ABSTRACT
OBJECTIVES: to evaluate the second stage of the Kangaroo Mother Care (KMC) and its integration with the third stage in maternity hospitals in Recife in the context of the coronavirus pandemic.
METHODS: normative assessment carried out at the Kangaroo Neonatal Intermediate Care Unit (KNICU) in two public reference maternity hospitals for KMC between November/2021 and May/2022. The logical model and matrix of KMC indicators were developed and validated using the Delphi Method: semi-structured interviews were carried out with professionals from the KNICU team and the municipal child health coordination. It was considered implemented when the criteria were met (from 100.0 to 80.0%); partially implemented (79.9 to 60.0%); incipient (59.9 to 40.0%) and not implemented (<or=39.9%).
RESULTS: the MC was partially implemented in both KNICU (79.0% both). The Structure dimension was implemented (84.0 and 97.0%) and the Process dimension, in the Education (70.0% both) and Management components, were partially implemented (61.0% and 78.0%), although the units claim that they do not share clinical objectives, exams and treatments and do not have an effective referral/counter-referral system. While Assistance was implemented in one unit (90.0%) and partially implemented in the other (75.0%).
CONCLUSION: KNICU was partially implemented during the coronavirus pandemic in the two reference maternity hospitals, but with obstacles to integration with the third stage of the method.
Keywords:
Premature birth, Kangaroo-mother care method, COVID-19, Health evaluation, Process assessment, Health care
RESUMO
OBJETIVOS: avaliar a segunda etapa do Método Canguru (MC) e a sua integração com a terceira etapa em maternidades do Recife no contexto da pandemia de coronavírus.
MÉTODOS: avaliação normativa realizada na Unidade de Cuidados Intermediários Neonatais Canguru (UCINCa) em duas maternidades públicas de referência para o MC entre novembro/2021 e maio/2022. Elaborou-se o modelo lógico e a matriz de indicadores do MC, validada através do Método Delphi. Realizaram-se entrevistas semiestruturadas com profissionais da equipe das UCINCa e a coordenação municipal de saúde da criança. Considerou-se implantado quando os critérios alcançaram (de 100,0 a 80,0%); parcialmente implantado (79,9 a 60,0%); incipiente (59,9 a 40,0%) e não implantado (<ou=39,9%).
RESULTADOS: o MC estava parcialmente implantado nas duas UCINCa (79,0% ambas). A dimensão Estrutura encontrava-se implantada (84,0 e 97,0%) e a de Processo, nos componentes Educação (70,0% ambas) e Gestão encontravam-se parcialmente implantados (61,0% e 78,0%), embora as unidades afirmem não compartilhar os objetivos clínicos, exames e tratamentos e não ter um sistema de referência/contrarreferência efetivo. Ao passo que o componente Assistencial estava implantado em uma unidade (90,0%) e parcialmente implantado na outra (75,0%).
CONCLUSÃO: a UCINCa encontrava-se parcialmente implantada durante a pandemia de coronavírus nas duas maternidades de referências, mas com obstáculos para a integração com a terceira etapa do método.
Palavras-chave:
Nascimento prematuro, Método canguru, Covid-19, Avaliação em saúde, Avaliação de processos em cuidados de saúde
IntroductionPrematurity is a challenge for perinatal care. According to estimates, one out of ten babies is born prematurely worldwide, and in 2020, approximately one million babies died due to it, as it is considered the main cause of death for children under five years of age.
1 Furthermore, millions of children remain with sequelae and disabilities, besides the technological development, as well as the development observed in perinatal care, which increased the survival rate of preterm low weight neonates. Thus, the need for providing postnatal care focused in a better development for preterm newborns (PTNB) is evident, in order to fully perform all their capabilities.
1,2Kangaroo Method (KM) is a strategy for decreasing infant mortality and for qualification of neonatal care, as it is recognized for the early skin-to-skin contact provided by the “Kangaroo Care”, which assumes diverse characteristics in the countries that adopt it.
3-5 In Brazil, it consists in three stages, the first two at the hospital: one in the Neonatal Intensive Care Unit (NICU) and other in the Conventional Neonatal Intermediate Care Unit (CNICU), and the other in the Kangaroo Neonatal Intermediate Care Unit (KNICU). The third one occurs after hospital discharge, by means of the sharing of the care between the maternity of origin and the Basic Health Unit (UBS – Portuguese acronym) for following-up the child until he/she reaches 2500g.
