ABSTRACT
OBJECTIVES: to identify the prevalence and factors associated with breastfeeding in the first hour of a baby's life in Southern Brazil.
METHODS: cross-sectional study with 2.101 births that occurred in a city in the South of the country in 2019, through the application of a questionnaire to puerperal women in the first 48 hours post-partum, containing variables on sociodemographic, clinicals, psychosocial, and obstetric from the pre-gestational period to the immediate post-partum. Univariate analysis was conducted to describe the sample and calculate the prevalence of the outcome. In the bivariate analysis, the chi-square test was used for categorical exposures and the Student's t-test for numericals. For multivariate analysis, a hierarchical reduction model by binary logistic regression (backward elimination) was applied at a significance level of 5%.
RESULTS: 74.2% of the sample carried out was breastfeeding in the first hour of life. There was a statistically significant association between breastfeeding in the first hour of life and birth in a Baby-Friendly Hospital Initiative (BFHI) (p≤0.001) and normal delivery (p≤0.001).
CONCLUSIONS: the results highlight the importance of measuring to still encourage breastfeeding support in the delivery room, especially in cases of cesarean deliveries and conditions that may hinder early initiation of breastfeeding, such as in the maternity hospitals without BFHI.
Keywords:
Breastfeeding, Newborn, Infant care, Perinatal care
RESUMO
OBJETIVOS: identificar a prevalência e os fatores associados ao início precoce da amamentação na primeira hora de vida do bebê no extremo sul do Brasil.
MÉTODOS: estudo transversal com 2.101 nascimentos ocorridos em uma cidade do sul do país em 2019, através da aplicação de questionário às puérperas nas primeiras 48 horas pós-parto, contendo variáveis sociodemográficas, clínicas, psicossociais e obstétricas do período pré-gestacional até o pós-parto imediato. Foi conduzida análise univariada para descrever a amostra e calcular a prevalência do desfecho. Na análise bivariada, o teste qui-quadrado foi utilizado para exposições categóricas e o teste t-Student para as numÉricas. Para análise multivariada, um modelo hierárquico de redução por regressão logística binária (eliminação retrógrada) foi aplicado ao nível de significância de 5%.
RESULTADOS: 74,2% da amostra realizou amamentação na primeira hora de vida. Houve associação estatisticamente significativa entre amamentação na primeira hora de vida com nascer em Iniciativa Hospital Amigo da Criança (IHAC) (p≤0,001) e parto normal (p≤0,001).
CONCLUSÕES: os resultados evidenciam a importância de medidas que incentivem o suporte à amamentação ainda na sala de parto, especialmente em casos de cesarianas e condições que possam dificultar o início precoce do aleitamento, como nas maternidades sem IHAC.
Palavras-chave:
Aleitamento materno, Recém-nascido, Cuidado do lactente, Assistência perinatal
IntroductionBreastfeeding within the first hour of life is announced by the World Health Organization (WHO) as one of the recommendations to be followed immediately after birth.
1 According to WHO, newborns without complications should be skin-to-skin contact with their mothers and encouraged to be breastfed during the first hour of life, with the aim of promoting exclusive breastfeeding and reducing neonatal mortality. Studies show that breastfeeding within the first hour after birth can reduce neonatal mortality by up to 13%.
2 This is an important public health issue, especially in Brazil, whereas more than half of deaths of children under one year of age occur in the neonatal period.
2Breastfeeding in the first hour contributes in establishing exclusive breastfeeding.
3,4,5 It has been observed that, shortly after birth, newborns are more apt to spontaneously seek the nipple region and begin breastfeeding, as the baby is more active and awake before the first sleep.
5 In addition, suckling stimulates the secretion of the hormones prolactin and oxytocin, which induce milk production and ejection. These hormones contribute to the continuity of breastfeeding and the reduction of stress caused by childbirth, assisting in uterine contraction, preventing hemorrhage, and stimulating protective behaviors, facilitating bonding.
3,6,7 Breastfeeding in the first hour after birth also helps prevent hypothermia and stabilizes the newborn's cardiorespiratory function,
5 besides in reducing infant morbidity from respiratory infections and diarrhea.
6,8The practice is part of Step 4 of the Baby-Friendly Hospital Initiative (BFHI), which recommends postponing routine procedures to ensure continuous and direct skin-to-skin contact.
