ABSTRACT
OBJECTIVES: to describe the effects of the Covid-19 pandemic on maternal mortality in Brazil in 2021.
METHODS: it is an exploratory study with description of the excess maternal mortality in Brazil for 2021, considering different scenarios: (i) 2015-2019 linear trend; (ii) 2020 observed number of deaths; (iii) 2015-2019 linear trend corrected for general mortality excess; (iv) 2020 observed number of deaths corrected for general mortality excess.
RESULTS: compared to the trend of the previous five years, the year 2021 showed an excess mortality of 39% (n=3030). The maternal mortality ratio for 2021 drastically exceeded the SDG target for this indicator, reaching approximately 110 maternal deaths per 100,000 live births. In any scenario described, there will be excess maternal mortality in 2021 higher than general mortality and higher than level presented in 2020. Analysis stratified by region demonstrates subnational heterogeneity.
CONCLUSION: Covid-19 pandemic had a considerable impact on maternal health, not only by leading to increased deaths but also by increasing social health inequality. The year 2021 was the most critical period of the pandemic regarding the magnitude of mortality. Barriers to accessing and using essential health services are challenging to achieving health-related Sustainable Development Goals.
Keywords:
Maternal mortality, Covid-19, Excess mortality, Social determinants of health
RESUMO
OBJETIVOS: analisar os efeitos da pandemia da Covid-19 na mortalidade materna no Brasil em 2021.
MÉTODOS: realizou-se estudo exploratório com descrição do excesso de mortalidade materna no Brasil para 2021, considerando diferentes cenários: (i) tendência linear 2015-2019; (ii) número de óbitos observados em 2020; (iii) tendência linear 2015-2019 corrigida para excesso de mortalidade geral; (iv) número de óbitos observados em 2020 corrigido pelo excesso de mortalidade geral.
RESULTADOS: em comparação com a tendência dos cinco anos anteriores, o ano de 2021 apresentou excesso de mortalidade de 39% (n=3030). A razãode mortalidade materna para 2021 ultrapassou a meta dos ODS para este indicador, atingindo um nível superior a 110 mortes maternas por cem mil nascidos vivos. Em qualquer cenário, houve excesso de mortalidade materna em 2021 superior à mortalidade geral em 2020. A análise estratificada por região demonstra heterogeneidade subnacional.
CONCLUSÃO: a pandemia da Covid-19 teve impacto considerável na saúde materna, não só por levar ao aumento de mortes, mas também por aumentar a iniquidade em saúde. O ano de 2021 foi o período mais crítico da pandemia em termos de mortalidade. Barreiras ao acesso e uso de serviços de saúde são um desafio para alcançar os Objetivos de Desenvolvimento Sustentável relacionados à saúde.
Palavras-chave:
Mortalidade materna, Covid-19, Excesso de mortalidade, Determinantes sociais da saúde
IntroductionIn 2000, the United Nations (UN) established the reduction of maternal mortality as the ‘Millennium Goal' (MDG). After the end of the MDG cycle in 2015, it was found that the performance of the countries was not satisfactory, which led the institution to renegotiate it for the ‘Agenda 2030', which, in SDG 3.1 (Sustainable Development Goal) established an intent nor so ambitious: reducing it, globally, to less than 70/100,000 live births.
1Brazil failed to reach the goal proposed by the MDGs. Even so, in 2017, it established an even more ambitious goal, offering to reduce maternal mortality to 30/100,000 live births. Motta and Moreira
2 showed that, between 2001 and 2018, the national maternal mortality ratio (MMR) was never below 50.6/100,000 live births (2001), with a peak of 64.5/100,000 live births in 2009 At the end of the historical series, a. MMR magnitude was 56.2/100,000 live births. Furthermore, the context is one of social inequality: of the country's 450 health regions (CIR), about 70% had MMR greater than 30/100,000 live births, while 35.3% exceeded the target of 70/100,000 live births.
