ABSTRACT
OBJECTIVES: to determine the incidence of peri-intraventricular hemorrhage (PIVH) and the risk factors in newborns weighing <1,500 g and/or gestational age <33 weeks.
METHODS: a prospective cohort type study on premature newborns admitted to the type II neonatal intensive care unit at the Sistema Único de Saúde (SUS) (Public Health System) from January/2019 to December/2022. The dependent variable was PIVH, with determination of its incidence and associated risk factors. The project was approved by the Research Ethics Committee.
RESULTS: a total of 503 neonates participated and the incidence of PIVH was 32.4%. The risk factors were: immediate clamping of the umbilical cord (p=0.017; RR= 1.089; 95%CI=1.015-1.167), vaginal delivery (p=0.001, RR= 1.110; 95%CI= 1.041-1.183) and surfactant use (p<0.001; RR= 1.163; 95%CI= 1.092-1.239).
CONCLUSION: the incidence of PIVH was high and was associated with immediate clamping of the umbilical cord, vaginal delivery and surfactant use, risk factors that can be modified by good perinatal care practices.
Keywords:
Cerebral intraventricular hemorrhage, Infant premature, Umbilical cord clamping, Pulmonary surfactant-associated proteins
RESUMO
OBJETIVOS: determinar a incidência de hemorragia peri-intraventricular (HPIV) e os fatores de risco em recém-nascidos com peso <1.500 g e/ou idade gestacional <33 semanas.
MÉTODOS: estudo do tipo Coorte prospectiva de recém-nascidos pré-termo admitidos em unidade de terapia intensiva neonatal tipo II do Sistema Único de Saúde no período de janeiro/19 a dezembro/2022. A variável dependente foi HPIV, com determinação de sua incidência e fatores de risco associados. O projeto foi aprovado pelo Comitê de Ética em Pesquisa.
RESULTADOS: participaram 503 neonatos e a incidência de HPIV foi 32,4%. Os fatores de risco identificados foram: clampeamento imediato do cordão umbilical (p=0,017; RR= 1,089; IC95%= 1,015-1,167), parto vaginal (p=0,001, RR= 1,110; IC95%= 1,041-1,183) e uso de surfactante (p<0,001; RR= 1,163; IC95%= 1,092-1,239).
CONCLUSÃO: a incidência de HPIV foi elevada e esteve associada a clampeamento imediato do cordão umbilical, parto vaginal e uso de surfactante, fatores de risco que podem ser modificados por boas práticas de assistência perinatal.
Palavras-chave:
Hemorragia cerebral intraventricular, Recém-nascido prematuro, Clampeamento imediato do cordão umbilical, Proteínas associadas a surfactantes pulmonares
IntroductionThe central nervous system (CNS) has a region called the germinal matrix, which is richly vascularized, with a large number of neuronal and glial cells. The small blood vessels in the germinal matrix form an immature vascular network. Fluctuations in cerebral blood flow caused by conditions such as anemia, hypoglycemia, asphyxia and abrupt rises in systemic blood pressure leaving the CNS prone to congestion and stasis, increasing cerebral venous pressure, causing peri-intraventricular hemorrhage (PIVH). This condition usually occurs in premature infants and is multifactorial: the presence of vulnerable vessels, hemodynamic alterations, inflammatory mediators, genetic predisposition, and among others.
1The incidence of PIVH increases when gestational age (GA) is less, and is more frequent in patients younger than 32 weeks and with a birth weight of less than 1500g. Studies show that immediate clamping in these premature infants (< 30 seconds), the use of surfactant and vaginal delivery increase the risk of PIVH.
2-5 Gestational hypertension and the use of prenatal magnesium sulphate also decrease this risk.
6,7The first classification of PIVH was written by Papile
8 in 1978, where it was divided into grades I, II, III and IV. The one most used today is the one published by Volpe
9 in 1989, in which there was a change regarding to grade IV. Grades I and II are considered milder conditions, while grade III and ventricular hemorrhage with associated hemorrhagic infarction (formerly grade IV) are more serious, with a higher risk of death and negative neurodevelopmental outcomes.
9Regarding clinical presentation, most patients are asymptomatic. Therefore, for diagnosis, it is necessary to perform a transfontanellar ultrasound (TFUS) early, in the first week of life. In a survey of severe PIVH cases (grade III and IV),
10 in Brazil and worldwide, between 2007 and 2013, the frequency of cases was similar. In Brazil, around 10% of premature newborns (PTNBs) have grade III and IV PIVH,
11 as in Spain and Canada. In Israel, 12% of hemorrhage cases were classified as more severe.
