 These health indicators, extracted from the “
Agenda de Compromissos para a Saúde Integral da Criança e Redução da Mortalidade Infantil”,
21 contribute to developmental risks, such as severe asphyxia (Apgar less than 7 in the fifth minute of life), prematurity (gestational age inferior to 37 weeks), low birth weight (less than 2.500 grams), and perinatal events that culminate in NICU admission.
Participation in the research met the following inclusion criteria: being a resident of the city in Mafra (SC); be considered a NB at risk for development, being a group with and another without exposure to NICU admission. The following were excluded from the sample: NBs who had severe clinical conditions that alter neuropsychomotor development such as neurological syndromes and sequelae and NBs whose mothers had withdrawn the informed consent. Considering these elements, the sample consisted of 26 participants, 13 of whom were exposed to NICU admission and 13 were not exposed. No sampling technique was used, all eligible participants were invited to participate in the study.
The variable exposure to NICU admission was positioned as an Independent Variable and the variables Maternal Stress and Psychic Risk Indicators were positioned as Dependent Variables.
To assess Maternal Stress, the
Inventário de Sintomas de Stress para Adultos de Lipp (ISSL) (Lipp Stress Symptom Inventory for Adults) was used, which diagnoses stress and the phase in which the participant is (alert, resistance, near-exhaustion and exhaustion) applicable to participants between 15 and 75 years.
22To evaluate the Psychic Risk Indicators, the “
Indicadores Clínicos de Risco para o Desenvolvimento Infantil” (IRDI) (Clinical Risk Indicators for Child Development) protocol was used. The instrument aims at the early detection of psychic risk in NBs/infants aged 0 to 18 months. There are 31 clinical indicators of psychological risk or child’s development problems. The presence of indicators, separated by age group, characterizes a good process of subjective constitution and their absence is a risk for the NB’s /infant’s psychological development.
4Data collection from the Data Record Form prepared by the authors took place retrospectively from the NB’s medical record at a reference Health Unit. The collection of data referring to Psychic Risk, consisting of the application of the IRDI and the data referring to maternal stress, through the ISSL occurred within 15 days after the newborn’s hospital discharge, with a new application around four months considering the age corrected for preterm infants.
The first collection period was stipulated based on the functioning of the service where the research took place and it proved to be favorable, as the IRDI must have two applications at each psychological development stage, the first stage being from birth to four months of the child’s corrected age. The instrument is organized in this way so that the initial assessment takes place with enough time for an intervention to favor healthy development before the second application, which occurs around the end of the ideal period for acquiring the mental health indicator.
The collected data were entered into a spreadsheet (Microsoft Excel, 2013) and exported to the SPSS 25.0software for statistical analysis. The confidence interval adopted was 95% (significance level
p<0.05) for all inferential analyses.
For the description of the quantitative variables, the mean and median central tendency measurements, the variability standard deviation measurement, minimum and maximum were calculated. To describe the nominal qualitative variables, the absolute frequency (n) and the relative frequency (%) were calculated. The normality of the quantitative variables was analyzed with the Shapiro Wilk Test and all had a non-normal distribution. Thus, the comparison of quantitative variables as a function of nominal qualitative variables was performed using the Mann-Whitney test. The association between nominal qualitative variables of two categories was performed using Fisher’s Exact Test, and the association between qualitative variables of more than two categories was performed using Pearson’s Chi-Square Test.
The study took place after the approval by the Human Research Ethics Committee of the Health Sciences Sector of the
Universidade Federal do Paraná, CAAE 78303217.9.0000.0102.
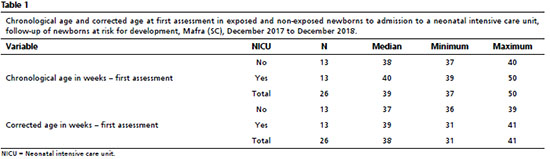
Resultstwenty-six newborns participated in the study, their chronological and corrected ages in the first evaluation are shown in table 1. the total sample (n=26) had a median age of 39 weeks, minimum of 37 and maximum of 50 weeks. the median considering the corrected age was 38 weeks, with the youngest participant to be evaluated at 31 weeks and the most mature at 41 weeks. newborns exposed to nicu admission had a median age of 40 weeks of gestation and a corrected age of 39 weeks (table 1). the length of stay in the nicu had a median of seven days, with a minimum of one day and a maximum of 90 days.
