ABSTRACT
OBJECTIVES: to determine the clinical and epidemiological profile of the long post-COVID syndrome (LPCS) and the quality of life among female survivors compared to males after hospitalization for COVID-19 in the city of Recife, Brazil.
METHODS: a prospective cohort study analyzed demographic and clinical data during hospitalization, as well as LPCS and the quality of life questionnairewhereasdata was collected by telecare at three, sixand 12 months after hospital discharge. Logistic regression was used to explore the association between variables and each dimension of the questionnaire.
RESULTS: 887 patients were included. At the end of three, sixand 12 months, women were more frequently reported with LPCS (p<0.001). Regarding quality of life, women tended to worsen over time in all domains compared to men: mobility domain (28.4% versus 9.3%, p<0.05), personal care (14.8% versus 5.6%; p<0.05), usual activities (30.8% versus 13.1%, p < 0.05), pain/discomfort (29% versus 16.9%, p<0.05) and anxiety/depression (43.8% versus 33.3%, p<0.05).
CONCLUSION: the frequency of LPCS increased and the quality of life worsened with both genders until the first year after hospital discharge, especially in women.
Keywords:
Long post-covid syndrome, Quality of life, Female
RESUMO
OBJECTIVES: to determine the clinical and epidemiological profile of the long post-COVID syndrome (LPCS) and the quality of life among female survivors compared to males after hospitalization for COVID-19 in the city of Recife, Brazil.
METHODS: a prospective cohort study analyzed demographic and clinical data during hospitalization, as well as LPCS and the quality of life questionnairewhereasdata was collected by telecare at three, sixand 12 months after hospital discharge. Logistic regression was used to explore the association between variables and each dimension of the questionnaire.
RESULTS: 887 patients were included. At the end of three, sixand 12 months, women were more frequently reported with LPCS (p<0.001). Regarding quality of life, women tended to worsen over time in all domains compared to men: mobility domain (28.4% versus 9.3%, p<0.05), personal care (14.8% versus 5.6%; p<0.05), usual activities (30.8% versus 13.1%, p < 0.05), pain/discomfort (29% versus 16.9%, p<0.05) and anxiety/depression (43.8% versus 33.3%, p<0.05).
CONCLUSION: the frequency of LPCS increased and the quality of life worsened with both genders until the first year after hospital discharge, especially in women.
Palavras-chave:
Long post-covid syndrome, Quality of life, Female
IntroductionThe acute infection caused by severe acute respiratory syndrome coronavirus 2 (SARS Cov2-), which causes coronavirus disease 2019 (COVID-19), has constituted a serious pandemic, with more than 775 million confirmed cases and seven million deaths worldwide by March 31, 2024.
1 However, many of the survivors have reported persistence of symptoms beyond 12 weeks of acute onset, without an alternative diagnosis, which characterizes the long post-COVID syndrome (LPCS).
2One year after acute infection, COVID-19 survivors still had lower health status than matched non-COVID-19 controls, for age, sex, comorbidities,
3,4 the severity of the acute disease and female patients have been the main risk factors for the development of the syndrome.
4 Women and presence of high blood pressure were the main factors associated with LPCS.
5Even after one year, approximately 20% of patients have reported significant worsening in their quality of life.
2 Matched COVID-19 survivors at 12 months had more problems with mobility, pain or discomfort, and anxiety or depression, and had more prevalent symptoms than the controls.
3 Anxiety and depression have been the main clinical problems identified in the quality of life of patients with LPCS.
2Brazilian LPCS patients have been evaluated in different scenarios. Fatigue, dyspnea, arthralgia, and depression/anxiety were the most prevalent symptoms identified after 12 months.
6,7 However, the clinical profile of LPCS and the quality of life until the period of one year need to be better evaluated in developing countries like Brazil to determine the clinical and epidemiological profile of LPCS and the quality of life among female survivors compared to males.
The frequency of long post-COVID syndrome and its impact on the quality of life need to be assessed by genders in COVID-19 survivors who were hospitalized. Therefore, this study aims to compare the clinical and epidemiological profiles of female and male survivors and determine their quality of life at three, six, and twelve months after hospital discharge. The study was conducted at a reference hospital for COVID-19 diagnosis and treatment in Recife, Pernambuco, Brazil.
