ABSTRACT
OBJECTIVES: to evaluate the contribution of the Maternal Mortality and Death Surveillance Committee for women of childbearing age (WCA) and maternal mortality in the magnitude of maternal mortality and in the qualification of the causes of death in Recife, Brazil.
METHODS: ex ante/ex post evaluation, ecological, of the annual indicators of mortality of WCA, maternal and case study of declared maternal deaths according to causes of death before and after surveillance. Deaths of WCA (2010 and 2017) were analyzed. The percentage of investigation of deaths of WCA was calculated; their rates and maternal mortality ratio (MMR) were estimated; the groups of causes of death, classification of death, the moment of death, the proportional variation before and after surveillance, and the relocation of the causes after this process were described.
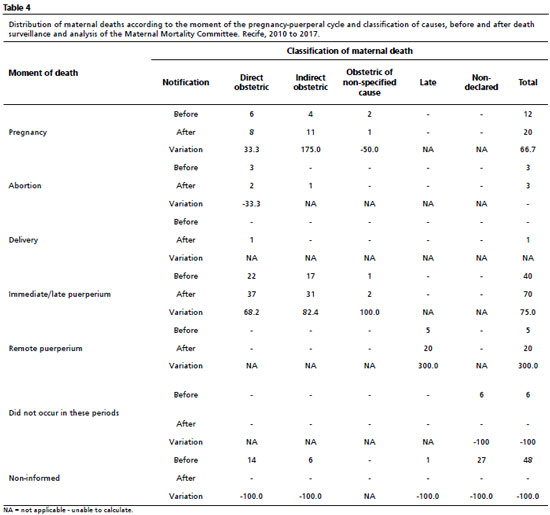
RESULTS: 4.327 (97.0%) of deaths of WCA were investigated (increase of 40.7% of maternal deaths) and MMR of 62.9/100 thousand live births. Improved notifications of immediate/late (75.0%) and remote (300.0%) postpartum; there was a difference in direct obstetric causes, total maternal deaths and late maternal death (p<0.001).
CONCLUSION: the surveillance and the Maternal Mortality Committee showed potential in identifying the magnitude and qualification of causes of maternal death in order to propose the interventions directed to obstetric care.
Keywords:
Maternal mortality, Vital statistics, Mortality registries, Health information systems, Public health surveillance
RESUMO
OBJETIVOS: avaliar a contribuição do Comitê de Mortalidade Materna e da Vigilância do Óbito de mulheres em idade fértil (MIF) e materno na magnitude da mortalidade materna e na qualificação das causas dos óbitos no Recife, Brasil.
MÉTODOS: avaliação ex ante/ex post, ecológico, dos indicadores anuais de mortalidade de MIF, materna e estudo de caso de óbitos maternos declarados segundo causas de morte antes e após a vigilância. Analisaram-se óbitos de MIF (2010-2017) e calculou-se o percentual de investigação; estimaram-se suas taxas e a razão de mortalidade materna (RMM); descreveram-se: grupos de causa, classificação e momento do óbito, variação proporcional antes e após a vigilância/análise do comitê e a realocação das causas após esse processo.
RESULTADOS: investigou-se 4.327 (97,0%) dos óbitos de MIF (incremento de 40,7% das mortes maternas), e RMM de 62,9/100 mil nascidos vivos; melhoraram as notificações do puerpério imediato/tardio (75,0%) e remoto (300,0%); houve diferença nas causas obstétricas diretas, total de óbitos maternos e morte materna tardia (p<0,001).
CONCLUSÃO: mostrou-se o potencial da vigilância e do Comitê de Mortalidade Materna na identificação da magnitude e qualificação das causas de morte materna para proposição de medidas direcionadas aos cuidados obstétricos.
Palavras-chave:
Mortalidade materna, Estatísticas vitais, Registros de mortalidade, Sistemas de informação em saúde, Vigilância em saúde pública
IntroductionMaternal death persists as a global public health problem, besides the decrease of the maternal mortality ratio (MMR) between 1990 and 2015 of 385 deaths to 216 per 100,000 live births (LB), with important differentials among countries.