12 In more recent studies in Brazil, between 2013 and 2018, cases of severe PIVH were around 32.2%.
13Due to the importance of this morbidity and the negative neurological outcomes associated with its occurrence,
14 the aim of this study was to determine the incidence of PIVH in PTNBs in a type II neonatal intensive care unit (NICU) at the
Sistema Único de Saúde (SUS) (Public Health System) in the Northeast of Brazil, as well as to identify risk factors associated with its occurrence. Carrying out this research will help track cases better and reinforce preventive care and proper management of these children, in an attempt to avoid complications and promote the best quality of life, without compromising neurodevelopment.
MethodsThis was a prospective cohort study of newborns (NB) admitted to the NICU at a high-risk maternity hospital in the city of Natal - RN, in the Northeast of Brazil, from January 2019 to December 31, 2022. It has 20 beds, is classified as type II and attends exclusively for SUS patients. Patients were followed from the moment of birth until the final outcome (discharge, transfer to another hospital unit or death).
The inclusion criteria were PTNBs with a GA of less than 33 weeks and/or a birth weight of less than 1,500g. The cut-off point adopted for gestational age and birth weight was based on the higher morbidity and mortality seen in these groups at the institution where the research was carried out.
The exclusion criteria were: carriers of congenital infections (STORCH: syphilis, toxoplasmosis, rubella, cytomegalovirus and herpes, as well as arboviruses, HIV and Sars-Cov 2 infection), major congenital malformations and/or chromosomopathies, genetic syndromes, inborn errors of metabolism, non-performance of TFUS during hospitalization and coming from other services more than 24 hours after birth. Major congenital malformations are those that have medical and/or social implications and generally require surgical treatment or have an increased risk of death due to the severity and complexity of the malformation.
15The dependent variable was PIVH according to Volpe's classification
9 in 1989, as shown in Table 1.
The diagnosis was made by means of TFUS performed using Philips Affiniti 50 ultrasound equipment, with a Linear L12-4 transducer (4 - 12 MHz). The tests were carried out at the patient's bedside in the NICU by two doctors, ultrasonographers from the institution with specific training to carry out such tests and extensive experience in the field. The first TFUS was carried out in the first week of life and the following tests were carried out at intervals according to the results of the first test, or when there was clinical suspicion of intracranial bleeding.
The independent maternal variables analyzed were: maternal age; prenatal care and number of visits; type of pregnancy (single or multiple); presence of hypertensive syndromes and diabetes during pregnancy; use of antenatal corticosteroids, with number of doses administered; use of magnesium sulphate for neuroprotection.
The neonatal variables analyzed were: route of delivery (cesarean or vaginal); time of ruptured pouch; time of umbilical cord clamping, considered immediate when performed < 30 seconds, according to the
Sociedade Brasileira de Pediatria;
16 (Brazilian Society of Pediatrics) sex of the NB; GA and birth weight; classification of weight in relation to GA using the Intergrowth-21
st Project curves.
17 Participants were classified as small for GA when their weight was less than the 10th percentile for GA; neonatal resuscitation and Apgar score in the 1
st and 5
th minute of life; axillary temperature in the first hour of life; use of intra-tracheal surfactant for respiratory distress shortly after birth and inspired oxygen fraction greater than 30%; analysis of the occurrence of infections, according to criteria defined by the
Agência Nacional de Vigilância Sanitária (ANVISA)(National Health Surveillance Agency), which are considered early when they manifest in the first 48 hours of life and late when they occur after this period;
18 pulmonary hemorrhage (PH): presence of blood in the orotracheal tube associated with the need to increase ventilatory parameters and/or hemodynamic support;
19 patent ductus arteriosus: patent ductus arteriosus with flow on echocardiogram after 72 hours of life, a diagnosis made by the pediatric cardiologists at the institution using GE's Vivid I echocardiogram machine (all NBs with symptoms such as the presence of a heart murmur, pulmonary hemorrhage, tachycardia, wide pulses, signs of congestive heart failure, hypotension and the need to use vasoactive drugs were assessed for this morbidity); use of vasoactive drugs in the first week of life.