9,10 Despite the widely recognized benefits, data show that less than half of the newborns worldwide begin breastfeeding within the first hour of life.
10,11 The highest prevalence of breastfeeding in the first hour of life is associated with normal delivery,
12,13,14 being born in a BFHI,
12 having adequate prenatal care,
15 birth weight greater than 2500g,
15 APGAR greater than 7,
15 and skin-to-skin contact.
13,16International studies show great variability in the prevalence of the practice, ranging from 9.1%
17 to 92.6%,
18 reflecting cultural, institutional, and health policy differences. Although biological and institutional factors are often explored, there is a lack of data on social, cultural, and psychological aspects—including the influence of maternal anxiety—on early breastfeeding.
19,20,21 In this context, the present study aims to identify the prevalence and factors associated with breastfeeding in the first hour of life in two hospitals in Southern Brazil.
MethodsData were obtained from a larger study entitled "
Estudo Perinatal" (Perinatal Study) a cross-sectional census study conducted in the city of Rio Grande, in the Southern part of the country, on the coast between the Mirim and Patos lakes and the Atlantic Ocean. The economy of the city is centered on commerce, agribusiness, fishing activities, and fertilizer industries. The city has an estimated population of 191,000 inhabitants and has two general hospitals, one of which is 100% linked to the
Sistema Único de Saúde (SUS)(Public Health System), and the other with two hospital buildings, one public and one private.
Between 2007 and 2019, perinatal surveys were conducted in Rio Grande (RS) every three years to assess pregnancy, childbirth, and post-partum care. These population-based studies, were conducted by using standardized methodology, including all births that occurred in the city over a full year and investigated clinical, psychosocial, and obstetric aspects from the pre-gestational period to the immediate post-partum period. Unlike the routine on information systems, such as the
Sistema de Informações sobre Nascidos Vivos (Sinasc)(Live Birth Information System), the survey provided more detailed primary data, allowing the aspects of analysis to not be routinely captured. In addition, periodic survey allowed monitoring of trends in various indicators related to maternal and child health over time.
22The present study analyzed data from the 2019 survey. To be included in the study, mothers had to reside in the urban or rural area of the city, and newborns had to weigh 500 grams or more, or have a minimum gestational age of 20 weeks. The data were collected from a standardized questionnaire administered to post-partum women, face-to-face, while still in the hospital, within the first 48 hours after childbirth, between January 1 and December 31, 2019. A total of 2,314 deliveries were performed during this period.
The questionnaire was administered during visits, including weekends, to the maternity, by previously trained interviewers. Daily, they verified the previous day of births through medical records, and eligible post-partum women were interviewed. Tablets were used to apply the questionnaires through the REDCap (Research Electronic Data Capture) application.
The questionnaire covered sociodemographic and psychosocial variables and obstetric medical history. The variables used to describe the sample were: maternal age, schooling, skin color, marital status, family income, perception of paternal support during pregnancy, symptoms of anxiety, smoking during pregnancy, alcohol consumption during pregnancy, parity, type of childbirth, planned pregnancy, prenatal consultations, information on breastfeeding, APGAR at 5
th minute, and childbirth in BFHI.
The outcome variable was breastfeeding in the first hour of life. Data were collected through the question "How many hours after birth did you breastfeed your baby?" The answer to the question was recorded numerically, and the variable was subsequently operationalized in dichotomous form. The categories were defined as follows: "Within one hour of the baby's life" and "More than one hour of life."
The overall construct on anxiety was assessed using the General Anxiety Disorder-7 (GAD-7) instrument, which was validated for the Portuguese language by Moreno
et al.
21 A careful and standardized application of the GAD-7 in the perinatal period aims to better understand the relation between maternal anxiety and early breastfeeding, since it is an instrument that assesses anxiety symptoms and has been widely used in scientific research due to its brevity and reliability and because it is self-administered. It consists of seven questions with a Likert scale ranging from zero to three, where zero means "never" and three means "almost every day." The total score ranges from zero to 21, measuring the frequency of signs and symptoms of anxiety in the last two weeks. A score of 10 or higher indicates a positive result for signs and symptoms of anxiety disorders.
Regarding data processing, double entry and database review were performed using SPSS version 18.0. [SPSS Inc. Released in 2009. PASW Statistics for Windows, version 18.0. Chicago: SPSS Inc.]. Qualitative variables were described as absolute (n) and relative (n%) frequencies, and intragroup comparisons were made using the chi-square test with adjusted residual analysis.