As for the mothers, there were 26 participants, with an average age of 27 years, 50% had completed high school, 61.5% reported not having their own income and 92.3% were married or living in a stable relationship with the NB’s parent. The study found, in the first evaluation, a frequency of maternal stress of 23.1% in mothers of newborns exposed to NICU admission and 3.8% in mothers of newborns who were not exposed, demonstrating that there was an association between maternal stress and exposure of newborns to NICU admission (
p=0.037 – Table 2). There was also an association between maternal stress and time of exposure of the NB’s to NICU admission (
p=0.031 – Table 3).
As for psychic risk, 38.5% of the NBs who were exposed to NICU admission had two or more absences of indicators in the first assessment, which suggests psychic risk. In the population of NBs not exposed to the NICU, the frequency was 30.8%. In other words, there was no significant difference in the frequency of psychological risk indicators between exposed and non-exposed newborns to NICU admission. When relating maternal stress and psychic risk, there was no association between these variables. When relating psychic risk and prematurity, it was possible to verify that there was an association between psychic risk and prematurity (
p=0.014 – Table 4), when considering the total sample studied.
In the second evaluation, after psychological intervention on the dyads, the infants had emotional characteristics appropriate for their age and the incidence of maternal stress was 3.8%.
DiscussionThe present study showed that mothers who have their children exposed to nicu admission present more stress than mothers of nbs who were not exposed, demonstrating an association between maternal stress and nb’s admission to the nicu. it also indicated that the length of exposure to nicu hospitalization was a factor in increasing the frequency of maternal stress. that is, mothers had greater emotional difficulties in enduring longer periods of hospitalization of nbs in the nicu.
Using the Parental Stress Scale: Neonatal Intensive Care Unit to assess the parents’ stress levels of newborns admitted to the NICU, Varghese
9 evaluated 343 parents in the North of India, where he concluded that mothers of hospitalized newborns have high levels of stress. The same result was found by Chourasia,
23 when evaluating 100 mothers of newborns admitted to the NICU. In the present study, mothers who had their children hospitalized in the NICU were more stressed than mothers who did not have their children hospitalized. Maternal stress persisted after hospital discharge.
In this context, only one American study
24 was found that included maternal stress after hospital discharge. Which leads to questioning how mothers have been treated in the follow-up of NBs at risk of development worldwide, especially in Brazil. In this study, Holditch-Davis
et al.
24 described the mothers’ patterns of suffering who had preterm newborns (PTNBs) exposed to NICU admission. A total of 232 mothers were analyzed and, as a result, 52 mothers had low distress; 57 mothers with moderate suffering; 20 mothers with a high level of depression and anxiety; 78 mothers with high levels of stress; 20 mothers with high levels of depression and anxiety and 25 mothers with extreme distress. Mothers were assessed during the hospitalization period and then reassessed during the child’s first year of life, indicating persistence of most symptoms at different levels throughout the study period. However, there was no intervention in the studied sample. The persistence of symptoms of emotional distress up to one year after their evaluation demonstrates the importance of public policies aimed at the evaluation and specific follow-up for this population.
The present study found a frequency of 26.9% of maternal stress in the first assessment and 3.8% in the second assessment, when considering only the subgroup of mothers whose newborns were exposed to NICU admission. However, all cases with stress-related complaints, even without a diagnosis according to the assessment instrument, received intervention in the form of psychological counseling.
Counseling sessions took place weekly or fortnightly, according to the participant’s availability to attend. In these sessions, unlike a psychotherapy that covers broad themes, the theme dealt with was limited to the present moment regarding to motherhood. The fact that the sample was small may have been important for all mothers to receive intervention and thus, raise the hypothesis that early treatment of maternal stress symptoms is effective in reducing them.
The intervention proposals that focus on a follow-up that takes into account the mother-NB/infant dyad and not just the NB/infant after hospital discharge found in the Brazilian literature consulted are psychoanalytically oriented. The intervention proposals mention about the importance of the follow-up, but such interventions are focused on the psychological development of the NB. Mothers are welcomed for the intervention due to the supposed or found risks for the subjective constitution of the NB.