MethodsThis prospective study analyzed data of clinical and quality of life of patients discharged between April 2020 to May 2021 at a reference hospital created for diagnosis and treatment of COVID-19 cases in the city of Recife, State of Pernambuco, Brazil, the
Hospital de Campanha Aurora (HCA), with 100 Intensive Care Unit (ICU) beds and 60 ward beds.
Patients were included in this cohort if they were 18 years or older, discharged after hospitalization, confirmed positive for COVID-19 by real-time polymerase chain reaction testing (RT-PCR SARS-CoV-2) Patients were followed up to one year after discharge and were dichotomized into two groups by sex: female and male patients. Pregnant and postpartum patients were excluded.
The following demographic data and epidemiological and clinical variables were assessed: age, ethnicity (categorized into white, mixed, black and others), level of schooling (categorized into illiterate, up to elementary school, up to high school or college/university); marital status (dichotomized as single [divorced, unmarried, widowed] versus married [married, living with partner]), comorbidities (Hypertension, diabetes, lung disease, obesity, kidney disease and asthma); Smoking was assessed by never smoked, former smokers and current smokers. Frequency of ICU admissions, use of mechanical ventilation, vasopressors and hemodialysis were also collected.
The recommendations of STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) were used as reference.
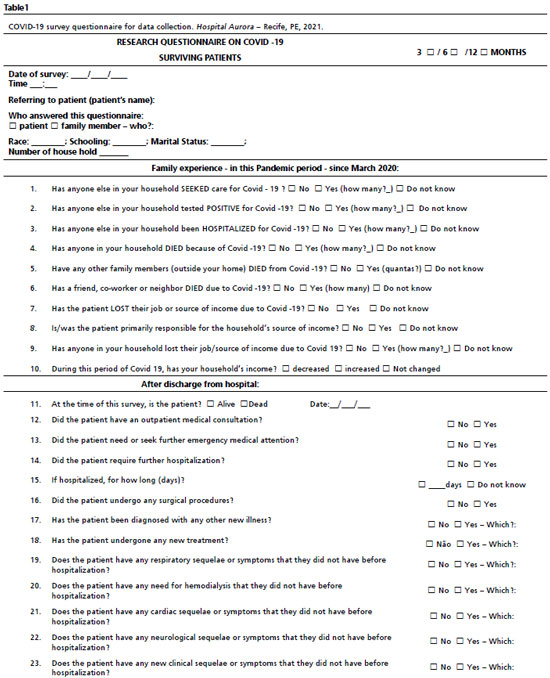
All patients after discharge were invited to participate in this study. patients were assessed at three, six, and 12 months after discharge by teleconsultations to collect updated clinical data and quality of life questionnaire. Patients who informed some new symptoms more than 12 weeks and had not been before hospitalized by COVID-19 were considered having LPCS. Patients or their relatives were accepted as responders. Teleconsultations were done by one of four different health professionals among nurses or physiotherapists after specific training. The telephone interview was conducted using the same standard questionnaire (Table 1).
The main analysis was the quality of life assessed by the EuroQol five-dimension three-level (EuroQol 5D-3L) questionnaire. EQ-5D-3L questionnaire to assess health-related quality of life, the EQ-5D-3L descriptive system comprises the following five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has 3 levels: 1-no problem, 2-some problem, and 3-extreme problem. The sum of 2 and 3 levels was used to determine the frequency of each domain altered. A Brazilian Portuguese version was requested by the
Sociedade Pernambucana de Combate ao Câncer-SPCC with screening number 36973 was granted by EuroQol on July 30
th, 2020.
8Data were analyzed using SPSS version 28.0 and only valid data were considered. A descriptive analysis of the study population was performed using mean and standard deviation measures for continuous variables and absolute and relative frequency distributions for categorical variables. The
t-test was used to compare continuous variables and the chi-square test was performed to compare categorical variables. Logistic regression analysis was used to explore the association among variables and each dimension of EQ-5D-3L, with an emphasis on older patients. Variables that showed an association with outcomes in univariate analyses, exhibiting values of
p<0.15, were sequentially tested in a multivariate model. Variables with
p<0.05 were considered statistically significant in the multiple models.Differences were considered significant when
p<0.05.