1 In Brazil, for the year 2017, MMR stood in 64.5/100,000 LB with relevant regional differences, which varied from 38.5 to 88.9/100,000 LB in the North and South regions, respectively. In the same year, Pernambuco portrayed a MMR of 61.3/100,000 LB.
2Trustworthy information on mother deaths due to maternal causes subsidize the implementation of actions focused on the identified problems, improvement on the access and assistance of healthcare and guarantee of sexual and reproductive rights, assured internationally in the Sustainable Development Goals (SDG).
3 However, the underreporting and diminished quality of data on maternal death in information systems restrict their utility in the follow-up of obstetric care and the evolution of these avoidable deaths, impairing the accurate knowledge on magnitude, causes and circumstances of their occurrence, for the planning and management of health actions.
1For the official statistics, the registry of maternal death is conditioned to the report of death causes in the pregnancy-puerperal cycle.
4 In Brazil, the declaration of death (DD), besides notifying the occurrences and causes of death, has a specific field to determine whether the death of women of childbearing age (WCA), 10 to 49 years, occurred or not during pregnancy, abortion, delivery or puerperium.
4Flaws in fulfillment, codification and typing of the DD in the Brazil Mortality Information System (SIM - Portuguese acronym) interfere in the accuracy of maternal death indicators,
5 demanding local and national strategies to expand notification and qualify information on these deaths. Among them, the following stand out: qualification of physicians in the fulfillment of DDs, mainly causes of death; building of encoders of basic death cause; partnership with Death Verification Services and Institutes of Legal Medicine; implementation and strengthening of Maternal Mortality Committees and Surveillance of Maternal Death and Women of Childbearing Age Death.
4-7In Brazil, the structure for identification of the magnitude of this problem has been built since the decade of 1980, when the first Committees were created; the National Committee (1994); the definition of compulsory notification of maternal death (2003) and the epidemiological surveillance as assignment of states and municipalities (2004).
8 The experiences of Committees multiplied in the country, being decisive for the institutionalization of actions of surveillance of maternal death.
4,8In view of the protagonism of women's movement, the visibility of the team and the discussion about reproductive rights had expanded, as well as sexual and reproductive health as an issue of public health in emblematic international conferences.
9With the obligatoriness of investigation of maternal and WCA deaths, in 2008, and the further edition of the Guide of epidemiological Surveillance of Maternal Death, the actions of committees were strengthened.
4 The death surveillance integrated the group of actions of notification, epidemiological investigation and analysis of technical discussion groups and/or committees of death prevention. The Committees are strategies of social control that congregate governmental agencies, civil society and universities, of critical-reflexive, educational and non-punitive performance.
4 The integrated and interdependent action of the Maternal Death Surveillance and the Committee makes it possible the update and correction of data in the strategic information systems, as well as allowing the understanding of problems and circumstances of death, when identifying the access and quality of care provided to women, improving the causes of deaths and indicating their avoidability.
10In Pernambuco, the State Health Secretary (SHS) defined in an ordinance, that all WCA deaths, regardless of the declared cause, transcending ruling national guidelines (investigation of WCA and maternal deaths with presumable cause).
11 Ever since, Recife develops this activities systematically and concentrates the highest population quota of WCA and maternal deaths.
This study aimed to assess the contribution of the Maternal Death Committee and the Surveillance of WCA and maternal Deaths in the magnitude of maternal deaths and in the qualification of the causes of these deaths in Recife, from 2010 to 2017.
MethodsAn evaluative research of ex-ante vs. ex-post type, ecological, descriptive, of annual indicators of WCA and maternal deaths and a case study of declared maternal deaths according to death cases and after the surveillance process.
Information was obtained from the registries of WCA deaths, notified and investigated at SIM; data on the causes of death and the moment of maternal death described in the original DDs before and after the surveillance process, at SIM. The DDs are fulfilled by physicians from health units in which the death occurred or at the necropsy services; registries were encoded and typed in the SIM by the secretaries of health of the municipalities and sent to the regional health facilities, SHS and the Ministry of Health.