Descriptive analysis was carried out using the mean, standard deviation (Mean ± SD), absolute and relative frequencies. Point estimates with 95% confidence intervals were used to calculate the incidence of PIVH. The Student's t-test for independent samples was applied to continuous variables with a normal distribution. The homogeneity of variances was checked using Levene's test. In the presence of heterogeneity of variances, Welch's t-test was applied. The chi-square test was used to analyze the association between categorical variables.
For results that showed significance in the t-test, Cohen's d effect size was calculated by dividing the mean difference by the standard deviation of the difference. The values were assessed according to Cohen's scale: up to 0.19 = negligible; between 0.20 and 0.39=small; between 0.40 and 0.79=moderate and ≥0.80=large. The effect size for significant associations was assessed by calculating the Relative Risks (RR) and respective 95% Confidence Intervals (95%CI) using robust Poisson regression. The robust Poisson regression model was also used in the multivariate analysis. The initial model was adjusted for the independent variables that showed a significance level ≤0.20 in the bivariate analysis.
In a second adjustment stage, variables with a
p-value of <0.10 were selected. For the final model, equidispersion assumptions were checked and the quality of the fit was assessed using the Wald chi-square test, Deviance analysis and the ROC curve. The variables selected were those with significant associations (
p<0.05). A 5% significance level was adopted for all analyses. The software used for the analyses was SPSS (Statistical Package for the Social Sciences, Chicago, USA), version 28.0.
The study was approved by the Research Ethics Committee at the hospital, CAAE: 11177019.7.0000.5292, and by the Teaching and Research Management.
ResultsIn the period studied, 647 NB were admitted with a GA of less than 33 weeks and/or a birth weight of less than 1500g. The following were excluded: 21 because they were admitted to the service more than 24 hours after birth; 12 due to a diagnosis of genetic syndromes (trisomies 13, 18 and 21, Cri Du Chat syndrome and Jarcho Levin syndrome); 27 with a diagnosis of severe congenital malformations; six with STORCH-type congenital infections; one with lysosomal storage disease and three guardians refused to take part. A total of 74 babies did not undergo TFUS and could not be included in the study. Therefore, the final sample consisted of 503 participants.
The incidence of IVH found was 32.4%, corresponding to 163 patients (95%CI= 28.3%-36.5%). Bleeding was classified as mild (I or II) and severe (III or IVHF with associated venous infarction) in 74.2% (121) and 25.8% (42), respectively. The average GA and birth weight were 29.5 weeks ±2.5 and 1251 grams ±385, respectively. The average follow-up time for patients until the final outcome was 56.05 ± 32.27 days (Table 2).
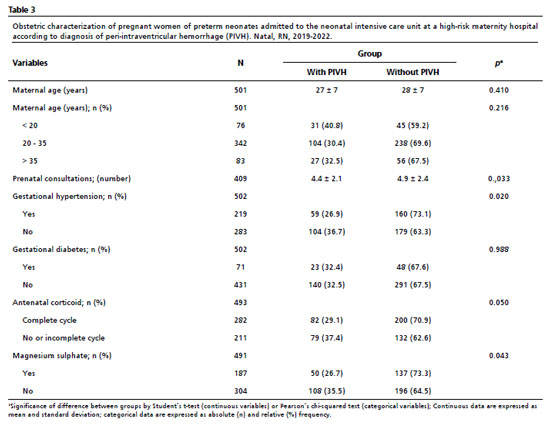
Comparing the group of NBs with and without hemorrhage, it was found that mothers who had been diagnosed with hypertensive syndromes in pregnancy and received two doses of antenatal corticosteroids and magnesium sulfate for neuroprotection had a lower incidence of PIVH. The number of prenatal consultations was lower for the group of patients diagnosed with PIVH (4.4 ± 2.1) compared to the group of neonates not diagnosed with PIVH (4.9 ± 2.4), a statistically significant difference (Table 3).
PIVH was also associated with vaginal delivery, immediate clamping of the umbilical cord, neonatal resuscitation, Apgar less than 7 in the first and fifth minute of life, use of mechanical ventilation, use of surfactant and vasoactive drugs in the first week of life, pulmonary hemorrhage and Persistent Patent Ductus Arteriosus (PDA). On the other hand, the use of nasal CPAP (Continuous Positive Airway Pressure) in the delivery room proved to be a protective factor against the occurrence of this morbidity. The GA at birth was lower for the group of patients diagnosed with PIVH (28.8 ± 2.8) compared to the group of neonates without this diagnosis (29.9 ± 2.4),
p<0.01. Birth weight was also lower for the group of patients diagnosed with PIVH (1.194 ± 408) compared to the neonates group without the diagnosis (1.279 ± 371), a statistically significant difference,
p=0.020 (Table 4).