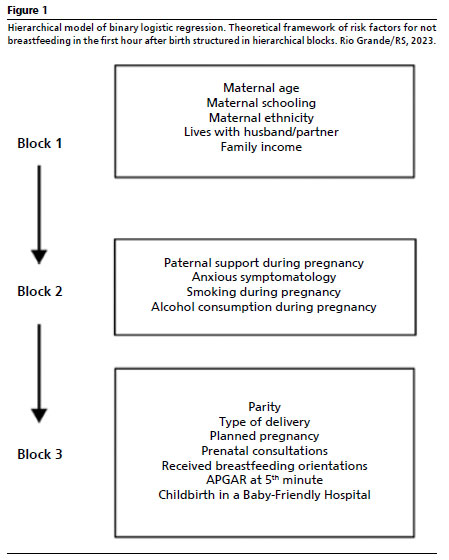
Multivariate analysis was performed using logistic regression, based on a hierarchical analysis model (Figure 1), using the backward selection process and considering a
p-value ≤0.20 to maintain the variables in the model. As a summary of the variation in the proportion of non-breastfeeding in the first hour after childbirth is explained by the model, the coefficients were calculated, the final regression coefficient (B), odds ratio (OR), and 95% confidence interval (95% CI). The significance level adopted for all analyses was set at 5%.
This study was approved by the
Comitê de Ética em Pesquisa na área da Saúde (CEPAS) (Ethics Committee on Health Research) of the
Universidade Federal do Rio Grande (FURG), under the number 278/2018, CAAE: 03488918.4.0000.5324, on December 19, 2018.
Figure 1 shows the hierarchical binary logistic regression model. Theoretical framework of risk factors for not breastfeeding in the first hour after childbirth structured in hierarchical blocks.
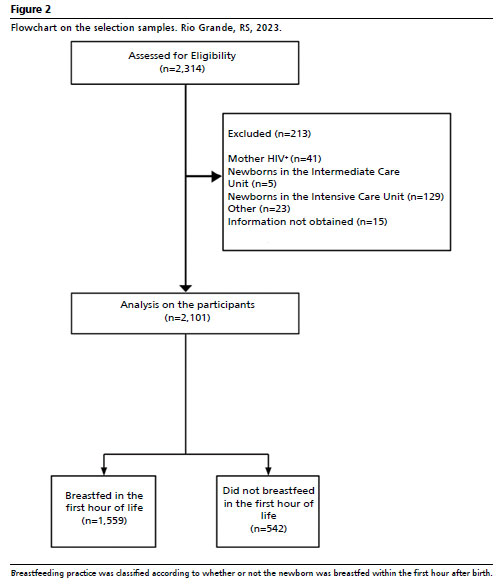
ResultsA total of 2,314 childbirths were delivered in 2019. In the study sample, 213 (9.2%) were excluded due to complications that prevented breastfeeding in the first hour after birth: mothers diagnosed with HIV (n=41), newborns admitted to intermediate care units (n=5), newborns admitted to intensive care units (n=129), and other reasons (n=23). There were also exclusions due to lack of access to the necessary information (n=15 losses). Thus, 2,101 births were included in the final analyses, classified as breastfed newborns (n=1,559, 74.2%) or newborns not breastfed (n=542, 25.8%) in the first hour after childbirth (Figure 2).
Sociodemographic characteristics are presented in Table 1. Younger maternal ages (up to 25 years) were associated with breastfeeding in the first hour after childbirth (49.6%), while ages between 26 and 35 years were associated with non-breastfeeding in the first hour after childbirth (52.8%) (chi-square test,
p≤0.001). Maternal schooling up to elementary was associated with breastfeeding in the first hour after childbirth (38.4%), while those with at least a higher education were associated with not breastfeeding in the first hour after childbirth (35.1%) (chi-square test,
p≤0.001). A higher proportion of self-declared black mothers breastfed in the first hour after childbirth (9.2%), while white mothers did not (81.5%) (chi-square test,
p=0.007). Mothers who did not live with a husband/partner had a higher proportion of breastfeeding in the first hour after childbirth (15.9%), while those who lived with a husband/partner did not (91.5%) (chi-square test,
p≤0.001). When categorizing family income (in US dollars) into tertiles, the lowest tertile was associated with breastfeeding in the first hour after childbirth (41%), while the highest tertile was associated with not breastfeeding in the first hour after childbirth (50.8%) (chi-square test,
p≤0.001).