4The research was conducted in Recife, a city located in the Northeast Region of Brazil, which had a 0.772 HDI; water supply index of 87% and garbage collection of 98%. In 2017, the estimated population was of 1,629,796 inhabitants, being 526,389 (32.3%) WCA, residing in 94 neighborhoods distributed in eight sanitary districts, exclusively urban. The primary healthcare network had 60% of coverage of the Family Health Strategy (ESF - Portuguese acronym) and had 16 maternity hospitals (seven public and nine private), which performed circa 50 thousand deliveries in this year, being 22,817 live births of women residing in the city, according to Datasus.
The Maternal Death Surveillance of Recife involves death notification, reported at SIM or identified in the investigation of WCA deaths, regardless of the causes described in the DD; epidemiological survey at home, clinics, hospitals that provided care to women in the pregnancy-puerperal cycle and in the necropsy services, by means of researches in the medical records; discussion/analysis in the Committee of Maternal mortality and referral of the guidelines of measures of protection, healthcare and correction of vital statistics to managers.
12The Municipal Committee is composed of representatives of the Regional Medicine and Nursery Councils; of the Women Movement; of Universities and Health and Women Councils. During the reunions for analysis and discussion about deaths, ESF representatives and Community Agents of the area of residence of women are included; of hospitals that provided assistance; managers and technicians of surveillance, primary care, of high and medium complexity and women's health. These reunions occurred after finalization of the investigation of deaths, to reclassify the causes, when necessary, identify the avoidability and adequate measures of intervention.
The universe of WCA and maternal deaths of Recife residents was included, occurring between the pregnancy and one year after delivery, in the period from January 1, 2010 to December 31, 2017, investigated by epidemiological hospital and municipal surveillances, analyzed by the Committee of Maternal Mortality. The inclusion of deaths that occurred up to less than one year after delivery, follows the recommendation of the Committee of Maternal Mortality of Pernambuco (state ordinance of 2017),
12 which expanded the period of identification of maternal deaths due to its extension by means of the development of health technologies. Deaths by sequels of direct obstetric causes were excluded, as well as those by external causes.
The study used the variables:
Investigated WCA Deaths;
Moment of death (pregnancy, abortion, delivery, puerperium, did not occur in these periods, ignored and/or not informed);
Causes of death (sequence of disease causes or morbid state that directly lead to death - part I; other significant conditions that contributed to death, but without direct relation with the chain of causes that lead to death - part II) described by the physician who attested the original DD, and
Basic Cause of Death (disease or lesion that started the chain of pathological events that directly lead to death, or the circumstances of the accident or violence that produced the fatal lesion).
The registries related to the investigations, the deaths and the total population of WCA were collected, respectively, from SIM, in the database of the Federal System, and the Datasus website. The registries of LB were extracted from the state Information Live Birth Information System (Sinasc - Portuguese acronym), with the Tabwin32 software. All registries were exported to Excel
® 2007.
All data from investigated and discussed maternal deaths, which occurred in the same period, were collected from the original DD, archived by the Secretary of Health of Recife, and of SIM from SHS/PE. The registries of the original DD were typed and electronic Excel 2007 spreadsheets, and those from SIM were extracted with the Tabwin32 tool, constituting two distinct databases.
The informed death causes in all lines of part I and II of the original DD before the surveillance, were encoded with the inclusion of basic causes by encoders of the SHS/PE, using the International Classification of Diseases and Related Health Problems - 10
th review (CID-10); and national guidelines about special encodings.
13 The basic causes of death after the conclusion of death surveillance and analysis of the Committee were selected from the database extracted from SIM. For the analysis, the selected codes as basic cause were grouped maintaining the clinical coherence within the same group.
The cause groups were aggregated according to the classification of maternal death: direct obstetric, resulting from obstetrical complications during pregnancy, delivery or puerperium; indirect obstetric, due to existent diseases previous to pregnancy or that developed in this period, aggravated by its physiological effects; obstetric of a non-specified cause, obstetric death whose cause was not determined; late, direct and indirect obstetric causes, occurred after 42 days and less than one year after the end of delivery.