5,18In general, the intervention proposals described in the literature did not start from maternal suffering to welcome the dyads in care.
5,18 Thus, the mother seems to be understood as an accessory to the NB’s psychic constitution. Mothers in mental distress, but who have NB/infants in good mental health, are missing the opportunity for early interventions, which can lead to worsening the conditions over time. Research in this sense is essential regarding to women’s mental health.
As for the psychic risk, the present study sought to understand whether when mothers go through the stressful experience of having their NBs’ hospitalized in the NICU, their ability to exercise their maternal function is affected. What could prevent them from satisfying the basic psychic needs of the NB’s psychological development, since it is the maternal function that supports, through the mother’s desire, the entire subjective constitution of the NB, which occurs in a process of alienation and subsequent separation. Alienation in the period in which there are no psychological conditions on the part of the NB to support his/her psychic and the gradual separation as his/her subjectivity develops. It is in this context that the subject’s assumption, demand establishment, presence/absence alternation and the entry of the paternal role occur, as previously described.
18Findings in the literature variously describe the impact of maternal mental illness history on children’s health and development. In the validation study of the Neurobehavioral Network Scale in the NICU, conducted by Lester,
8 found protective factors for neurodevelopment in PTNBs without clinical diagnoses other than prematurity, namely: care aimed at stimulating neurodevelopment while still in the NICU; family involvement; parental satisfaction; less maternal depression and lower rates of parental stress.
Santos
et al.,
25 found signs of psychological distress in 229 mothers and the effect of this on the affective relationship and PTNBs neuropsychomotor development. The results indicated that mothers in distress had difficulties in stimulating the development of the infant at two and six months of corrected age. At 12 months, they still had difficulties in stimulating cognitive development in a milder way and motor development more significantly. It is noteworthy that, although they have difficulties in stimulation, they did not present significant difficulties in developing a positive involvement with the infants from an affective point of view.
Mughal
et al.26 evaluated the impact of stress on the neuropsychomotor development of 108 PTNBs at four months of corrected age, verifying that maternal stress was significantly associated with poor results in the baby’s personal-social interaction skills and also in gross motor development. The present study is in agreement with Santos
et al.,
25 findings because by stating that the mother’s psychological distress did not affect her ability to develop a positive affective involvement with the baby, it allows establishing a correlation with the ability to establish an affective bond between a stressed mother and NB, verified through the IRDI.
According to Laznik,
6 the infant’s psychological risk cannot be attributed to the parents’ psychopathological state . For a long time, the literature worked with the hypothesis that psychic risk was an effect of the parents’ emotional state. However, it is currently known that the parents’ emotional illness occurs in the face of the NB/baby’s developmental difficulties. It is the parents who can get sick in the face of the child’s difficulty and not the other way around. The current hypothesis is that the parents, when they get sick, would give up investing in the establishment of the subjectifying bond with the NB/baby, tired and disillusioned with the unanswered investiture. Which could worsen the condition of the NB/infant without intervention. In this context, the present study found data that point out that maternal mental health is impacted by events that affect the NB in an important way, being fundamental the reception of the dyad in treatment when necessary.
Another point that the present study sought to verify was the impact on the psychological development of exposure to NICU admission for NBs through the assessment of psychic risk. The NB went through a potentially traumatic experience according to the literature.
3,6 Because pleasurable bodily experiences are essential for the development of a healthy relationship with the body, where this body is represented in a unified way. The bodily discomfort caused by the interventions in the NICU tend to bring bad psychic representations about the bodily experience, generating a sense of discomfort with oneself.
18 Therefore, evaluating the impact on subjective constitution is important for mental health prevention. Consequently, the results of the present study demonstrate that, in the first evaluation, 34.6% of the total sample had two or more absences of psychological development indicators, which suggests psychological risk, being similarly divided among the NBs exposed to hospitalization in the NICU and the unexposed. The time of exposure in the NICU stay, as well as the invasive procedures, did not show statistical significance in the sample evaluated regarding the association with psychological risk.