The ethics committee of the
Hospital do Cancer de Pernambuco analyzed and approved this research (CAAE: 35243120.7.0000.5205).
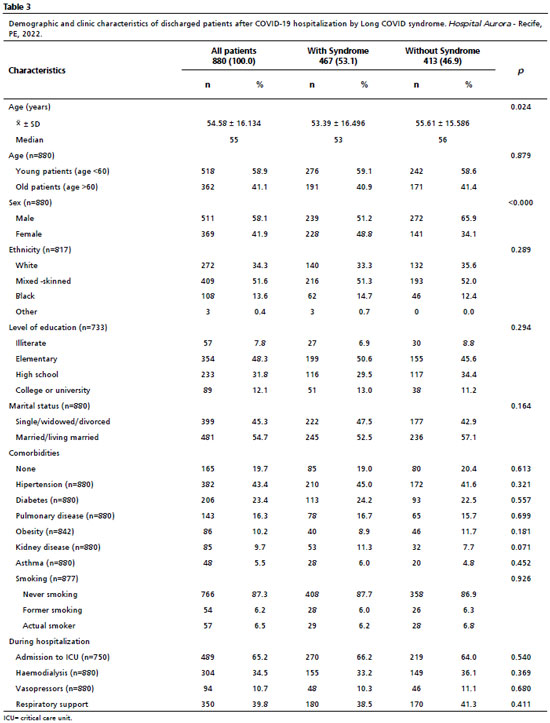
ResultsIn this study, 1,204 patients were discharged after hospitalization with RT-PCR positive for SARS-COV-2 from HCA between April 2020 and May 2021. Three hundred and seventeen patients were excluded because the follow-up data were not completely collected. At the end of 3, 6 and 12 months, 635, 395 and 184 patients were completely evaluated by EQ-5D-3L, respectively. Thus, 887 different patients were included in this study. The mean age of the participants was 54.58 + 16.13 years old. Most patients were male (58.1%), self-reported as mixed colored skin (51.6%), were young, less than 60 years old (58.4%), had attended elementary school (48.2%) and were mainly admitted to the intensive care unit (ICU) (65.2%). Regarding comorbidities, 80.4% of the patients reported some comorbidity: systemic arterial hypertension (SAH) was the most frequent 43.5%, followed by diabetes mellitus (DM) in 23.3% and chronic lung disease in 16.2%. During hospitalization, most patients were admitted to the ICU environment (65.2%), where the use of vasoactive drugs was 10.9%, use of invasive mechanical ventilation was 39.8%, and the use of hemodialysis, in 34.8% of the cases. LPCS was identified in 53.1% of patients (Table 2 and 3).
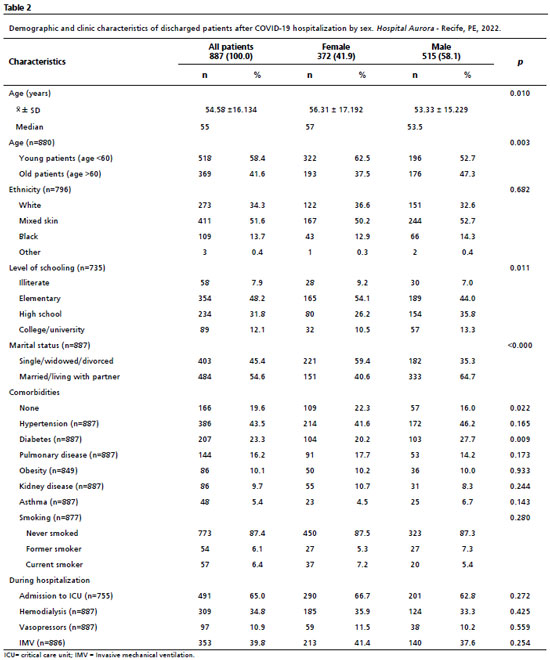
Compared to men, women (41.9%) were older (mean age 56.31 + 17.19 versus 53.33 + 15.23 years;
p=0.001) as also, had lower levels of schooling (
p=0.011), lived alone or without a partner (
p<0.001) and had a higher frequency of diabetes (
p=0.009). There were no significant differences in terms of ethnicity, other comorbidities, need for ICU admission, use of vasoactive drugs, hemodialysis and/or mechanical ventilation (Table 2).