4The percentage of WCA deaths investigation was calculated by the ratio between the investigated subjects and the total occurred; absolute frequencies of maternal deaths were identified with and without the inclusion of the late ones, before and after death surveillance and Committees' analysis by the percentage variation of increase, dividing the difference of obtained values before and after surveillance and Committee's analysis by the value registered before, multiplied by 100, by year and for the studied period.
The MMR was calculated before and after Committees' analysis (absolute number of maternal deaths reported before the process of surveillance and Committee's analysis divided by the total of LB, multiplied by 100 thousand LB); the MMR after surveillance and Committee's analysis (sum of absolute frequency of maternal deaths identified before and after surveillance and Committee's analysis, divided by total of LB, multiplied by 100 thousand LB); the late MMR (sum of absolute frequency of late maternal deaths obtained before and after surveillance and Committee's analysis, divided by the total of LB, multiplied by 100 thousand LB) and MMR added to the late ones (sum of absolute frequency of maternal deaths to the late ones obtained before and after surveillance and Committee's analysis, divided by the total of LB, and multiplied by 100 thousand LV). It was also calculated the mortality rate of WCA, dividing the number of female deaths of childbearing age by the total of WCA, multiplied by 100 thousand WCA.
The percentages of maternal deaths were calculated by cause groups and death classification by means of the ratio between their respective absolute numbers and the total of maternal deaths, before and after the surveillance and Committee's analysis. Absolute frequencies were described, according to the moment and classification of death. The reallocation of maternal deaths was analyzed by groups of cause by the absolute frequency pre and post-process of surveillance and the Committee's analysis.
The methodological support to the execution of statistical analysis concerning the building of confidence intervals and execution of hypothesis tests for difference of proportions is based in Derrick
et al.
14 The statistical calculations were performed using the software library
Partially Overlapping Sample Tests, version 2.0 (12/12/2018) of the R software.
The study was approved by the Research and Ethics Committee of the Institute of Integrative Medicine Prof. Fernando Figueira, under opinion number 2.277.245 from 09/15/2017, with certificate of presentation for ethical appreciation n°: 72815317.4.0000.5201.
ResultsIn the period from 2010 to 2017, 4459 WCA deaths were notified, among which 4327 (97.0%) were investigated, being 93.8% in 2012 and 99.1% in 2015. Maternal deaths passed from 75 to 94 post-surveillance of death and the Committee's analysis, with the percentage difference statistically significant of 0.5 (CI95%=0.3-0.7)
p<0.001. When including the late maternal deaths, the number of notified deaths passed from 81 to 114 after death surveillance and the Committee's analysis, demonstrating statistical significance (
p<0.001) in the percentage difference 0.8 (CI95%=0.6-1.1). There was statistical significance to all isolated years, except 2011 and 2013 (Table 1).
The WCA mortality rate in the study period was 105.4/100 thousand WCA, being the lowest 101.1 (2013) and the highest 114.2/100 thousand (2011). The MMR passed from 41.4 to 51.9 live LB between 2010 and 2017, an increase of 25.3% after death surveillance and Committee's analysis, and for 45.9 (2010); 65.5 (2016) and 43.8 (2017). When included the late maternal deaths, the MMR post-surveillance and Committee's analysis passed from 51.9 to 62.9/100 thousand LB, an increase of 21.3% and for 93.0 (2015) and 65.8 (2017). The late MMR was 11/100 thousand LB in the period, with rates of 16.9 (2015) and 21.9 (2017) post-surveillance and Committee's analysis (Table 2).
The direct obstetric causes increased from 45 deaths to 48 after surveillance and the Committee's analysis, demonstrating statistically significant difference (
p<0.001); the indirect ones did not demonstrate statistical significance, differently from the late maternal deaths, (
p<0.001). Among the 114 maternal deaths identified after surveillance and Committee's analysis, 33 were underreported to SIM, for absence of information on the pregnancy-puerperal cycle in the original DD before the process of surveillance and analysis of death (Table 3). The ranking of death causes before and after surveillance is portrayed in this Table.