The multivariate regression model was not statistically significant by the Omnibus test (
p=0.089), however, by analyzing the Deviance and ROC Curve, the model showed an acceptable fit (Deviance/Grades of freedom = 0.145; Area under the curve = 67.2%). The results indicated an increased risk of PIVH in neonates with an umbilical cord clamping time of < 30 seconds (RR = 1.09; 95%CI = 1.02-1.17), who used surfactant (RR = 1.16; 95%CI = 1.09-1.24) and who were born by vaginal (RR = 1.11; 95%CI = 1.04-1.18), all with
p<0.05 (Table 5).
DiscussionIn this present study, the incidence of PIVH in premature infants was high compared to the national average. However, the frequency of more severe hemorrhages was lower and morbidity was more common in patients with lower gestational age and birth weight.
A national study using data from the
Rede Brasileira de Pesquisa Neonatal (Brazilian Neonatal Research Network), carried out between 2013 and 2018
13 showed that 30.4% of patients had PIVH, ranging from mild to severe. The severe form was diagnosed in 32.2%, a high incidence with an increasing trend over the years in a population with an average gestational age of 29 weeks and an average weight of 1,085 grams. The occurrence of bleeding was also higher in patients with lower gestational ages and birth weights (28 weeks and 815 grams).
The risk factors that remained associated with PIVH in the multivariate analysis were: immediate umbilical cord clamping (< 30 seconds), the use of surfactant and vaginal delivery compared to cesarean section.
In the literature, we have seen that timely umbilical cord clamping (>30 seconds in premature NBs under 34 weeks of gestational age, according to the recommendations of the
Programa de Reanimação Neonatal da Sociedade Brasileira de Pediatria)
16 (Neonatal Resuscitation Program of the Brazilian Society of Pediatrics) brings benefits for the patient, as it increases the transfer of blood from the cord to the NB, increasing hematocrit levels and preventing early anemia. In addition, immediate clamping decreases intravascular volume, favoring cerebral hypoperfusion.
2 For this reason, it is recommended that in premature infants under 34 weeks, clamping be performed between 30 seconds and one minute of life. However, for this to happen, it is necessary for the NB to have good vitality at birth, characterized by the presence of regular breathing and good muscle tone, which sometimes does not occur in premature infants under 34 weeks, especially those who did not receive prenatal corticosteroids.
20,21 In the institution studied, the pediatricians in the delivery room are trained periodically with neonatal resuscitation courses, indicating that the care provided to newborns is adequate. However, many premature newborns are not born with good vitality and in these situations there is a need for immediate umbilical cord clamping according to national guidelines.
16Many extreme preterm infants have respiratory distress syndrome (RDS), and the main treatment recommended is the use of surfactant to recruit pulmonary alveoli, associated with ventilatory support (invasive or not). However, despite its benefits, one of the side effects is hemorrhage, such as PIVH and pulmonary hemorrhage.
3 Many of the PTNB <33 weeks in the unit studied received at least one dose of surfactant. It is important to note that in the institution where the research was carried out, surfactant is administered primarily through orotracheal intubation (InSurE-Intubate Surfactant Extubate technique), and minimally invasive techniques such as MIST (Minimally Invasive Surfactant Therapy) are not routinely used. With the InSurE technique, the patient is intubated to administer the medication, after which they must be extubated, but the risk of keeping the patient intubated is greater, causing harm due to the invasive ventilation time.
22Recent studies have shown that using a less invasive technique to administer surfactant, such as MIST, reduces the need for invasive ventilation, reduces the length of hospital stay and is less likely to develop pulmonary bronchodysplasia and severe PIVH. The MIST technique consists of using a thin endotracheal catheter, introduced into the trachea under direct visualization through the laryngoscope. This catheter is then removed after administration of the medication. Throughout the procedure, the patient has a nasal prong with positive pressure in non-invasive ventilation and maintains spontaneous breathing.