When assessed for LPCS, patients with LPCS were younger (
p=0.024) and males (
p<0.001). There were no significant differences in terms of ethnicity, education, comorbidities, need for ICU admission, use of vasoactive drugs, hemodialysis and/or mechanical ventilation (Table 2). However, at the end of three, six and 12 months of follow-up, women were more frequently reported having LPCS (59% versus 45%;
p<0.001), (51.7% versus 40%;
p<0.001), and (72.9% versus 59.5%;
p<0.001), respectively. Furthermore, there was an increase in the frequency of long post-COVID syndrome over time for both genders, reaching its peak frequency at 12 months of follow-up, primarily affecting female patients (Figure 1).
Regarding the evaluation of quality of life by the EQ-5D-3L questionnaire, there was a trend towards worsening in the quality of life over time, predominantly among women in all domains: in the mobility domain at three months (9% versus 5.7%,
p=ns), at six months (17 versus 6.8%,
p<0.05) and at 12 months (28.4% versus 9.3%,
p<0.05), in the personal care domain at three months (7.7% versus 4.1%,
p<0.05), at six months (15.6 versus 5.8 %,
p<0.05) and at 12 months (14.8% versus 5.6%,
p<0.05), in the usual activities domain at three months (12% versus 6.2%,
p<0.05), at six months (19.1 versus 8.9%,
p<0.05) and at 12 months (30.8% versus 13.1%,
p<0.05), pain/discomfort domain at three months (20.1% versus 10.3%,
p<0.05), at six months (28.4 versus 11.6%,
p<0.05) and at 12 months (29% versus 16.9%,
p<0.05) and the anxiety/depression domain at three months (34.1% versus 30.8%,
p=ns), at six months (38.8 versus 29.1%,
p=ns) and at 12 months (43.8% versus 33.3%,
p<0.05). Finally, there was a trend towards lower scores on the visual analogue scale (VAS), whose scores range from zero (worst) to 100 points (best), over time for women compared to men, at three months (85 versus 87,
p<0.05), at six months (81 versus 85,
p<0.05) and at 12 months (79 versus 81,
p=ns) (Figure 2).
DiscussionIn this longitudinal cohort, which assessed surviving post-COVID patients by telephone interview at 3, 6 and 12 months after hospital discharge, found that half of the patients met the criteria for LPCS initially and was worsening over time, although it was more frequent in the female population, which was perceived in up to 73% at the end of 12 months. Also, women had more chance and probable to have impairment in quality of life over time, assessed by the EQ-5D-3L questionnaire, for all domains, especially at the end of 12 months. This makes women as a priority group for assessment, monitoring and treatment in mental health and physical rehabilitation programs after developing acute COVID-19.
Women have been more frequently affected by LPCS.
9,10 Women have been often diagnosed with autoimmune diseases, measured higher immunoglobulins levels, and responded better to infections and vaccines compared to men.
11 Females are affected two to three-fold higher than males with LPCS.
12 Males have been reported to develop severe cases of acute COVID-19,
13 but not LPCS. A metanalyses showed that global prevalence of inpatients had more frequent long COVID than outpatients (54% versus 34%) and it was confirmed that female adults had both higher prevalence and risk of having post-COVID-19 than male adults.
14 And, the survival rate was lower in men than in women.
15 In our study there were no significant differences in terms of ethnicity, education, comorbidities, need for ICU admission, use of vasoactive drugs, hemodialysis and/or mechanical ventilation.
Vaccines against SARS-CoV2 has been a risk factor for preventing long COVID.
16 Analyzing among healthcare personnel, another Brazilian study identified that female sex, age and more than two infections by COVID-19 were factors related to develop long COVID. However, protective factors were infections caused by variants delta and omicron of SARS-CoV-2 and receive 4 doses of COVID vaccines prior to infection.