The maternal and obstetric characteristics of the participants are described in Table 2. Breastfeeding in the first hour of life was associated with several factors. Mothers who reported good or very good paternal support during pregnancy had a higher frequency of early breastfeeding compared to those with regular or unsatisfactory support (
p=0.015). The presence of symptoms on generalized anxiety disorder was associated with a lower occurrence of breastfeeding in the first hour (
p=0.041), while smoking during pregnancy was negatively associated with the practice (
p≤0.001).
Fewer than six prenatal consultations were also associated with a lower prevalence of breastfeeding in the first hour (
p≤0.001), as was the absence of pregnancy planning (
p≤0.001). The type of delivery was one of the most strongly associated factors: vaginal deliveries had a higher frequency of early breastfeeding, while cesarean sections were associated with a lower prevalence (
p≤0.001). Similarly, deliveries performed in hospitals accredited as Baby-Friendly favored early breastfeeding (
p≤0.001); mothers who handled their babies while still in the delivery room had higher rates of breastfeeding in the first hour (
p≤0.001).
Most smoking mothers were multiparous (87.7%) (chi-square test,
p≤0.001), had vaginal deliveries (63.1%) (chi-square test,
p≤0.001), gave birth in BFHI (77.9%) (chi-square test,
p≤0.001), had a reduced number of prenatal consultations (22.6%) (chi-square test,
p≤0.001), did not plan their pregnancy (79.9%), and had schooling level up to elementary school (61.1%) (chi-square test
, p≤0.001) (data not shown).
Regression models were performed for non-breastfeeding in the first hour after childbirth and associated factors, excluding variables less associated with the outcome. A final hierarchical model was produced by multiple logistic regressions (conducted in three blocks) and is illustrated in Figure 1. Statistical data (beta coefficient, odds ratio, 95% confidence intervals, and
p-values) from the final model are presented in Table 3. In summary, cesarean section and non-delivery in BFHI was increased by 11,705 (95% CI = 8,512–16,096) and 9,820 (7,501 – 12,857) times, respectively, the chance of not breastfeeding in the first hour after childbirth (hierarchical binary logistic regression reduction model,
p≤0.001 for both) (Table 3).
DiscussionThis study identified that 74.2% of the mothers breastfed in the first hour of their baby's life, and that the observational evidence corroborates the findings of other studies, in cesarean delivery
13,14 and not being born in BFHI
12 were the most consistent factors associated with not breastfeeding in the first hour of life.
WHO in global initiatives, aims to increase exclusive breastfeeding rates by 2030, focusing on children's health and positive impacts on the economy and society. The goals include at least 70% of the mothers breastfeeding within the first hour of life.
10 The present study showed a prevalence of over 70%, in line with WHO recommendations.
National and international studies have revealed large disparities in the prevalence of breastfeeding in the first hour of life. Asian and African countries had lower rates compared to American and European countries. The lowest prevalence was found in a prospective cohort study of 695 mothers residing in Jiangyou, China.
17 Although breastfeeding in the first hour of life was only 9%, the frequency of prenatal classes on breastfeeding and encouragement from BFHI hospital staff were factors associated with the initiation of breastfeeding shortly after delivery.
The highest prevalences were observed in Europe and the United States: 92.6% in a study conducted in the city of Viseu, Portugal;
18 88.2% in a study conducted in Spain and a hospital in Ireland,
16 85% in the city of Oulu, Finland,
23 and 70.2% in Querétaro, Mexico.
24 It is noteworthy that one of the studies with the highest prevalence rate recorded in Brazil, reached 79.5%, and was conducted in the Triple Frontier region.
25 Vaginal delivery was identified as a protective factor for breastfeeding in the first hour in several of these studies, as well as in this study.
The results of a study conducted in Pelotas, in the South of Brazil,
26 confirm the findings of this research, demonstrating the existence of an association between being born in a BFHI and early breastfeeding. This study revealed that for newborns born in maternities that do not adopt BFHI, the risk of not breastfeeding in the first hour increased 42%. In addition, not breastfeeding in the first hour increased the risk of not exclusively breastfeeding at one month of age (RR=1.24,
p=0.01). Lower prevalence rates of early breastfeeding were also found, 48.6% of the newborns breastfed within the first hour in BFHI, compared to 31.7% in other maternities.