3,4,6Preterm or low birth weight children need specialized treatment during hospitalization and hospital discharge, as well as support and monitoring of the primary healthcare team (APS – Portuguese acronym). At the KNICU, besides the reception and qualified assistance for both the PTNBs and their families, guidelines and encouragement for maintaining the shared follow-up of children, which is shared by the outpatient clinic and the APS.
7In the face of a public health emergency of international interest, the international sanitary regulation recommends that national health systems be structured to respond to the resulting needs. Similarly, in face of Covid-19 pandemic, enacted in March 2020, health services adopted several strategies for its challenging.
8Among them, restrictive measures that implied in the need for adaptations for the assistance provided to the mother-child binomial.
9Initially, contradictory global guidelines were published, which caused negative impacts for KM continuity,
10-13 yet it was posteriorly identified that the benefit of maintaining the method is 65 to 630 times higher than the risk of dying from Covid-19.
11 Despite of this, a study about the KM carried out in 62 countries observed substantial changes in the services related to PTNB.
12Assessing the repercussions of the coronavirus pandemic in the PTNB and low weight neonates is essential to continue the integrative assistance for this group. Studies on diversified interventions signalize the fact that the assessment and monitoring are tools that favor choices of effective and essential actions for their full implementation when pointing barriers that restrict the achievement of better results.
14,15 This study aimed to assess the second stage of KM and its integration with the third stage in maternity hospitals in Recife in the coronavirus pandemic context.
MethodsNormative assessment of KNICU, in which the resources employed, their organization, the services and goods produced were compared with the criteria and regulations established by the Ministry of Health (MH).
16The survey was carried out in the KNICU of two public maternity hospitals located in the municipality of Recife. The maternity A is a philanthropic entity, focused in high-risk and is one of the National Reference Centers for KM. At first, the Neonatal Unit (NU) had 18 NICU beds, 32 CNICU beds and 22 KNICU beds.
17 However, during Covid-19 pandemic, the institution became the maternity of reference in the state for assistance to pregnant women with SARS-Cov-2, implying in the temporary interruption of the KNICU, which reopened in the end of 2021, with five beds that increased progressively until ten beds in the period of data collection.
The maternity B is a unit for high-risk births as well, acts as a reference in the state for KM and has 15 NICU beds, 15 CNICU beds and eight KNICU beds, with two extra beds.
18 During Covid-19 pandemic the KNICU had no interruption of medical care, although the sanitary restrictions reduced the number of hospitalizations.
For the execution of the assessment, we elaborated a logic model of the second stage of KM (Table 1). The modeling of intervention considered the donabedian triad structure, process and result, in which structure refers to physical, human and material resources needed for providing care; the process refers to activities developed by health professionals; and result, to the effects obtained in healthcare.
19 For the building of the logical model, institutional documents and technical standards concerning KM were consulted. Among them: Ordinance SAS/MS n° 930/2012, Ordinance GM/MS nº 1683/2007 and the KM handbooks: Kangaroo method: care guidelines (2019), Handbook of the third stage of Kangaroo Method in Basic Care (2018), Humanized care for the newborn: Kangaroo Method: technical handbook (2017), Guidelines for Kangaroo Method in Basic Care: Shared Care (2016) and Shared Follow-up between Hospital Care and Basic Care (2015). Local strategies for the application of KM policy, such as Plans and state and municipal laws were not included, since they are not generalized for the entire country.