70 maternal deaths occurred in the immediate/late puerperium, increase of 75% (82.4% among indirect obstetric causes); 20 in the remote, increase of 300%; 20 in the pregnancy, increase of 66.7% (175% among the indirect ones); three in abortion and one in delivery after death surveillance. The information on the moment of death in the pregnancy-puerperal cycle was retrieved in 54 deaths, six reported as "did not occur in these periods" and 48 without information on the pregnancy-puerperal cycle (Table 4).
Among the 43 indirect obstetric causes, 11 were classified as direct (hypertensive disorders, embolisms, puerperal infection, obstetric hemorrhage, abortion and others); ten not declared as maternal death; two obstetric of non-specified cause and one late maternal, before death surveillance. Among the late ones, 12 are not declared as maternal deaths and three are indirect obstetric. Of the 48 direct obstetric, 28 remained with the same causes post-surveillance; five were classified as indirect obstetric and eight not declared as maternal death. It was specified the cause of two deaths by uterine inertia that were classified as obstetric hemorrhages (Table 5).
DiscussionThe study demonstrated that the surveillance process, including a broad investigation of WCA deaths, analysis and reclassification of causes by the Maternal Mortality Committee, expanded the notification of these deaths, emphasizing the late one and indirect obstetric. This reverberated in the increase of their rates, with a higher magnitude in 2015/2016 and fluctuations in the study period.
The observed difference in the expansion of notification of maternal death up to 42 days after delivery, including the late ones in between 2010 and 2017, ratifies international guidelines about the use of Maternal Death Surveillance and Response Systems and its indication for specifying the causes and associated factors, reducing subregistration and reinforcing measures of intervention.
15 Nevertheless, though the application of confidential inquiries makes robust and complete analyses about maternal deaths possible, the malfunction of vital registries and the little involvement of health professionals with the notification, impair its applicability in less developed regions with high mortality.
16Still, the investigation of nearly all WCA deaths and the review of all obstetric deaths observed in the study were possible due to the decentralized articulation between epidemiological surveillance in hospitals, municipalities and Maternal Death Committees, composing the integrated action of death surveillance. The normative and legal structure, investments in qualification of surveillance professionals and committees built over the years, favored the consolidation of the strategy in Brazil.
4,8We highlight that over one quarter of the total of maternal deaths were identified after the investigation of nearly all WCA deaths (97%), analysis and review of causes. The misclassification of these deaths reduced the notification in the official systems of Mexico (28%) and Taiwan (65%).
17,18 However, in Pernambuco, the under-registration at the state SIM was 48%, 2003,
11 whilst between 2009 and 2011 almost 70% of WCA deaths were investigated
6 with progressive increase in the subsequent years.
The decrease of underreporting of the deaths evaluated in this study and their complications in MMR demonstrate the relevance of the integrated approach between death surveillance and committees. The standardization of the SHS-PE in the 1990 decade
11 favored the development of integrated actions of notification/investigation by the municipalities; analysis and qualification of information by the Committees; and legitimated the social control in the search for intersectoral interventions, performing an important role in the reduction of maternal deaths.
12 Thus, local strategies strengthen vital information systems and contribute with the decision making, influencing changes.
15Almost half of deaths by indirect obstetric causes were wrongly reported as direct and non-declared, revealing the difficulty of the physicians in the recognition and/or registration of pathological effects triggered or aggravated by pregnancy with precision,
7,10 as occurs in countries with restrict socioeconomic development and incomplete or inexistent official systems of registry.
2 In developed countries, underreporting is observed on a smaller scale and is related to imprecisions in the classification of death causes, contributing to systematic biases in the vital registries.
1,19,20 The indefiniteness of the cause is relevant, observing the increase of indirect obstetric deaths in some countries, once it impairs the comprehension of contributive factors, and the observation by cause groups is a clarifying alternative. We highlight that, still not in consensus, there are arguments that signalize that the division of maternal obstetric deaths in direct and indirect became less important, and even misleading in some cases.
19The predominance of specified diseases complicating the pregnancy, delivery and puerperium, observed in this study, demonstrates the influence of women's health condition in the outcome for maternal death. We highlight hypertensive disorders, embolisms, obstetric hemorrhages and diseases of the respiratory tract, which contributed to nearly one third of deaths. Better outcomes in the pregnancy-puerperal cycle can be obtained with the adequate offer of prenatal consultations,
21 whilst the low quality associated with the lack of connection of the pregnant women with the maternity hospital reinforces severe maternal morbidity.