A relevant fact is the possible improvement in the prevalence of breastfeeding in the first hour in the State of Rio Grande do Sul in recent years, since the current study obtained a significantly higher prevalence (74.2%) compared to studies conducted more than a decade ago in the cities of Pelotas
26 (37.8%) and Porto Alegre
27 (52%).
In the sample studied, the percentage of women who attended higher education or post graduate courses was low, with only 21.7% had graduated from higher education, which is also consistent with the family income ranges of the puerperal women in the study. Although it was expected that women with higher levels of education would have more information about breastfeeding and would have higher prevalences of breastfeeding in the first hour, as demonstrated in Araújo
et al.
13 research, this study showed the opposite: lower levels of schooling are associated with early breastfeeding. As a result of additional analyses between schooling, childbirth at BFHI or not, and type of delivery, the hypothesis raised for this finding was that women with lower levels of schooling had more normal childbirths and had more of their babies in BFHIs, which have intensified the training of teams to instruct on breastfeeding and respect for the
Hora de Ouro14 (Golden Hour). It is also important to note that 66.3% of the sample had given birth in BFHI in the present study.
In the bivariate analysis, the puerperal women with symptoms of anxiety were less likely to breastfeed in the first hour of life, but this association lost significance in the multiple analysis. A systematic review conducted in 2022 by Yuen
et al.
20 showed mixed results: some studies showed that breastfeeding reduces the risk of post-partum anxiety, while others did not identify such a reduction, showing the necessity further studies to better clarify this association.
Although 70.2% of the puerperal women reported not receiving information about breastfeeding during prenatal care, there was no significant association with the outcome. This result is similar to an Indian study
28 with 150 puerperal women, where only 26% started breastfeeding in the first hour, despite 71.3% had received prenatal guidance. This may indicate that it is necessary to improve the quality of counseling and invest in health education policies to impact breastfeeding during the
Hora de Ouro.
Other studies
13,14 have revealed that women who undergo cesarean sections are at greater risk of not breastfeeding early, a finding that was also identified in the present study. This may be attributed to the early separation between the mother and baby, often associated with cesarean sections, as demonstrated by the national survey
Nascer Brasil,
14 (Born Brazil) which pointed to high rates of early separation in these situations. It is essential to ensure support for breastfeeding in the first hour, especially for mothers who have had a cesarean section, promoting a successful start in breastfeeding.
The father's support as "excellent" was more frequently reported in cesarean deliveries, indicating its potential to promote early breastfeeding in this type of delivery. Investing in parental involvement can compensate for a lower rate of breastfeeding in the first hour in cesarean sections, deconstructing the idea that breastfeeding is exclusively the mother's responsibility.
The findings of this study reinforce the necessity to overcome persistent barriers in breastfeeding in the first hour of life, even in BFHI certified institutions. Brazilian studies indicate that in many maternities, including accredited ones, hospital routines still hinder the full experience of the
Hora de Ouro.14 In a survey of 415 mother-baby pairs in Natal, RN, more than half of the newborns received infant formula in the first hour of life, often without a physician's prescription.
29 Another study in the State of Paraíba revealed that only 9.3% of the puerperal women were able to maintain continuous skin-to-skin contact for more than 30 minutes, as recommended.
30An important limitation of this study was the absence of specific data on the duration and effectiveness of skin-to-skin contact, which made its main analysis unfeasible. In addition, the cross-sectional design prevents the inference of causality between variables. Most of the evidence reviewed is observational in nature and has methodological limitations, which reinforces the urgency for more robust primary studies in the perinatal context. Nevertheless, as it was conducted before the COVID-19 pandemic, the study contributes as a baseline for future comparative analyses.
In selecting the literature, priority was given to local studies with similar perinatal outcomes to ensure comparability. The national study
Nascer Brasil was included as a complementary reference with national coverage.
14The association between birth in a Baby-Friendly Hospital and early breastfeeding was significant, highlighting the effectiveness of practices such as Step 4 of BFHI. Although 66.3% of the births in the study occurred in accredited hospitals, the data point to the need to expand these practices to private and non-BFHI hospitals.