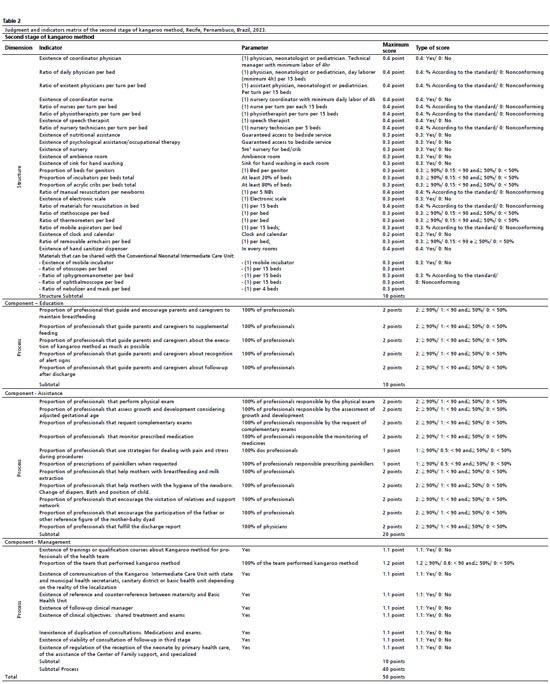
Lastly, the logical model presented three components: 1) Education, relating the guidelines to parents and caregivers, 2) Assistance, referring to care for the PTNB, specifically, and 3) Management, which is related to the integration between the second and third stages of the method and qualification of the multidisciplinary team. From the logical model, ajudgment matrix and indicators were created, representing the structure and process for each component of the model and defined as parameters according to the Ordinances and Handbooks consulted, and when not available, it was established by the main researcher by means of previous experience in a teaching hospital.
Aiming to expand the validity of the construct and the reliability, the judgment matrix and indicators were submitted to review by a group of specialists in the area of the survey, using a technique for achieving consensus, the Delphi Method. Details about the methodological procedures used in the technique were previously described and published.
20The final judgment and indicatorsmatrix was composed of 51 indicators, distributed into 26 structure indicators and 25 process indicators (Table 2).
The period of data collection occurred between November 2021 and May 2022, using a tool for collection based on indicators of the judgment matrix and organized considering the components of the KNICU. Professionals of higher education from the multidisciplinary team that act on the KNICUs were included in the survey, as well as the KM coordinators of these services and the manager of the health department of the municipality, and professionals who were on vacation or medical leave during data collection. The semi-structured interviews were carried out with nine professionals of maternity A, a medical coordinator, a nursery coordinator, two assistance nurses, two physicians, a speech therapist, a physiotherapist and two psychologists. In maternity B, nine professionals were interviewed: a medical coordinator, a nursery coordinator, three assistance nurses, a physician, a speech therapist, an occupational therapist and a psychologist.
In order to evaluate how many criteria and standards of KM were achieved, the level of implementation was expressed by the proportion of the score obtained in relation to the maximum score for each component and for the service as a whole, related to structure and process, according to the judgment and indicators matrix. In order to classify the level achieved by the KNICU, the following cutoff points were adopted: implemented, when achieving percentages from 100.0% to 80.0%, partially implemented, between 79.9% and 60.0%, incipient, between 59.9% and 40.0% and non-implemented, lower or equal to 39.9%.
The guidelines from 466/12 resolution of the National Health Council were followed and the study was approved by the IMIP Research Ethics Committee CAAE n° 35017420.7.3002.5201 and by the HAM Research Ethics Committee, CAAE nº 35017420.7.3001.5197.
ResultsIn both services, the KNICU was considered partially implemented (79.0%) during Covid-19 pandemic. The Structure dimension was implemented in Maternity B (84.0%) and Maternity A (97.0%). In the Process dimension, the component Education was partially implemented and both services obtained the same proportion (70.0%). The component Assistance was implemented in maternity B (90.0%) and partially implemented in maternity A (75.0%); whilst the Management component was partially implemented in maternity B (61.0%) and maternity A (78.0%) (Table 3).
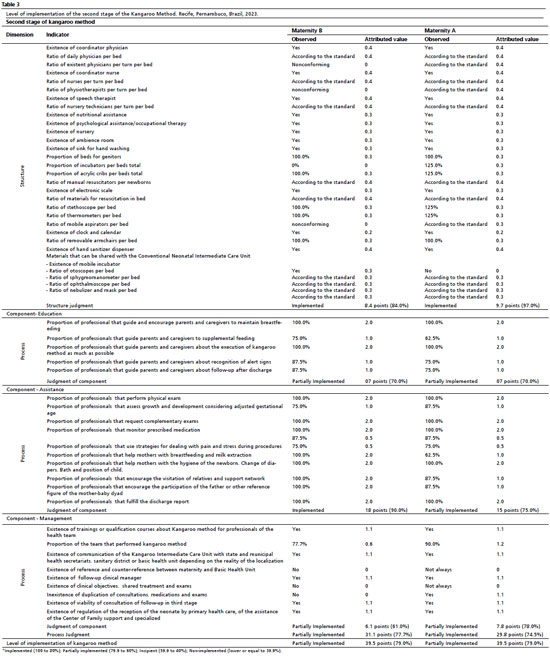
With regard to the structure of the KNICUs, maternity B did not have a physiotherapist, nor incubators or portable aspirators, whilst maternity A did not have a mobile incubator in the department. In the Education component, the indicators with lower scores in maternities B and A were: “Proportion of professionals who guide parents and caregivers about artificial feeding” (75.0% and 62.5%, respectively); “Proportion of professionals who guide parents and caregivers about the recognition of alert signs” and “Proportion of professionals who guide parents and caregivers about follow-up after hospital discharge” (both with 87.5% and 75.0%, respectively) (Table 3).