This is the national scenario before Covid-19. Thereafter, one of the most severe effects of the pandemic was aggravating the problems related to maternal mortality, both in its social determinations and in the performance of the Brazilian National Health System (SUS). One of main indicators of that was the excess of maternal mortality. Excess mortality is typically calculated by comparing the actual number of deaths observed during a specific period with the expected number of deaths under normal or baseline conditions. It is often used in public health and epidemiology to assess the impact of various factors on mortality, such as disease outbreaks, natural disasters, or other events. There is evidence concerning 2020.
3 The authors used data from the Mortality Information System (SIM) for general and maternal deaths and the Influenza Epidemiological Surveillance System (SIVEP-Influenza) to estimate female deaths and mothers by Covid-19. The excess maternal mortality in 2020 in Brazil was 1.40 (CI95%= 1.35-1.46), i.e., a mortality 40% higher than expected to that year.Even considering the excess mortality from COVID-19 for the female population of reproductive age, maternal mortality exceeded the expected number (MMR= 1.14; CI95%= 1.13-1.15).
3The diagnosis of maternal mortality in Brazil in 2020 was an essential baseline for better understanding the pandemic's effect on this critical indicator. Analysis of Covid-19 in Brazil also show that 2021 was much more challenging worldwide. Recently, the recent letter by Michels and Iser.
4 provided an essential update on the panorama of maternal mortality from Covid-19 in Brazil, initially launched by Souza and Amorim.
5 We offer additional comments here with calculations of excess maternal mortality in different scenarios of maternal mortality estimates in Brazil in 2021. The 2021 mortality data are currently consolidated, so the analysis is timely. In this context, this article aims to analyze the effects of the Covid-19 pandemic on maternal mortality in Brazil in the year 2021.
MethodsThrough an exploratory study, we described the excess of maternal mortality in Brazil for 2021, considering different scenarios. For this, we used data from the Mortality Information System for maternal deaths between 2015 and 2021. We used data from Influenza Epidemiological Surveillance Information System (SIVEP-Gripe) to assess maternal deaths from Covid-19 in the years 2020 and 2021. From these databases, we could count maternal deaths and deaths of childbearing age to estimate the excess maternal mortality in the country.
The definition of maternal death (inclusion criteria) includes every death of a pregnant woman or a new mother during pregnancy, childbirth, or in the postpartum period (typically within 42 days of giving birth), as a result of complications related to pregnancy or childbirth. As a control group, to verify the excess of maternal deaths compared to general mortality, we considered the mortality of women of childbearing age (15 to 49 years). Excess mortality was calculated considering the discrepancy between the observed and expected deaths for 2021.
Previously
3, we verified the excess maternal mortality in 2020 and compared it with the excess general mortality of women of childbearing age to confirm whether it differed from the excess general mortality. We repeat this analysis. However, considering that 2021 we can compare with scenarios in which the pandemic was already present, we calculated the number of expected maternal deaths for 2021 based on some counterfactual scenarios.
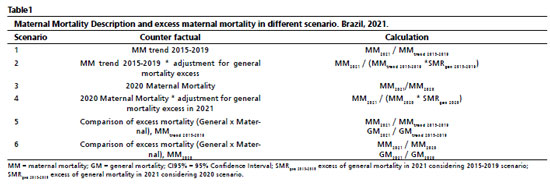
First, we checked excess maternal mortality in 2021, considering the indicator trend from 2015 to 2019. We performed a simple linear regression to obtain the increment coefficient and estimate the expected number of deaths for 2021 (i). In a second scenario, we consider maternal mortality in 2020 as a counterfactual scenario (when the Covid-19 pandemic had already been declared) (ii). Thirdly, wecorrected the predicted number for 2021 with excess general mortality in women of childbearing age in 2021, also considering the five years 2015-2019 (iii). As a fourth scenario, wecorrected the 2020 maternal mortality value for excess general mortality in women of childbearing age, also considering 2020 as a counterfactual (iv). Finally, we compare excess maternal mortality versus excess overall mortality in women of childbearing age, considering scenarios (i) and (iii). The description of the calculations can be found in Table 1.