Despite regional advances, indicators are still below WHO targets. Childbirth in non-BFHIs and cesarean sections were associated with early non-breastfeeding. Strengthening policies to promote breastfeeding, especially for births outside BFHIs and cesarean sections, is essential to improve care, guarantee rights, and promote the physical and emotional health of the mother-baby dyad.
References1. World Health Organization (WHO). WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: WHO; 2018. [
Internet]. [access in 2022 Abr 22]. Available from:
https://www.who.int/publications/i/item/97892415502152. Silva OLO, Rea MF, Sarti FM, Buccini G. Cost-effectiveness analysis of Baby-Friendly Hospital Initiative in promotion of breast-feeding and reduction of late neonatal infant mortality in Brazil. Public Health Nutr. 2021 Jun; 24 (8): 2365-75.
3. Moberg KU, Handlin L, Petersson M. Neuroendocrine mechanisms involved in the physiological effects caused by skin-to-skin contact - with a particular focus on the oxytocinergic system. Infant Behav Dev. 2020 Nov; 61: 101482.
4. Widstrom AM, Wahlberg V, Matthiesen AS, Eneroth P, Uvnas-Moberg K, Werner S,
et al. Short-term effects of early suckling and touch of the nipple on maternal behaviour. Early Hum Dev. 1990; 21 (3): 153-63.
5. Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016 Nov; 11 (11): CD003519.
6. Ministério da Saúde (BR). Secretaria de Atenção à Saúde, Departamento de Ações Programáticas Estratégicas. Bases para a discussão da Política Nacional de Promoção, Proteção e Apoio ao Aleitamento Materno. Brasília (DF): Ministério da Saúde; 2017. [access in 2022 Abr 22]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/bases_discussao_politica_aleitamento_materno.pdf 7. Norholt H. Revisiting the roots of attachment: a review of the biological and psychological effects of maternal skin-to-skin contact and carrying of full-term infants. Infant Behav Dev. 2020 Ago; 60: 101441.
8. Organização Mundial da Saúde (OMS), Fundo das Nações Unidas para a Infância (UNICEF). Iniciativa Hospital Amigo da Criança: revisada, atualizada e ampliada para o atendimento integrado: módulo 1: histórico e implantação. Brasília (DF): Ministério da Saúde; 2008. [access in 2022 Abr 24]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/iniciativa_hospital_amigo_crianca_modulo1.pdf9. Neczypor JL, Holley SL. Providing Evidence-Based Care During the Golden Hour. Nurs Women's Health. 2017; 21 (6): 462-72.
10. Melo DS, Oliveira MH, Pereira DS. Progressos do Brasil na proteção, na promoção e apoio do aleitamento materno sob perspectiva do Global Breastfeeding Collective. Rev Paul Pediatr. 2021; 39: e2019296.
11. North K, Gao M, Allen G, Lee AC. Breastfeeding in a Global Context: Epidemiology, Impact, and Future Directions. Clin Ther. 2022 Feb; 44 (2): 228-44.
12. Paredes HDMT, Pontes JS, Mourão RG, Almeida MFL, Capelli JCS. Prevalência da amamentação na primeira hora de vida: uma revisão sistemática. Rev Saúde Redes. 2021; 6 (3): 223-33.
13. Araújo KEAS, Santos CC, Caminha MFC, Silva SL, Pereira JCN, Filho MB. Contato de pele com pele e o início precoce da amamentação: um estudo transversal. Texto Contexto Enferm. 2021; 30: e20200621.
14. Gomes MASM, Esteves-Pereira AP, Bittencourt SDA, Augusto LCR, Lamy-Filho F, Lamy ZC,
et al. Atenção hospitalar ao recém-nascido saudável no Brasil: estamos avançando na garantia das boas práticas? Ciên Saúde Colet. 2021; 26 (3): 859-74.
15. Pereira CRVN, Fonseca VM, Oliveira MIC, Souza IEO, Mello RR,
et al. Avaliação de fatores que interferem na amamentação na primeira hora de vida. Rev Bras Epidemiol. 2013; 16 (2): 525-34.
16. Martín-Arribas A, Vila-Candel R, O'Connell R, Dillon M, Vila-Bellido I, Beneyto MÁ,
et al. Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study. Int J Environ Res Public Health. 2020 Nov; 17 (22): 8394.
17. Tang LP, Binns CW, Lee AH, Pan X, Chen S, Yu C. Low prevalence of breastfeeding initiation within the first hour of life in a rural area of Sichuan Province, China. Birth. 2013; 40 (2): 134-42.