22It has also been shown that the route of delivery contributes to the occurrence of PIVH. There are controversial results in the scientific literature; some authors have also found the same result with an increased risk of PIVH in PTNBs born vaginally, but with no association with more severe bleeding. Vaginal delivery favors the rupture of the NB's vessels, and in an elective cesarean delivery this risk would be lower. However, the best route of delivery should always take into account the risk of maternal complications, as well as the risks to the fetus.
4,5,23Minimum or essential handling protocols, especially in the first 72 hours of life, have been indicated as a neuroprotective strategy and to reduce the risk of PIVH.
24,25 These protocols, are known as bundles, generally include: maintaining the supine position and head in a neutral position, avoiding painful and stressful procedures, aspirating the tracheal tube only if there is excessive secretion/obstruction, arterial catheterization in addition to venous catheterization in those with a birth weight of <1,000g (for the administration of medication and to avoid repeated punctures for test collection), not collecting cerebrospinal fluid, essential manipulation and care bundling. Bundles are a set of good practices, such as those listed above, and are used in NB care. It is a low-cost solution that contributes to improving the quality of care.
26 The studies showed that the use of these care measures was effective in reducing cases of PIVH, but that there is still a need for continuing education for the team caring for the NB, emphasizing the importance of this care and that these are simple actions that can be adopted and maintained.
For the management of children diagnosed with PIVH, it is recommended to: maintain adequate mean arterial perfusion; oxygenation and ventilation according to the condition; adequate water support, metabolic and nutritional support; treat seizures in timely manner to avoid hypoxia or hypotension; continuous surveillance with TFUS for early detection of post-hemorrhagic ventricular dilation to assess the need for ventricular shunt.
27Severe PIVH is considered harmful to the child's neurological development, and can delay the achievement of developmental milestones, and compromise speech, hearing and vision, and among others. For this reason, follow-up with the multidisciplinary team after hospital discharge is very important.
28By evaluating the results of this longitudinal study, we can contribute to changes in the care of premature patients, in order to provide better quality care, reducing prenatal risk factors, increasing the use of corticosteroids for example, and controlling postnatal risk factors such as the use of ventilatory support with protective strategies, the administration of surfactant in a less invasive way and with stress and pain control and the timely umbilical cord clamping.
29With regard to limitations, the study was single-center, but with a large sample size and prospectively constructed. Some approaches could not be well analyzed, such as the use of vasoactive drugs, for example, which in the literature and in our statistical analysis is associated with an increased risk of PIVH,
30 but the indications for their use were not well documented, compromising the evaluation of data for future interventions, with the aim of improving care.
In conclusion, we would like to point out that the incidence of PIVH was high. The risk factors identified for its occurrence are similar to those described in the literature and can be minimized through bundles of care for the premature infant including timely umbilical cord clamping, prevention of hypothermia, application of good practices in vaginal delivery or indication of cesarean delivery in cases of extreme prematurity, considering the associated maternal risks and protocol for indication and administration of tracheal surfactant, preferably through minimally invasive techniques and with adequate management of stress and pain during the procedure.
References1. Tsao PC. Pathogenesis and Prevention of Intraventricular Hemorrhage in Preterm Infants. J Korean Neurosurg Soc. 2023 May; 66 (3): 228238.
2. Hemmati F, Sharma D, Namavar Jahromi B, Salarian L, Farahbakhsh N. Delayed cord clamping for prevention of intraventricular hemorrhage in preterm neonates: a randomized control trial. J Matern Fetal Neonatal Med. 2022 Oct; 35 (19): 3633-9.
3. Abdel-Latif ME, Davis PG, Wheeler KI, De Paoli AG, Dargaville PA. Surfactant therapy via thin catheter in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database Syst Rev. 2021 May; 5 (5): CD011672.
4. Costa STB, Costa P, Graça AM, Abrantes M; Portuguese National Registry of very low birth weight infants. Delivery Mode and Neurological Complications in Very Low Birth Weight Infants. Am J Perinatol. 2024 Jul; 41 (9): 1238-44.
5. Zahedi-Spung LD, Raghuraman N, Macones GA, Cahill AG, Rosenbloom JI. Neonatal morbidity and mortality by mode of delivery in very preterm neonates. Am J Obstet Gynecol. 2022 Jan; 226 (1): 114.e1-114.e7.
6. Nakamura N, Ushida T, Nakatochi M, Kobayashi Y, Moriyama Y, Imai K,
et al. Neonatal Research Network of Japan. Mortality and neurological outcomes in extremely and very preterm infants born to mothers with hypertensive disorders of pregnancy. Sci Rep. 2021 Jan 18; 11 (1): 1729.