22-24 In addition, unnecessary cesarean section surgeries and low quality of the birth care contribute to the high maternal mortality.
23 The concentration of the mother and child healthcare network in the most developed centers lead to the wandering of pregnant women in search for assistance for delivery, and reflects the deficit in the distribution of obstetric beds and ICU and the weakness of its regulation, recurrent and emergent aspects of the Committees' analyses.
23In the United Kingdom, thrombosis and thromboembolism were the main causes of direct maternal death, hypertensive disorders remained reduced and cardiovascular diseases predominated as indirect cause,
25 whilst in South Africa, HIV infections, obstetric hemorrhages and hypertensive disorders stood out.
26 In countries of low and medium income such as Guatemala, Congo, Kenya, Zambia, India and Pakistan, obstetric hemorrhage, infection related to pregnancy and preeclampsia/eclampsia stood out and corresponded to 83% of mortality.
27 Disparities between maternal death causes of different regions are explained by the level of socioeconomic development, access and quality of health services.
18-20,25-27The increase in late maternal deaths in high income countries signalizes the expansion of survival due to the development of health technologies,
28 in the Americas, the elevation might be consequence of the qualification of the causes by the activities of the Committees, active search and robust information systems in countries such as the United States, Mexico and Brazil.
29 The increase of late deaths post-surveillance found legitimates this presupposition and corroborates the hypothesis of increase of survival by the temporal expansion of the rate.
In this study, over half of late maternal deaths were declared without any mention of relation with the pregnancy-puerperal cycle, still its notification is mandatory by means of specific encoding. The reduced medical accuracy about these deaths and the non-accounting in the calculation of rates contribute to its invisibility.
28Late maternal deaths represent almost one fifth of the deaths and expanded MMR in the study period. Their inclusion in the calculation of the ration influence the indicator, with the possibility of changes in the epidemiological profile of maternal mortality.
29 Observing the relevance, additional information on the original cause, direct or indirect obstetric, need to be identified in order to the analysis of these deaths can contribute with the dimensioning of obstetric risks and adequateness of care.
28 In this way, the recommendation of the Pernambuco Committee
12 promotes the visibility of the problem and stimulates strategies for the reduction of avoidable deaths, questioning the standardizations and national and international ruling practices.
In this study, the puerperal period concentrated 75% of deaths due to indirect and direct obstetric causes, according to what is expected, as occurs worldwide.
30 The specification of the moment of death in the pregnancy-puerperal cycle contributes to the optimization of the network of obstetric health services,
30 although this information had been absent in almost half DDs, corroborating the results of a study conducted with WCA deaths.
5The Committee classified over three quarters of deaths as avoidable or probably avoidable, after analysis of the information and problems of access/and or assistance to healthcare. Thus, over 80% of maternal deaths could be avoided by effective and accessible measures, which is similar to what is observed in poor countries, with life conditions similar to that of many women from Recife.
16 Among the measures of intervention proposed by the Committee, after singular analyses of the maternal deaths, the recommendations concerning prenatal, hospital assistance, birth and postpartum and of the organization of the health system stood out, among others.
Among the limitations, we highlight the difficulties of operationalization, once involving inter-institutional actions; non-usage of methods for validating the cause of death or statistical techniques of concordance and of the correction factor calculation in order to apply to non-investigated deaths. However, the articulation between municipal and hospital surveillance and Committees stood out as an alternative to overcome such restrictions and provided the study with more validity, since it promoted broad investigation of 97% of WCA deaths and 100% of the maternal deaths.
The study demonstrated the potential of death surveillance and the Committee in reducing underreporting, revealing the magnitude and qualifying the causes of maternal deaths, highlighting the indirect and late ones. The findings reinforce the importance of initiatives that strengthen this approach and promote the development of its process, maintaining perennial intersectoral partnerships and strengthening the social control.
References1. Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A,
et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016; 387: 462-74.
2. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Mortalidade Materna no Brasil, 2009-2019. Brasília (DF): Bol Epidemiol. 2021; 52 (29): 13-24. [access in 2022 Fev 20]. Available from:
https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/edicoes/2021/boletim_epidemiologico_svs_29.pdf3. Vanderlei LCM, Frias PG. A vigilância do óbito como instrumento para reduzir a invisibilidade da exclusão social e assistencial de mulheres e crianças. [Editorial] Rev Bras Saúde Matern Infant. 2017; 17 (4): 635-6.
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Análise de Situação em Saúde. Guia de vigilância epidemiológica do óbito materno. Brasília (DF): Ministério da Saúde; 2009. [access in 2022 Fev 20]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_epidem_obito_materno.pdf5. Gil MM, Gomes-Sponholz FA. Declarações de óbitos de mulheres em idade fértil: busca por óbitos maternos. Rev Bras Enferm. 2013; 66 (3): 333-7.
6. Szwarcwald CL, Escalante JJC, Rabello Neto DL, Souza Júnior PRB, Victora CG. Estimação da razão de mortalidade materna no Brasil, 2008-2011. Cad Saúde Pública. 2014; 30 (Supl. 1): S71-S83.
7. Azevedo BAS, Vanderlei LCM, Mello RJV, Frias PG. Avaliação da implantação dos Serviços de Verificação de Óbito em Pernambuco, 2012: estudo de casos múltiplos. Epidemiol Serv Saúde. 2016; 25 (3): 595-606.
8. Jannotti CB, Silva KS, Perillo RD. Vulnerabilidade social e mortalidade materna no mundo e no Brasil. In: Bittencourt S, Dias M, Duarte Mayumi, orgs. Vigilância do óbito materno, infantil e fetal e atuação em comitês de mortalidade. Rio de Janeiro: Fiocruz; 2013. p. 51-89.
9. Thomas TN, Gausman J, Lattof SR, Wegner MN, Kearns AD, Langer A. Improved maternal health since the ICPD: 20 years of progress. Contraception. 2014; 90 (6 Suppl): S32-8.
10. Oliveira CM, Bonfim CV, Guimarães MJB, Frias PG, Medeiros ZM. Mortalidade infantil: tendência temporal e contribuição da vigilância do óbito. Acta Paul Enferm. 2016; 29 (3): 282-90.
11. Alves SV. Maternal mortality in Pernambuco, Brazil: what has changed in ten years? Reprod Health Matters. 2007; 15 (30): 134-44.
12. Pernambuco. Secretaria Estadual de Saúde. Portaria nº 456 de 04 de outubro de 2017. Dispõe sobre a vigilância dos óbitos maternos no âmbito do estado de Pernambuco. Diário Oficial do Estado. Pernambuco; 2017.
13. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde, Coordenação Geral de Informação e Análise Epidemiológica. Protocolos de codificações especiais em mortalidade. Brasília (DF): Ministério da Saúde; 2013. [access in 2022 Fev 20]. Available from:
https://svs.aids.gov.br/daent/cgiae/sim/documentacao/protocolos-codificacoes-especiais-mortalidade.pdf14. Derrick B, Dobson-Mckittrick A, Toher D, White P. Test statistics for comparing two proportions with partially overlapping samples. J Appl Quantitative Methods. 2015; 10 (3).
15. Bandali S, Thomas C, Hukin E, Matthews Z, Mathai M, Dilip TR,
et al. Maternal Death Surveillance and Response Systems in driving accountability and influencing change. Int J Gynecol Obstet. 2016; 135 (3): 365-71.
16. Smith H, Ameh C, Roos N, Mathai M, van den Broek N. Implementing maternal death surveillance and response: A review of lessons from country case studies. BMC Pregnancy Childbirth. 2017; 17 (1): 1-11.
17. Torres LM, Rhenals AL, Jiménez A, Ramírez-Villalobos D, Urióstegui R, Piña M,
et al. Intentional search and reclassification of maternal deaths in Mexico: The effect on the distribution of causes. Salud Publica Mex. 2014; 56: 333-47.