16 Then, vaccination programs against COVID should be stimulated for preventing LPCS not only to reduce morbidity and mortality by SARS-CoV-2 infections.
Patients with LPCS have reported less physical activities even after 6 months onset of symptoms.
17 Malik
7 reiterate the high prevalence of continuous symptoms affecting the population, reducing quality of life, with great social and financial impact, requiring rehabilitation programs. In our study, they found that women had higher risk to develop LPCS and worsening over time, an average of 61.8% of the women will reach to 73% at the end of the 12 months of the study.
Severity of acute COVID has been related to higher incidence of LPCS. Older patients have been related to longer post period of LPCS and severity of acute COVID was the main factor that determined the duration of symptoms in long cases.
18 Around 50% of the patients slowly returned to work after hospitalization by moderate-severe and critical cases of COVID-19.
19 Psychological dysfunctions often have been reported, such as depression, anxiety, post-traumatic stress, lethargy, and low mood affecting individual’s quality of life by making it difficult to perform normal activities.
20 Then, LPCS has been widely imprecise about quality and quantity of symptoms what quality of life questionnaire should be used to objectively evaluate patients after COVID-19 infection.
Women also have been greater impairment of quality of life after hospital discharge by COVID-19.
21 Anxiety/depression dimension has been the most affected mainly in advanced age of the people and women.
22,23 Anxiety/depression domain has been secondary not only to persistent symptoms but women are often taking care of the family and housework, as well as losing a job or income in the economic crisis’.
23 Moreover, COVID survivors have been more related with psychiatric morbidity and/or neurocognitive impairment.
24Our study, women were more compromised in the EQ-5D-3L questionnaire, mainly in the anxiety/depression and usual activities domains, besides worsening in self-assessment. Thus, we can infer that survivors after COVID-19 should be substantially evaluated to the possibility of LPCS and/or quality of life, since these patients have been progressively worsening over time, especially among women, which has been proven to be a priority group.
The frequency of LPCS and quality of life impairment have ranged a lot over time. The LPCS has been reported widely unspecific about numbers and kinds of symptoms,
25 which makes data from studies so vulnerable to biases on the diagnoses.
26 Up to 84 different symptoms have been related to LPCS. Moreover, some studies have identified that the frequency of LPCS has decreased over time. Post COVID-19 patients also need to be evaluated for quality of life questionnaire, which could give greater information about the impact of the disease and provide knowledge about treatmentor rehabilitation.
27 Actual, new health services had not been created to offer properly care for COVID survivors, especially for women, as well as sex-specific rehabilitation programs should be adapted to improve psychological status and quality of life,
28 which may explain the worsening of these situations over time.
In Brazil, World Health Organization (WHO) estimates between 2.8 million and 5.6 million people will need health care due to long COVID, around 10% to 20% are of confirmed cases.
29 However, there was no effort by the Ministry of Health to collect data on the numbers and profile of people affected by LPCS, they failed to recognize the problem and understand it in terms of its impact in the Brazilian health system , specific rehabilitation protocols for LPCS have not been developed for different priority groups, factors that make it hard to design strategies to meet this demand.
30 In this way, it is important to specifically screen and understand post-COVID-19 patients, in search of rehabilitation protocols, by a multidisciplinary team, that individualize the demands of the population.
There were some limitations in this study. First, the loss of follow-up of patients over time with about 30% at the end of 12 months of the initial group. Second, the data were collected from patients from a single hospital. And finally, patients were not assessed for health status before COVID. However, this prospective cohort assessed clinical and epidemiological data of surviving patients after hospitalization for COVID, for LPCS and quality of life at the end of 3, 6 and 12 months, by telephone interview, a recognized monitoring modality, of a reference hospital whose results are expressive and worrisome as to the degree of clinical, physical, mental, and consequently social involvement, especially among women.
Thus, this study showed that the development of LPCS and/or the impaired quality of life affects a significant portion of survivors after post-COVID hospitalization, it worsens over time, and women were a risk group. Our study also helped to identify patients and clinics in having greater impact on their health conditions, and the importance for comprehending and managing LPCS. LPCS is not symptom-specific and likely requires a long time for physical, mental, and social rehabilitation. Therefore, rehabilitation programs and public policies need to be available and targeted to post-COVID patients in a comprehensive and accessible way, especially for priority groups such as women.