We carried out the analysis for Brazil as a whole and for the macroregions. Statistical analysis was performed using the R program, version 4.1.2 (Viena, Austria, 2021). For all scenarios evaluated, we estimated excess maternal mortality in 2021 and its 95% confidence interval using a Poisson model with robust variance.We considered the Poisson regression model with robust variance estimation better compared to a standard Poisson regression model because it accounts for the potential violation of the assumptions that underlie the standard Poisson regression model, including when there is any suspect of heteroscedasticity, model misspecification, the presence of outliers, or when dealing with clustered or correlated data. It provides more reliable parameter estimates and standard errors, which are crucial for valid statistical inference and hypothesis testing in regression analysis. It's a valuable tool to address some of the limitations of the standard Poisson regression model.
ResultsThe year 2021 was the most critical period of the pandemic in terms of the magnitude of mortality. Compared to the trend of the previous five years, the year 2020 showed an excess mortality of 19%. Considering the same trend, the overall mortality excess in 2021 was 39%. Regarding maternal mortality, there was the same trend. While 2020 presented maternal excess mortality of approximately 40%, raising the volume of deaths to the level of almost 2 thousand deaths in that year. In 2021 there was an explosion in the number of cases, which reached the level of 3000 deaths of pregnant and puerperal women. We consider it appropriate to mention that, in 2020, deaths from covid-19 represented 19% of maternal deaths. In 2021, Covid-19 accounted for 60% of maternal deaths (Figure 1a/1b). Furthermore, we highlight that the distribution of maternal deaths over the epidemiological weeks in 2021 followed the same trend in overall deaths from Covid-19. Considering that the trend in maternal mortality followed that described for general mortality, we can assume that the pandemic penalized pregnant and puerperal women more than the general population (Figure 1c). In the end, the maternal mortality ratio for 2021 drastically exceeded the SDG target for this indicator (70 maternal deaths per 100,000 live births), reaching a level of approximately 110 maternal deaths per 100,000 live births, a level similar to that of Brazil presented in the 80's.
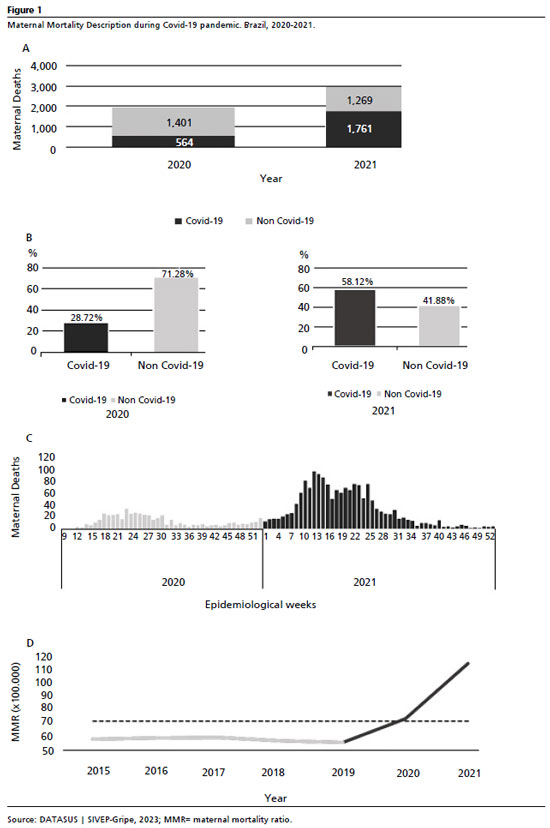
We described the scenarios in Table 1. In any scenario described, there will be excess maternal mortality in 2021 higher than general mortality, and higher than level presented in 2020. In the worst scenario, which is the comparison of maternal deaths in 2021 with what was expected, based on the trend between 2015 and 2019 (Scenario #1), we found that there were more than twice as many expected deaths (Excess = 2.11, CI95%= 1.72 – 2.50). We found a similar relationship when we calculated the excess based on 2020 mortality (Scenario #2): there was an excess mortality of 57% (CI95%= 28 - 86%) when compared to 2020. There is an excess even when the number of maternal deaths is corrected for excess overall mortality in 2021, compared to the five-year period 2015-19 (SMR = 1.52; CI95%= 1.24 – 1.80, Scenario #3) or 2020 (SMR = 1.35, CI95%= 1.10 – 1.59, Scenario #4).