7. Moradi Y, Khateri R, Haghighi L, Dehghani S, Hanis SM, Valipour M,
et al. The effect of antenatal magnesium sulfate on intraventricular hemorrhage in premature infants: a systematic review and meta-analysis. Obstet Gynecol Sci. 2020 Jul; 63 (4): 395-406.
8. Papile L, Burstein J, Burstein R, Koffler H, Albuquerque NM. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infantes with birth weights less than 1,500 gm. J Pediatr. 1978 Abr; 92 (4): 529-34.
9. Volpe JJ. Intraventricular hemorrhage and brain injury in the premature infant. Diagnosis, prognosis, and prevention. Clin Perinatol. 1989 Jun; 16 (2): 387-411.
10. Huang J, Wang Y, Tian T, Zhu T, Tang J, Gao Q,
et al. Risk factors for periventricular-intraventricular haemorrhage severity in preterm infants: a propensity score-matched analysis. BMC Pediatr. 2023 Jul; 23 (1): 341.
11. Guinsburg R, Almeida MF, Castro JS, Silveira RC, Caldas JP, Fiori HH,
et al. Death or survival with major morbidity in VLBW infants born at Brazilian neonatal research network centers. J Matern Fetal Neonatal Med. 2016 Mar; 29 (6): 1005-9.
12. Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M,
et al.; International Network for Evaluating Outcomes (iNeo) of Neonates. Neonatal Outcomes of Very Low Birth Weight and Very Preterm Neonates: An International Comparison. J Pediatr. 2016 Oct; 177: 144-52.e6.
13. Vinagre LEF, Caldas JPS, Marba STM, Procianoy RS, Silveira RC, Rego MAS,
et al. Temporal trends in intraventricular hemorrhage in preterm infants: A Brazilian multicenter cohort. Eur J Paediatr Neurol. 2022 Jul; 39: 65-73.
14. Lee JH, Noh OK, Chang YS; Korean Neonatal Network. Neonatal Outcomes of Very Low Birth Weight Infants in Korean Neonatal Network from 2013 to 2016. J Korean Med Sci. 2019 Jan 28; 34 (5): e40.
15. Chimah OU, Emeagui KN, Ajaegbu OC, Anazor CV, Ossai CA, Fagbemi AJ,
et al. Malformações congênitas: Prevalência e características dos recém-nascidos internados no Centro Médico Federal de Asaba. Saúde Sci Rep. 2022 Abr; 5 (3): e599.
16. Rugolo LMSS, Anchieta LM, Oliveira RCS. Recomendações sobre o clampeamento do cordão umbilical. Programa de Reanimação Neonatal da Sociedade Brasileira de Pediatria. 2022 Mar 17. [access in 2023 Dez 2]. Available from:
https://www.sbp.com.br/fileadmin/user_upload/23396c-Diretrizes-Recom_Clamp_CordUmb.pdf17. INTERGROWTH-21st - International Fetal and Newborn Growth Consortium for the 21
st Century. 2009-2024. [access in 2023 Dez 2]. Available from:
http://intergrowth21.ndog.ox.ac.uk/pt18. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária (ANVISA). Critérios diagnósticos de infecção associada à assistência à saúde Neonatologia. Série Segurança do Paciente e Qualidade em Serviços de Saúde. 2
nd ed. Brasília (DF): Ministério da Saúde; 2017. [access in 2023 Dez 2]. Available from:
https://www.gov.br/anvisa/pt-br/centraisdeconteudo/publicacoes/servicosdesaude/publicacoes/caderno-3-criterios-diagnosticos-de-infeccao-associada-a-assistencia-a-saude-neonatologia.pdf/view.19. Aziz A, Ohlsson A. Surfactant for pulmonary haemorrhage in neonates. Cochrane Database Syst Rev. 2020; 2 (2): CD005254.
20. Morhart P, Gärtner J, Weiss C, Stumpfe FM, Dammer U, Faschingbauer F,
et al. Influence of Timing of Antenatal Corticosteroid Administration on Morbidity of Preterm Neonates. In Vivo. 2022 Jul-Aug; 36 (4): 1777-84.
21. Howes A, Hilditch C, Keir A. What clinical practice strategies have been shown to decrease incidence rates of intraventricular haemorrhage in preterm infants? J Paediatr Child Health. 2019 Oct; 55 (10): 1269-78.