Many newborns need admission to the NICU because of prematurity, so the present study verified the association between prematurity and psychological risk, concluding that gestational age has a significant association with psychological risk regardless of hospitalization in the NICU. In line with the present study, Hoogstraten
et al.
27 found an incidence of two or more absences in the IRDI in 40% of the PTNBs evaluated at four months, while in the group of newborns (term newborns) the incidence was 27.27%, finding an association between prematurity and psychological risk.
The same group was also evaluated
27 using the PREAUT instrument and, in general, they found that, using both instruments, PTNBs presented 11% more psychological risk than full-term newborns. The authors make use of the hypothesis that the element associated with such findings in the PTNB population is the fact that many have been admitted to the NICU for long periods of up to 60 days. It is important to note that Hoogstraten
27 study excluded infants who had health conditions that could impair performance in the assessment due to neurological issues such as genetic syndromes, neurological injuries or sensory deficits.
However, the present study evaluated the association between psychological risk and NICU admission, as well as psychological risk and length of NICU stay and did not find statistical significance to accuse such an association. As for the psychic risk, at four months 100% of the IRDIs present was found. This element may be related to the insufficient sample and to have occurred by chance, however, it is hypothesized that two factors may be associated with the finding, namely: the characteristics of the NICU where 92.3% of the NBs came from,
Maternidade Dona Catarina Kuss (MDCK), and the fact that they are all included in the Monitoring Service of NBs at risk of development.
MDCK guarantees quality, safe and humanized care to patients with practices that favor integral development, taking into account the NB’s biopsychosocial aspects admitted to the NICU. The institution recognizes and promotes the presence of the mother’s companion, emphasizing the importance of the companion offering physical and emotional support during the maternal hospitalization. Maternity encourages breastfeeding whenever possible, which favors the mother/NB bond, providing the benefits of this bond as early as possible.
28 O’Brien
et al.
29 highlights that the daily insertion of parents in the care of the PTNB’s, whether in the NICU or not, is shown to be effective in improving newborns’ general health and the parents’ mental health.
As for the Follow-up Service for NBs at risk for development, they leave the maternity hospital with a day and pre-scheduled time in the Primary Care for reception and evaluation by an interdisciplinary team formed by a psychologist, nutritionist and speech therapist. This first contact takes place within 15 days after hospital discharge. When necessary, the mental health intervention begins in this first consultation and continues according to the mother and/or the newborn’s needs, and can be weekly or fortnightly exclusively with a psychologist. It was in this first contact that the first stage of data collection in the present study took place. Regardless of the need for intervention or not, all patients return 30 days after the first consultation, where they are again welcomed and oriented.
The follow-up schedule repeats the consultation at an average of four months, when the second data collection of this study took place. Thus, it is hypothesized that the entire process of humanization of the MDCK, combined with the follow-up offered by the
Secretaria Municipal de Saúde (Municipal Health Department) through the NASF, were associated with the good results found in terms of psychic risk and also maternal stress. Studies with larger populations are important to assess the real impact of intervention, not early, but in time, on psychological risk. Validating the hypothesis that the procedure adopted both in the maternity hospital and in the follow-up offered by the NASF, the study carried out in the United Kingdom on the topic of humanization at the time of hospital discharge of the NBs whowent through the NICU, pointed to an increase in positivity, parents’ hope and feeling in being able to control the situation.
30Thus, the present study concluded that the NB’s hospitalization in the NICU is associated with the establishment of maternal stress, but it is not associated with psychological risk. The finding regarding to the NBs’ mental health can be justified by the fact that the primary subjectivizing bond has been preserved even during hospitalization or has been satisfactorily reestablished after the end of this period.
It was found in the total sample that mothers in emotional distress were able to perform the maternal function in order to provide NB’s psychic development, therefore, there was no association between maternal stress and psychic risk. Thus, it can be inferred that the psychological support offered to the dyads contributed to the mothers sustaining the maternal function.
Considering the above, it can be mentioned that a special look is needed for populations that are more sensitive to the development of Mental Disorders, having timely intervention as an ally in preventing their emergence or worsening.