With regard to the Assistance component, in maternity B, 100.0% of professionals reported to stimulate the participation of fathers or other reference figure for the mother-baby dyad, and the visitation of relatives and social support networks, whilst 87.5% of professionals of maternity A reported the same; 100.0% of professionals of maternity B reported to help mothers in breastfeeding and extraction of milk, against 62.5% of professionals of maternity A. In relation to the Management component, qualifications on the method occurred in both services, with 77.0% of professionals of maternity B reporting to have accomplished courses, whilst in maternity A it was 90.0%. Similarly, professionals of both units reported to have a clinical manager and communication of the KNICU with the state and municipal health secretariats, sanitary district or UBS (Basic Health Units). Nevertheless, professionals of maternity B affirmed that there is no sharing of clinical goals, exams and treatments nor the effective existence of a reference and counter-reference system with the UBS, whilst those from maternity A informed that these actionsdo not always occur (Table3).
DiscussionThe study demonstrated that during the coronavirus pandemic, the second stage of KM was partially implemented in both reference services and presented impairments to the integration with the third stage of the method. On the other hand, whilst the structure dimension was implemented, there were variations in the level of implementation within the components of the process dimension, with the components Education and Management partially implemented and the component Assistance implemented and partially implemented, respectively, for each health unit.
During the pandemic, the maternity A KNICU, one of the National Reference Centers (CNR – Portuguese acronym), was temporarily closed while acting as a state reference for pregnant women with coronavirus, and their professionals were relocated in other departments of the institution. The reopening of the KNICU was gradual, which may explain its partial implementation. A study carried out in 2015 identified that all maternities indicated as CNR of the method and 66.7% of those of state reference presented all their stages implemented.
21 The difference of these results with those of our assessment, besides the pandemic onset and the hiatus of almost ten years between the surveys
21 may occur due to the fact of the indicators matrix has normative updates, which did not exist previously, or having used different criteria of judgment.
The interruption of KNICU in maternity A was also found in several countries that adopted the centralized response strategy for isolation and treatment of Covid-19.
12 Such strategy altered the care provided to newborns (NB) that included relocation in the space of the unit, the redistribution of the neonatal care team for tasks related to Covid-19, and even the mother-baby separation not only for mothers who tested positive for Covid-19, but also the suspect ones, interrupting the continuity of care provided to mothers and NBs.
11,12 In Brazil, the MH guideline was to not reduce or close the KNICUs,
22 although several maternities were affected in the country.
Rao
et al.
12 identified that KM was the routine practice of 85% of interviewees previously to the pandemic, and during the pandemic, 55%. The repercussions of coronavirus pandemic on KM included the reduction of skin-to-skin contact (26.5%), earlier discharge (30.8%), total interruption of KM services (7%) or restrict policies of visitation (51.2%).
23In the present study, professionals of both services reported having stimulated visitation of relatives of the support network. In spite of that, during pandemic, with the social distancing measures, there were restrictions in the policy of visitation and the involvement of family with care for the NB, besides the other consequences verified for KM.
9,11,12,22-24 Such measures included impairments in maternal mental health, hindering the bond with the NB and the adhesion to KM.
24 With the proper support of the KNICU team, such damages can be mitigated, favoring a positive effect in the interaction and care of the NB.
9.24,25 However, aspects related to uncertainties, guidelines and availability of personal protection equipment brought fear for life, stress and worry within the NB caregivers.
12The structure dimension was implemented in the two assessed services, and this is one of the relevant aspects in the strategy of humanization of care. Accordingly, professionals and patients interviewed about the environmental desirable attributes in a KNICU highlighted the importance of the comfortable environment, with privacy, controlled access, with furniture and ergonomic equipment in sufficient quantity.