Finally, the contrast between the excess of maternal deaths and general deaths (Scenarios #5 and #6) confirms the hypothesis that pregnant and postpartum women were more penalized by the pandemic than the general population. Using 2015-2019 trend as a counterfactual (Scenario #5), maternal mortality excess was 51.8% higher than general mortality excess. Using 2020 as a counterfactual (2020), maternal mortality excess was 83.7% higher than general mortality excess. The comparison with the excess of general mortality shows that pregnant and puerperal women were more penalized by Covid-19 than the general population, and the gap increased as worst pandemic was (2020
vs. 2021). In all of them, the estimates are statistically significant. In addition, we emphasize that not all deaths were caused by Covid-19 directly. However, the pandemic severely limited women's access to adequate prenatal care, delivery, and puerperium.
Analysis stratified by region demonstrates subnational heterogeneity (Table 2). For all regions, there was an excess of maternal mortality regardless of the scenario, and in all of them the excess was statistically significant. However, for the North, South, Southeast and Brazil as a whole, the scenario whose counterfactual was maternal mortality observed in 2020 was worse than the scenario whose counterfactual was the 2015-2019 five-year trend corrected for excess general mortality. For the Northeast and Midwest regions, the evidence was opposite. We also emphasize that the comparison between excess maternal mortality and overall mortality also did not show the same magnitude between regions.
DiscussionThe excess maternal mortality during the Covid-19 pandemic has an intersectoral multicausality that articulates, at least, biological factors, functioning and structure of the SUS, public policies/inequalities, and institutional crisis. Not focusing on the critical biological factors, this article focuses on social and political aspects. Our analysis converges with the field of social determinants of health.
6 For this, we assume as an initial focus the way the federal government dealt with Covid-19, marked by denialism; the delay in purchasing vaccines; fake news promoting "medicines" without any scientifically documented effectiveness; the non-adoption of a policy of social distancing and the use of masks (non-pharmacological measures); for attacking everyone who defended actions to deal with the pandemic; and, above all, for the constant change in command of the Ministry of Health, including the appointment of a Minister who admitted that
he does not know anything about SUS.7,8Coronavirus pandemic has brought to light health inequities in countries, especially concerning access to health services. Since the beginning of the Covid-19 pandemic, Brazil has been monitoring maternal mortality.
9 This concern was growing as Covid-19 started to present conditions that escaped the rule of a classic respiratory syndrome, but as a systemic condition. Aside the risk due to this biological plausibility, maternal mortality is strongly influenced by the access and availability of care resources for prenatal care, childbirth, and puerperium. The context of the pandemic creates additional barriers to prenatal care and childbirth, which directly impacts maternal mortality.
Maternal mortality is notably affected by the quality of maternity care, which involves access, availability of necessary resources, and acceptable practices for prenatal care, childbirth, and the puerperium.
4 In countries where there is inadequate access to health services during pregnancy and childbirth, maternal mortality is higher.
10 This scenario becomes more evident when the health system is overloaded, as occurred in the first two years of the pandemic.Brazil had difficulty promoting prenatal care for pregnant women. In addition, they witnessed access barriers to childbirth, and faced a low supply of intensive care beds when there was a demand for them. Now the Brazilian health system will need to turn its attention to recovering aspects of health that have been neglected during the last three years.