18. Ferreira M, Vaz T, Aparício G, Duarte J. OC20 – Skin-to-skin contact in the first hour of life. Nurs Children Young People. 2016; 28 (4): 69-70.
19. Pérez-Escamilla R, Tomori C, Hernández-Cordero S, Baker P, Barros AJD, Bégin F,
et al. Breastfeeding: crucially importnt, but increasingly challenged in a Market-driven world. Lancet. 2023; 401 (10375): 472-85.
20. Yuen M, Hall OJ, Masters GA, Nephew BC, Carr C, Leung K, et al. The Effects of Breastfeeding on Maternal Mental Health: Systematic Review. J Womens Health (Larchmt). 2022 Jun; 31 (6): 787-807.
21. Moreno AL, De Sousa DA, Souza AMFLP, Manfro GG, Salum GA, Koller SH,
et al. Factor structure, reliability, and item parameters of the brazilian-portuguese version of the GAD-7 questionnaire. Temas Psicol. 2016; 24 (1): 367-76.
22. Cesar JA, Mendoza-Sassi RA, Marmitt LP. Evolução da assistência à gestação e ao parto no extremo sul do Brasil. Rev Saúde Pública. 2021; 55: 50.
23. Hakala M, Kaakinen P, Kääriäinen M, Bloigu R, Hannula L, Elo S. The realization of BFHI Step 4 in Finland - Initial breastfeeding and skin-to-skin contact according to mothers and midwives. Midwifery. 2017 Jul; 50: 27-35.
24. Río GF, Paredes-Melesio N. Impact of early initiation of breastfeeding on exclusive breastfeeding. Ginecol Obstet Méx. 2022; 90 (7): 551-8.
25. Netto A, Spohr FA, Zilly A, França AFO, Rocha-Brischiliari SC, Silva RMM. Amamentação na primeira hora de vida em uma instituição com Iniciativa Hospital Amigo da Criança. Ciênc Cuid Saúde. 2016; 15 (3): 515-21.
26. Silva MB, Albernaz EP, Mascarenhas MLW, Silveira RB. Influência do apoio à amamentação sobre o aleitamento materno exclusivo dos bebês no primeiro mês de vida e nascidos na cidade de Pelotas, Rio Grande do Sul, Brasil. Rev Bras Saúde Mater Infant. 2008; 8 (3): 275-84.
27. Abdala LG, Cunha MLC. Contato pele a pele entre mãe e recém-nascido e amamentação na primeira hora de vida. Clin Biomed Res. 2019; 38 (4): 356-60.
28. Ananthakrishnan S, Kasinathan B, Sounderrajan P. Antenatal counseling for breast feeding - Are we doing it the right way?. Curr Pediatr Res. 2012; 16: 142-4.
29. Pinheiro JMF, Menêzes Flor TB, Mata AMB, Pires VCC, Oliveira LIC, Barbosa WPM,
et al. Prevalência da oferta de complemento alimentar para o recém-nascido. Rev Bras Saúde Mater Infant. 2021; 21 (3): 869-78.
30. Sampaio ARR, Bousquat A, Barros C. Contato pele a pele ao nascer: um desafio para a promoção do aleitamento materno em uma maternidade pública "Amiga da Criança" do Nordeste do Brasil. Rev Epidemiol Serv Saúde. 2016; 25 (2): 281-90.
Authors' contributions: Teixeira DCL: manuscript planning, literature review, data analysis, and manuscript writing; Santos DB: co-supervision of the manuscript and manuscript writing; Corrêa ML: data analysis and manuscript writing; Garcia MO: literature review and manuscript tables; Prietsch SM: research guidance and supervision of manuscript writing. All authors approved the final version of the article and declare no conflict of interest.
Data Availability: The entire data set supporting the results of this study has been published in the article itself.
Received on February 19, 2024
Final version presented on April 28, 2025
Approved on May 5, 2025
Associated Editor: Karla Bomfim
 ; Daniela Barsotti Santos2
; Daniela Barsotti Santos2 ; Mariana Lima Corrêa3
; Mariana Lima Corrêa3 ; Mariana de Oliveira Garcia4
; Mariana de Oliveira Garcia4 ; Silvio Omar Macedo Prietsch5
; Silvio Omar Macedo Prietsch5