References1.World Health Organization (WHO). Survive and thrive: transforming care for every small and sick newborn. Genebra: WHO; 2019. [access in 2020 abr 20]. Available from:
https://www.who.int/publications/i/item/97892415158872. Beltrame VH, Moraes AB, Souza APR. Perfil sensorial e sua relação com risco psíquico, prematuridade e desenvolvimento motor e de linguagem por bebês de 12 meses. Rev Ter Ocup Univ São Paulo. 2018; 29 (1): 8-18.
3. Rogers CE, Lenze SN, Luby JL. Late preterm birth, maternal depression, and risk of preschool psychiatric disorders. J Am Acad Child Adolesc Psychiatry. 2013 Mar; 52 (3): 309-18.
4. Mariotto RMM, Pesaro ME. O roteiro IRDI: sobre como incluir a ética da psicanálise nas políticas públicas. Estilos Clin. 2018;23 (1): 99-113.
5. Zen ET, Triani I. Acompanhamento pós-alta de mães-bebês: prevenção via continuidade dos cuidados. In: Parlato-Oliveira E, Cohen D, orgs. O Bebê e o Outro: seu entorno e suas interações. São Paulo: Instituto Langage; 2017. p. 129-40.
6. Laznik MC, Chauvet M. Tratamento psicanalítico de um bebê com risco de autismo e seu tratamento concomitante em sensoriomotricidade. In: Souza APR, Zimmermann VB, orgs. Inserção de crianças e adolescentes na cultura: caminhos possíveis. São Paulo: Instituto Langage; 2016. p. 13-36.
7. Cohen D, Viaux S, Sint-Geoges C, Leclère C, Chetouani M, Xavier J. Importância do estudo das interações precoces mãe-bebê através de métodos automatizados do sinal social: aplicações à psicopatologia. In: Parlato-Oliveira E, Cohen D, orgs. O Bebê e o Outro: seu entorno e suas interações. São Paulo: Instituto Langage; 2017. p. 91-110.
8.Lester BM, Andreozzi-Fontaine L, Tronick E, Bigsby R. Assessment and evaluation of the high risk neonate: the NICU Network Neurobehavioral Scale. J Vis Exp. 2014; 90: 1-9.
9. Varghese MA. Study on Parental Stress in the Neonatal ICU Using Parental Stressor. Pediatrics. 2015; 135 (Supl. 1): S9.
10. Varma JR, Nimbalkar SM, Patel D, Phatalak AG. The level and sources of stress in mothers of infants admitted in neonatal intensive care unit. Indian J Psychol Med. 2019; 41 (4): 338-42.
11. Beck CT, Woynar J. Posttraumatic stress in mothers while their preterm infants are in the newborn intensive care unit: a mixed research synthesis. ANS Adv Nurs Sci. 2017; 40 (4): 337-55.
12. Mackay LJ, Benzies KM, Barnard C, Hayden KA. A scoping review of parental experiences caring for their hospitalized medically fragile infants. Acta Paediatr.2020; 109 (2): 266-75.
13. Das A, Gordon-Ocejo G, Kumar M, Kumar N, Needlman R. Association of the previous history of maternal depression with post-partum depression, anxiety, and stress in the neonatal intensive care unit. J Matern Fetal Neonatal Med. 2021 Jun; 34 (11): 1741-6.
14. Gondwe KW, Brandon D, Yang Q, Malcom WF, Small MJ, Holditch-Davis D. Emotional distress in mothers of early-preterm infants, late-preterm infants, and full-term infants in Malawi. Nursing Outlook. 2020; 68 (1): 94-103.
15. Garthus-Niegel S, Horsch A, Graz MB, Martini J, Von Soest T, Weidner K, Eberhard-Gran M. The prospective relationship between postpartum PTSD and child sleep: a 2-year follow-up study. J Affect Disord. 2018 Dez. 241:71-9.
16. Engel D, Ghazzi MS, Silva HC.Acompanhamento Terapêutico e a Relação Mãe-Bebê. Psicol Ciênc Prof. 2014; 34 (4): 1045-58.
17. Gratier M. A melodia antes das palavras? O papel da voz nas primeiras trocas sociais do bebê. In: Parlato-Oliveira E, Cohen D, orgs. O Bebê e o Outro: seu entorno e suas interações. São Paulo: Instituto Langage; 2017. p. 29-38.