References1. World Health Organization 2023. WHO Coronavirus (COVID-19) Dashboard. WHO-Coronavirus (COVID-19) Dashboard. 2023. [access in 2024 Mar 31]. Available from:
https://data.who.int/dashboards/covid19/cases2. Joan B Soriano, Srinivas Murthy, John C Marshall, Pryanka Relan JVD. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022; 22: e102-07.
3. Lixue Huang, Qun Yao, Xiaoying Gu, Qiongya Wang, Lili Ren, Yeming Wang, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021 Aug; 398 (10302): 747-58.
4. Harenwall S, Heywood-Everett S, Henderson R, Godsell S, Jordan S, Moore A, et al. Post-Covid-19 Syndrome: Improvements in Health-Related Quality of Life Following Psychology-Led Interdisciplinary Virtual Rehabilitation. J Prim Care Comm Health. 2021; 12.
5. Malheiro DT, Bernardez-Pereira S, Parreira KCJ, Pagliuso JGD, Paula Gomes E, Mesquita Escobosa D, et al. Prevalence, predictors, and patient-reported outcomes of long COVID in hospitalized and non-hospitalized patients from the city of São Paulo, Brazil. Front Public Health. 2023; 11: 1302669.
6. Oliveira JF, Ávila RE, Oliveira NR, Cunha Severino Sampaio N, Botelho M, Gonçalves FA, et al. Persistent symptoms, quality of life, and risk factors in long COVID: a cross-sectional study of hospitalized patients in Brazil. Int J Infect Dis. 2022 Sep; 122: 1044-51.
7. Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL) - A systematic review and meta-analysis. J Med Virol. 2022 Jan; 94 (1): 253-62.
8. Santos M, Cintra MAG, Monteiro AL, Santos B, Gusmão-Filho F, Andrade MV, et al. Brazilian Valuation of EQ-5D-3L Health States: Results from a Saturation Study. Med Decis Making. 2016. 36 (2): 253-63.
9. Vos T, Hanson SW, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, et al. Estimated Global Proportions of Individuals with Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA. 2022; 328 (16): 1604–15.
10. Fumagalli C, Zocchi C, Tassetti L, Vittoria M, Amato C, Livi L, et al. Factors associated with persistence of symptoms 1 year after COVID-19 : A longitudinal, prospective phone-based interview follow-up cohort study. Eur J Intern Med. 2022; 97: 36–41.
11. Frontera JA, Sabadia S, Yang D, Havenon A De, Yaghi S. Life stressors significantly impact long-term outcomes and post-acute symptoms 12-months after COVID-19 hospitalization. J Neurol Sci. 2022; 443: 120487.
12. Bai F, Tomasoni D, Falcinella C, Barbanotti D, Augello M, Mondatore D, et al. Female sex is associated with long COVID syndrome : a prospective cohort study. Ottavia Vigan o. Clin Microbiol Infect. 2022; 28 (4): 611.e9-611.e16.
13. Pradhan A. Sex differences in severity and mortality from COVID-19 : are males more vulnerable ? 2020;7: 1–11.
14. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J Infect Dis. 2022 Nov; 226 (9): 1593-1607.
15. Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. May Clin Proc. 2020; 95 (8): 1613-20.
16. Marra AR, Sampaio VS, Ozahata MC, Lopes R, Brito AF, Bragatte M, et al. Risk factors for long coronavirus disease 2019 (long COVID) among healthcare personnel, Brazil, 2020–2022. Infect Control Hosp Epidemiol. 2023; 44 (12): 1972-8.
17. Delbressine JM, Machado FVC, Goërtz YMJ, Van Herck M, Meys R, Houben-Wilke S, et al. The impact of post-covid-19 syndrome on self-reported physical activity. Int J Environ Res Public Health. 2021; 18 (11): 1–11.