26In this study, the proportion of professionals that guide parents and caregivers about recognition of alert signs was suboptimal, with lower values in maternity A than in maternity B. This inadequate orientation to parents may be associated with other factors related to the institution or the professionals.
27-29 Also, some professionals recognize certain activities as attribution of other members of the team. Besides, a survey demonstrated that some professionals tend to prioritize the immediate assistance, disregarding educational activities and the preparation for hospital discharge.
27Similar to the finding about alert signs, the proportion of professionals that guide parents and caregivers about the follow-up after discharge had a low adhesion. Differently, the MH recommends and studies bring the relevance of the preparation for discharge by means of adequate guidance to families concerning the continuity of assistance in the third stage of KM and the link between mothers and primary healthcare teams.
27,28 A survey carried out in a mother-and-child teaching hospital identified that although nurses are aware of the KM benefits, low knowledge about KM is predominant, with scarce experience, resistance from the team and insufficient institutional support for its implementation.
27 Thus, the problems that may occur in households are not sufficiently valued and predicted, and the solutions, not properly informed.
29In the component Management, some weaknesses were identified in both services during the pandemic that were partially implemented. The absence of sharing of clinical objectives, exams and treatments for KNICU, previous outpatient clinic and Basic Health Unit are barriers for an effective network of reference and counter-reference, impairing the integration between second and third stages of KM.
28 Studies indicate a fragile communication between the different levels of care, fragmenting and discontinuing care, where primary healthcare professionals minimize their importance in the third stage of KM, and sometimes, the clinical communication with the specialized service is assumed by the NB caregivers.
3,5 This weakness may reverberate in the increase of late neonatal mortality, mainly in the pandemic context, in which the government guideline was the temporary interruption of follow-up consultations in outpatient clinics and their execution by primary healthcare teams.
3,22These difficulties are exposed in a survey that identified a significant number of mothers that did not receive visitations at home in the first week of hospital discharge and related this to a probable lack of adequate orientation on the importance of shared care with APS, by KNICU professionals. It also demonstrated that these professionals, even recognizing the importance of primary healthcare, believed to be unprepared to deal with PTNB or low birth-weight newborns and needed to be qualified.
3With regard to the qualification of professionals that act on KM, an expressive number of interviewed professionals referred having qualification on the method, however with distinct percentages in the institutions, higher in maternity A. Qualifications and updates for the team about KM are essential for ensuring quality of assistance in all its stages for patients and their families, promoting emotional support for the team to feel confident about their conduct.
12,25,30As limitations of this study, in spite of the normative assessment effectiveness when criteria and ministry standards are achieved, it does not clarify the reason of non-implementation, yet it draws hypotheses in a pandemic context. Furthermore, the pandemic period itself interfered with the result of assessment, since the challenges imposed to professionals and services generated specific impairments for the implementation of KM.
The KNICU was partially implemented during the coronavirus pandemic in both reference maternities, with barriers for the integration with the third stage of the method for its full implementation. Whilst the Structure dimension was implemented in both units, the Process dimension was partially implemented in all its components, with exception of the Assistance component in maternity B. We highlight the need for qualifying professionals for KM, as well as making them aware of the execution of educational activities. The broadly recognized benefits of the method signalize the need for valuing its continuity, even with adaptations in a context of public health emergencies of international interest such as coronavirus pandemic. We reinforce the importance of promoting strategies that integrate the second and third stages, mainly with primary health care teams, for a qualified and integrative assistance for children after hospital discharge.
References1. World Health Organization (WHO). Born too soon: decade of action on preterm birth. Geneva: WHO; 2023. Licence: CC BY-NC-SA 3.0 IGO. [access in 2023 Out 5]. Available from:
https://creativecommons.org/licenses/ by-nc-sa/3.0/igo/2. Alves FN, Wolkers PCB, Araujo LB, Ferreira DMLM, Azevedo VMGO. Impacto da segunda e terceira etapas do método canguru: do nascimento ao sexto mês. Rev Enferm Centro Oeste Mineiro. 2021; 11: e4200.
3. Silva MV, Lamy ZC, Sousa AF, Hartz Z, Mendes CM, Ramos CV. Evaluation of the third stage of the kangaroo method in primary health care. Rev Pesq. (Univ. Fed. Estado Rio J.). 2022; 14: e11116.
4. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Atenção humanizada ao recém-nascido: Método Canguru: diretrizes de cuidado. 1
st ed. Revisada. Brasília (DF): Ministério da Saúde; 2019. [access in 2023 Out 5]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/metodo_canguru_diretrizes_cuidado_revisada.pdf5. Aires LCP, Santos EKA, Bruggemann OM, Backes MTS, Costa R. Referência e contrarreferência do bebê egresso da unidade neonatal no sistema de saúde: percepção de profissionais de saúde da Atenção Primária. Esc Anna Nery 2017; 21 (2): e20170028.
6. Souza NA, Lamy ZC, Goudard MJ, Marba ST, Costa R, Caldas LN, et al. Factors associated with skin-to-skin contact less than 180 min/day in newborns weighing up to 1,800g: multicenter study. Ciênc Saúde Colet. 2023; 28 (4): 1021-9.
7. Lamy ZC, Soares M, Morsh DS. Cuidado compartilhado entre a Atenção Hospitalar e a Atenção Básica. In: Sanches MTC, Costa R, Azevedo VMGO, Morsh DS, Lamy ZC (org). Método Canguru no Brasil: 15 anos de política pública. São Paulo: Instituto de Saúde, 2015. Cap. 11. [access in 2023 Out 5]. Available from:
https://portaldeboaspraticas.iff.fiocruz.br/wp-content/uploads/2017/10/canguru_capa_miolo.pdf8. Organização Pan-americana da Saúde (OPAS). Histórico da pandemia de Covid-19. [Internet] [access in 2023 Out 5]. Available from:
https://www.paho.org/pt/covid19/historico-da-pandemia-covid-19.
9. Custodio ZAO, Morsch DS, Marba STM, Gomes MAM, Machado, LG, Lamy ZC. Kangaroo Care: how to guarantee and expand in Covid-19 times. 2020. SciELO Preprints [Preprints]. [access in 2023 Out 5]. Available from:
https://doi.org/10.1590/SciELOPreprints.77310. Coşkun Şimşek D, Günay U, Özarslan S. The impact of the COVID-19 pandemic on nursing care and nurses’ work in a neonatal intensive care unit. J Pediatr Nurs. 2022; 66: 44-8.
11. Minckas N, Medvedev MM, Adejuvigbe EA, Brotherton H, Chellani H, Estifanos AS, et al. Preterm care during the COVID-19 pandemic: A comparative risk analysis of neonatal deaths averted by kangaroo mother care versus mortality due to SARS-CoV-2 infection. EClinicalMedicine. 2021; 33: 100733.
12. Rao SPN, Minckas N, Medvedev MM, Gathara D, Prashantha YN, Estifanos AS, et al. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers’ voices and experiences. BMJ Glob Health. 2021; 6: e004347.
13. Yeo KT, Oei JL, De Luca D, Schmölzer GM, Guaran R, Palasanthiran P, et al. Review of guidelines and recommendations from 17 countries highlights the challenges that clinicians face caring for neonates born to mothers with COVID-19. Acta Paediatr. 2020; 109: 2192-207.
14. Bezerra TC, Falcão ML, Goes PS, Felisberto E. Evaluation of professional training programs in health: indicator construction and validation. Trab Educ Saúde. 2016; 14 (2): 445-72.
15. Bittencourt DAS, Vilela MEA, Marques COM, Santos AM, Silva CKRT, Domingues RMSM, et al. Labor and childbirth care in maternities participating in the “Rede Cegonha/Brazil”: an evaluation of the degree of implementation of the activities. Ciênc Saúde Colet. 2021; 26 (3): 801-21.
16. Brouselle A, Champagne F, Contandriopoulos AP, Hartz Z, orgs. Avaliação: conceitos e métodos. Rio de Janeiro: Editora Fiocruz; 2011.