22. Gupta BK, Saha AK, Mukherjee S, Saha B. Minimally invasive surfactant therapy versus InSurE in preterm neonates of 28 to 34 weeks with respiratory distress syndrome on non-invasive positive pressure ventilation-a randomized controlled trial. Eur J Pediatr. 2020 Aug; 179 (8): 1287-93.
23. Gamaleldin I, Harding D, Siassakos D, Draycott T, Odd D. Significant intraventricular hemorrhage is more likely in very preterm infants born by vaginal delivery: a multi-centre retrospective cohort study. J Matern Fetal Neonatal Med. 2019 Feb; 32 (3): 477-82.
24. Poryo M, Boeckh JC, Gortner L, Zemlin M, Duppré P, Ebrahimi-Fakhari D,
et al. PROGRESS study consortium and NGFN - Nationales Genomforschungsnetz Deutschland. Ante-, peri- and postnatal factors associated with intraventricular hemorrhage in very premature infants. Early Hum Dev. 2018 Jan; 116: 1-8.
25. Zhao Y, Zhang W, Tian X. Analysis of risk factors of early intraventricular hemorrhage in very-low-birth-weight premature infants: a single center retrospective study. BMC Pregnancy Childbirth. 2022; 22 (1): 890.
26. Ferreira DM, Girão ALA, Siebra e Silva AV, Chaves EMC, de Almeida PC, Freire VS,
et al. Application of a Bundle in the Prevention of Peri-Intraventricular Hemorrhage in Preterm Newborns. J Perinat Neonatal Nurs. 2020 Apr/Jun; 34 (2): E5-E11.
27. Kochan M, Leonardi B, Firestine A, McPadden J, Cobb D, Shah TA,
et al. Elevated midline head positioning of extremely low birth weight infants: effects on cardiopulmonary function and the incidence of periventricular-intraventricular hemorrhage. J Perinatol. 2019 Jan; 39 (1): 54-62.
28. Alotaibi WSM, Alsaif NS, Ahmed IA, Mahmoud AF, Ali K, Hammad A,
et al. Reduction of severe intraventricular hemorrhage, a tertiary single-center experience: incidence trends, associated risk factors, and hospital policy. Childs Nerv Syst. 2020 Dec; 36 (12): 2971-9.
29. Yeo KT, Thomas R, Chow SS, Bolisetty S, Haslam R, Tarnow-Mordi W, Lui K; Australian and New Zealand Neonatal Network. Improving incidence trends of severe intraventricular haemorrhages in preterm infants <32 weeks gestation: a cohort study. Arch Dis Child Fetal Neonatal Ed. 2020 Mar; 105 (2): 145-50.
30. Abdul Aziz AN, Thomas S, Murthy P, Rabi Y, Soraisham A, Stritzke A,
et al. Early inotropes use is associated with higher risk of death and/or severe brain injury in extremely premature infants. J Matern Fetal Neonatal Med. 2020 Aug; 33 (16): 2751-58.
Acknowledgements: We would especially like to thank the newborns' parents for signing the informed consent form, allowing us to carry out the study.
Authors' contribution: Sousa DAS and Barreto ACNG: conception and design of the study, data collection, filling in the spreadsheets, analysis and interpretation of the results, writing and critical revision of the content of the manuscript. Ferreira PLM: statistical analysis of the data, analysis and interpretation of the results, writing and critical revision of the content of the manuscript. Camargo JDAS: design of the research methodology, statistical analysis of the data, analysis and interpretation of the results, writing and critical revision of the content of the manuscript.Silveira SLA: research design, writing and critical revision of the content of the manuscript. All the authors have approved the final version of the article and declare no conflicts of interest.
Received on May 13, 2024
Final version presented on November 29, 2024
Approved on December 3, 2024
Associated Editor: Lygia Vanderlei
 ; Pedro Lucas de Morais Ferreira2
; Pedro Lucas de Morais Ferreira2 ; Juliana Dantas de Araújo Santos Camargo1
; Juliana Dantas de Araújo Santos Camargo1 ; Sarah de Lima Alloufa da Silveira1
; Sarah de Lima Alloufa da Silveira1 ; Anna Christina do Nascimento Granjeiro Barreto1
; Anna Christina do Nascimento Granjeiro Barreto1