18. Zimmermann VB. ‘Encontros’ necessários para a constituição psíquica. In: Parlato-Oliveira E, Cohen D, orgs. O Bebê e o Outro: seu entorno e suas interações. São Paulo: Instituto Langage; 2017. p. 47-66.
19. Cheng C, Franck LS, Ye XY, Hutchinson AS, Lee SK, O’Brien K. Evaluating the effect of Family Integrated Care on maternal stress and anxiety in neonatal intensive care units. J Reprod Infant Psychol. 2021 Apr; 39 (2): 166-79.
20. Ministério da Saúde (BR). DataSus – Departamento de Informática do SUS. 2020. [access in 2020 mar 18]. Available from:
http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvsc.def21. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Agenda de Compromissos para a Saúde Integral da Criança e Redução da Mortalidade Infantil. Série A: Normas e Manuais Técnicos. Brasília (DF): Ministério da Saúde (BR); 2004. [access in 2020 mar 18]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/agenda_compro_crianca.pdf22. Lipp MEN. Manual do Inventário de Sintomas de Stress para Adultos de Lipp (ISSL). São Paulo: Casa do Psicólogo; 2000.
23. Chourasia N, Surianarayanan P, Adhisivan B, Bhat BV.NICU admissions and maternal stress levels. Indian J Pediatr. 2013; 80 (5): 380-4.
24. Holditch-Davis D, Santos H, Levy J, White-Traut R, O’Shea TM, Geraldo V, David R. Patterns of psychological distress in mothers of preterm infants. Infant Behav Dev. 2015;41: 154-63.
25. Santos Jr H, Yahn Q, Docherty SL, White-Traut R, Holditch-Davis D. Relationship of Maternal Psychological Distress Classes to Later Mother–Infant Interaction, Home Environment, and Infant Development in Preterm Infants. Res Nurs Health. 2016; 39 (3): 175-86.
26. Mughal MK, Ginn CS, Magill-Evans J, Benzies KM. Parenting stress and development of late preterm infants at 4 months corrected age. Res Nurs Health. 2017; 40 (5): 414-23.
27. Hoogstraten AMRV, Souza APR, Moraes AB. Indicadores clínicos de referência ao desenvolvimento infantil e sua relação com fatores obstétricos, psicossociais e sociodemográficos. Saúde Pesq.2018; 11 (3): 589-601.
28. Santa Catarina. Secretaria de Estado de Saúde. Política da Qualidade da M.D.C.K. 2018. [access in 2018 fev 8]. Available from:
http://www.saude.sc.gov.br/index.php/resultado-busca/geral/10349-maternidade-dona-catarina-kuss.
29. O’Brien K, Robson K, Bracht M, Cruz M, Lui K, Alvaro R, et al. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicenter, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health. 2018 Apr; 2 (4): 245-54.
30. Ingram J, Redshaw M, Manns S, Beasant L, Johnson D, Fleming P, et al. “Giving us hope”: parent and neonatal staff views and expectations of a planned family-centred discharge process (Train-to-Home). Health Expect. 2017 Aug; 20 (4): 751-9.
Received on September 18, 2020
Final version presented on June 20, 2022
Approved on July 27, 2022
Authors’ contribution: Paula LS: conceptualization, data curation, formal analysis, investigation, method, project management, resources, software, validation, conceptualization, visualization up to the writing of the article. Celli A: conceptualization, data curation, formal analysis, investigation, method, project management, resources, software, validation, conceptualization, visualization up to the writing of the article. Mariotto RMM: conceptualization, formal analysis, investigation, method, project management, validation, and writing the review. Lagos-Guimarães HNC and Marciniak A: collaboration in writing the review. The authors approved the final version of the article and declare no conflict of interest.
The authors approved the final version of the article and declare no conflict of interest.
 ; Adriane Celli2
; Adriane Celli2 ; Rosa Maria Marini Mariotto3
; Rosa Maria Marini Mariotto3 ; Hellen Nataly Correa Lagos-Guimarães4
; Hellen Nataly Correa Lagos-Guimarães4 ; Andriéllen Marciniak5
; Andriéllen Marciniak5