17. Lima GMS. Trajetória do Método Canguru no Instituto de Medicina Integral Professor Fernando Figueira – IMIP. In: Sanches MTC, Costa R, Azevedo VMGO, Morsh DS, Lamy ZC, orgs. Método Canguru no Brasil: 15 anos de política pública. São Paulo: Instituto de Saúde; 2015. Cap. 04. [access in 2019 Jun 5]. Available from:
https://portaldeboaspraticas.iff.fiocruz.br/wp-content/uploads/2017/10/canguru_capa_miolo.pdf18. Secretaria Estadual de Saúde de Pernambuco (SES-PE). HAM apresenta novo espaço para Método Canguru, 2017. [access in 2019 Jun 5]. Available from:
http://portal.saude.pe.gov.br/noticias/secretaria-executiva-de-atencao-saude/ham-apresenta-novo-espaco-para-metodo-canguru19. Donabedian A. Quality assessment and assurance: unity of purpose, diversity of means. Inquiry. 1988; 25 (1): 173-92.
20. Cândido JLA, Frias PG, Sarinho SW. Construction and validation of indicators to evaluate the implementation of the Kangaroo Method using the Delphi technique. Rev Enferm UFPI. 2023; 12 (1): e4435.
21. Cardoso JS, Lamy ZC, Lamy F Filho, Gomes MA, Queiroz AL, Gianini NO, et al. Análise situacional da implantação do Método Canguru em maternidades públicas brasileiras. In: Sanches MT, Costa R, Azevedo VM, Morsch DS, Lamy ZC, orgs. Método Canguru no Brasil: 15 anos de política pública. São Paulo: Instituto de Saúde; 2015. p. 165-86.
22. Ministério da Saúde (BR). Secretaria de Atenção Primária à Saúde. Nota técnica nº 6/2020 - COCAM/CGCIVI/ DAPES/SAPS/MS. Atenção à Saúde do Recém-nascido no Contexto da Infecção do novo coronavírus (SARS-COV-2). [Internet]. Brasília (DF): Ministério da Saúde; 2020. [access in 2023 Out 11]. Available from:
http://docs.bvsalud.org/biblioref/2020/04/1087595/notatecnicaneonatal30mar2020covid-19.pdf23. Reichert APS, Guedes ATA, Soares AR, Brito PKH, Bezerra ICS, Silva LCL, et al. Repercussions of the Covid-19 pandemic in the care of premature infants. Esc Anna Nery 2022; 26 (spe): e20210179.
24. Morsch DS, Custódio ZAO, Lamy ZC. Psycho-emotional care in a neonatal unit during the Covid-19 pandemic. Rev Paul Pediatr. 2020; 38: e2020119.
25. Aires LCP, Koch C, Santos EKA, Costa R, Mendes JS, Medeiros GMS. Kangaroo-mother care method: a documentary study of theses and dissertations of the brazilian nurse (2000-2017). Rev Bras Enferm. 2020; 73 (2): e20180598.
26. Ely VHMB, Cavalcanti PB, Silveira JTT, Klein MF, Soares Junior A. Atributos ambientais desejáveis a uma unidade de alojamento conjunto Método Canguru a partir de uma experiência de projeto participativo. Ambient Constr. 2017; 17 (2): 119-34.
27. Ferreira DO, Silva MP, Galon T, Goulart BF, Amaral JB, Contim D. Kangaroo method: perceptions on knowledge, potencialities and barriers among nurses. Esc Anna Nery Rev. Enferm. 2019; 23 (4): e20190100.
28. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Manual da terceira etapa do Método Canguru na Atenção Básica. Brasília (DF): Ministério da Saúde; 2018. [access in 2023 Out 11]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/manual_terceira_etapa_metodo_canguru.pdf29. Sales IMM, Santos JDM, Rocha SS, Gouveia MTO, Carvalho NAR. Contributions of the nursing team in the second stage of the Kangaroo-Mother Care Method: Implications for hospital discharge of the newborn. Esc Anna Nery. 2018; 22 (4): e20180149.
30. Costa MC, Neves APSM, Cavalcanti MCAS, Morais ES. Proposta interprofissional de educação permanente em assistência perinatal no contexto da pandemia covid-19. Rev Multidiscip Saúde. 2023; 4 (3): 614-9.
Author’s contributionCândido JLA, Frias PG and Sarinho SW: conceptualization of the project, data analysis and interpretation, writing and critical review of the manuscript. All authors approve the final version of the manuscript and declare no conflicts of interest.
Received on March 13, 2023
Final version presented on July 11, 2024
Approved on July 25, 2024
Associated Editor: Ana Albuquerque
 ; Paulo Germano de Frias 2
; Paulo Germano de Frias 2 ; Silvia Wanick Sarinho 3
; Silvia Wanick Sarinho 3