18. Miranda DAP, Gomes SVC, Filgueiras PS, Corsini CA, Almeida NBF, Silva RA, et al. Long COVID-19 syndrome: a 14-months longitudinal study during the two first epidemic peaks in Southeast Brazil. Trans Royal Soc Trop Med Hyg. 2022; 116 (11): 1007-14.
19. Azevedo HMJ, Santos NWF, Lafetá ML, Albuquerque ALP, Tanni SE, Sperandio PA, et al. Persistence of symptoms and return to work after hospitalization for COVID-19. J Bras Pneumol. 2022; 48 (6): e20220194.
20. Oliveira RCS, Amaral LMB, Silva ABD, Brandão AS, Teixeira FTB, Maia LC, et al. Síndrome pós-Covid-19: breve revisão sistemática. Braz J Health Rev. 2022; 5 (2): 5714-29.
21. Costa B, Szlejf C, Duim E, Linhares AOM, Kogiso D, Varela G, et al. Clinical outcomes and quality of life of COVID-19 survivors: A follow-up of 3 months post hospital discharge. Respir Med. 2021; 184: 1–8.
22. Mitrović-Ajtić O, Stanisavljević D, Miljatović S, Dragojević T, Živković E, Šabanović M, et al. Quality of Life in Post-COVID-19 Patients after Hospitalization. Healthcare (Basel). 2022; 10 (9): 1666.
23. Ma Y, Deng J, Liu Q, Du M, Liu M, Liu J. Long-Term Consequences of COVID-19 at 6 Months and Above: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022; 19 (11): 6865.
24. Méndez R, Balanzá-Martínez V, Luperdi SC, Estrada I, Latorre A, González-Jiménez P, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. 2021; 290 (3): 621-31.
25. Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID : a living systematic review. BMJ Glob Health. 2021; 6 (9): e005427.
26. Alkodaymi MS, Omrani OA, Fawzy NA, Shaar BA, Almamlouk R, Riaz M, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022; 28: 657-66.
27. Amdal CD, Pe M, Sørum R, Claire F, Andrew P, Ignacio J, et al. Health - related quality of life issues, including symptoms, in patients with active COVID-19 or post COVID-19: a systematic literature review. Qual Life Res. 2021; 30 (12): 3367-81.
28. Hu J, Zhang Y, Xue Q, Song Y, Li F, Lei R, et al. Early Mental Health and Quality of Life in Discharged Patients With. Front Public Heal. 2021; 9:1–8.
29. Stam G. Covid longa pode deixar sequelas que duram muitos meses. Pesq FAPESP. 2022; 16 Mar. [Internet] [access in 2022 Dez 19]. Available from:
https:// revistapesquisa.fapesp.br/covid-longa-pode-deixar-sequelas-que-duram-muitos-meses/30. Batista KBC, Fernandez MV, Barberia LG, Silva ET, Pedi VD, Pontes BMLM, et al. Panorama da COVID longa no Brasil: análise preliminar de um inquérito para pensar políticas de saúde. Cad Saúde Pública. 2024; 40 (4): e00094623.
Authors’ contributionCosta MLC: study design and methodology, research, project management, data collection, analysis and interpretation, writing and revision of the manuscript. Franco MR, Costa CM, Andrade LB: support in methodology and data collection and analysis. Costa MM, Costa GCS, Queiroz Neta ML: support in methodology, research, data collection, analysis and interpretation. Costa GJ: study design, methodology, data analysis and interpretation, revision of the manuscript. All the authors have approved the final version of the article and declare no conflicts of interest.
Received on October 10, 2023
Final version presented on July 19, 2024
Approved on August 21, 2024
Associated Editor: Melânia Amorim
 ; Marcela Rezende Franco 2
; Marcela Rezende Franco 2 ; Mariana Menezes Costa 3
; Mariana Menezes Costa 3 ; Camila Menezes Costa 4
; Camila Menezes Costa 4 ; Gabriela Carla dos Santos Costa 5
; Gabriela Carla dos Santos Costa 5 ; Maria Luiza de Queiroz Neta 6
; Maria Luiza de Queiroz Neta 6 ; Lívia Barboza de Andrade 7
; Lívia Barboza de Andrade 7 ; Guilherme Jorge Costa 8
; Guilherme Jorge Costa 8