18. Wu TP, Huang YL, Liang FW, Lu TH. Underreporting of maternal mortality in Taiwan: a data linkage study. Taiwan J Obstet Gynecol. 2015; 54 (6): 705-8.
19. Akker TVD, Nair M, Goedhart M, Schutte J, Schaap T, Knight M, on behalf of the Netherlands Audit Committee Maternal Mortality and Morbidity and the UK Confidential Enquiry into Maternal Deaths. Maternal mortality: direct or indirect has become irrelevant. Lancet Glob Health. 2017; 5: e1181-e1182.
20. WHO, UNICEF, UNFPA, World Bank Group, the United Nations Population Division. Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO; 2019.
21. Trost S, Beauregard J, Chandra G, Njie F, Harvey A, Berry J,
et al. Pregnancy-Related Deaths Among American Indian or Alaska Native Persons: Data from Maternal Mortality Review Committees in 36 US States, 2017-2019. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2022. [access in 2023 Jan 23]. Available from:
https://www.cdc.gov/reproductivehealth/maternal-mortality/docs/pdf/Pregnancy-Related-Deaths-AIAN-Data-MMRCs-2017-2019-H.pdf22. Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health. 2016; 13 (Supl. 3): 115.
23. Leal MC, Szwarcwald CL, Almeida PVB, Aquino EML, Barreto ML, Barros F,
et al. Saúde reprodutiva, materna, neonatal e infantil nos 30 anos do Sistema Único de Saúde (SUS). Ciên Saúde Colet. 2018; 23 (6): 1915-28.
24. Marchant T, Boerma T, Diaz T, Huicho L, Kyobutungi C, Mershon CH,
et al. Measurement and accountability for maternal, newborn and child health: fit for 2030? BMJ Glob Health. 2020; 5: e002697.
25. MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK). Saving lives, improving mother's care: Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015-17. Oxford: MBRRACE-UK; 2019. [access in 2023 Jan 23]. Available from:
https://www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202019%20-%20WEB%20VERSION.pdf26. Moodley J, Pattinson RC, Fawcus S, Schoon MG, Moran N, Shweni PM, National Committee on Confidential Enquiries into Maternal Deaths in South Africa. The confidential enquiry into maternal deaths in South Africa: a case study. BJOG. 2014; 121 (4): S53-S60.
27. Pasha O, McClure EM, Saleem S, Tikmani SS, Lokangaka A, Tshefu A,
et al. A prospective cause of death classification system for maternal deaths in low and middle income countries: results from the Global Network Maternal Newborn Health Registry. BJOG. 2018; 125 (9): 1137-43.
28. Sliwa K, Anthony J. Late maternal deaths: a neglected responsibility. Lancet. 2016; 387: 2072-3.
29. De Cosio FG, Jiwani SS, Sanhueza A, Soliz PN, Becerra-Posada F, Espinal MA. Late maternal deaths and deaths from sequelae of obstetric causes in the Americas from 1999 to 2013: a trend analysis. PLoS One. 2016; 11: e0160642.
30. Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR,
et al. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384: 980-1004.
Received on June 30, 2022
Final version presented on April 11, 2023
Approved on April 17, 2023
Associated Editor: Ana Albuquerque
Authors’ contribution: Carvalho PI, Vidal AS, Figueirôa BQ and Frias PG: conceptualization and design, analysis and interpretation of data, critical review of the content of the manuscript.
Oliveira CM, Vanderlei LCM, Pereira CCB and Figueiroa JN: analysis and critical review of the content of the manuscript.
The authors approved the final version of the manuscript and declare no conflict of interest.
 ; Suely Arruda Vidal2
; Suely Arruda Vidal2 ; Barbara de Queiroz Figueirôa3
; Barbara de Queiroz Figueirôa3 ; Lygia Carmen de Moraes Vanderlei4
; Lygia Carmen de Moraes Vanderlei4 ; Conceição Maria de Oliveira5
; Conceição Maria de Oliveira5 ; Cândida Correia de Barros Pereira6
; Cândida Correia de Barros Pereira6 ; José Natal de Figueiroa7
; José Natal de Figueiroa7 ; Paulo Germano de Frias8
; Paulo Germano de Frias8