11We emphasize that the Executive's action led to the break with the cooperative federalism that characterizes the management of the SUS. Health policies were strongly strained by the Judiciary and Legislative Powers, which produced threats from the President of the Republic to the country's democratic stability. Consequently, the Federal Supreme Court (STF) authorized States and Municipalities to act autonomously in facing the pandemic, forcing the Executive to have minimum national planning for vaccination.
12Consequently, there was no tripartite management, yet federal coordination. The SUS, as the cases of Covid-19 pressured it, had to shift resources, equipment, and professionals (many of them getting sick and dying in the fight against the virus) to prevent the scenario from worsening.
8 This set of tragic relationships set more than 700,000 deaths caused by Covid-19 in Brazil.
13 Problems before the pandemic, such as maintaining a delivery and postpartum care network, and access to prenatal care, were even less focused by managers, multiplying. This scenario helps explaining Brazil's return to a critical scenario regarding maternal mortality.
14Although the analysis deals with the context of a particular country, we emphasize that there is sufficient evidence that during the pandemic, Brazil was the country that most increased maternal mortality.
15 We consider it appropriate to mention that, in 2018, even when the maternal mortality ratio already showed signs of retraction in Brazil,
16 35% of Brazilian health regions had levels above 70 per 100,000 live births (LB). Furthermore, over the last 20 years, the reduction has been substantial among women aged 30 to 49 years. However, in the age group of 10 to 29 years there was no significant change. In fact, national policy initiatives, such as the disclosure of the Maternal Mortality Committees, the PHPN, the PNAISM and the "
Rede Cegonha" contributed to improvements in late pregnancies; however, they were ineffective in preventing deaths among young mothers.
2 In this sense, it is important to reinforce the importance of resuming reproductive planning policies in preventing all avoidable maternal deaths, going beyond the maternal care.
Furthermore, in different scenarios of adjustment of the expected number of maternal deaths for 2021, Brazil has an excess of maternal deaths, even with correction for the excess of general mortality. In the worst-case scenario, Brazil has twice as many maternal deaths than expected, putting the country back in the uncontrolled zone of this event. Also, concerning subnational analysis, the Southeast region deserves to be highlighted, with an excess of maternal mortality 219.8% higher than the excess of general mortality.We may attribute this unexpected difference to the fact that the southeast systematically presented maternal mortality at lower levels than the rest of the country. With low numbers, slight variations in absolute numbers have a significant relative impact. Furthermore, we highlight the quality of the Maternal Death Investigation Committees in the southeast region, which makes the system more sensitive to the timely detection and closure of cases.
We observed maternal deaths caused by Covid-19 due to the different susceptibility of pregnant and postpartum women to the attack of the virus. On the other hand, we recognize that the dynamics of the pandemic have changed obstetric care, penalizing women of childbearing age by restricting access to quality prenatal care, delivery, and puerperal care. To sum up, maternal health, considered a priority of Brazilian health policies for at least 30 years, will demand special attention, under the risk of experiencing setbacks that jeopardize all the advances achieved by Brazil in this direction.
In the INTERCOVID Multinational Cohort Study
17 showed that Covid-19 in pregnancy was associated with consistent and substantial increases in severe maternal morbidity and mortality andneonatal complications when pregnant women with and without Covid-19 diagnosis. This result is corroborated by a series of cases
18 and a meta-analysis,
19 who identified that barriers to access healthcare, differences in pandemic containment measures in the country and high prevalence of concomitant risk factors for Covid-19 severe disease may play a role in the observed disparity compared to worldwide reports on maternal outcomes.
This is not a one-off situation, but a global trend. Global maternal and fetal outcomes have worsened during the Covid-19 pandemic, with an increase in maternal deaths and stillbirth. Current evidence suggests that maternal mortality mostly happened among women with previous co-morbidities.
20,21 Therefore, partially it is related to the fact that pregnant women with comorbidities including diabetes mellitus, hypertension, and cardiovascular disease were at increased risk for severe Covid-19-related outcomes, maternal morbidities, and adverse birth outcomes.
22 Still, some outcomes show considerable disparity between high-resource and low-resource settings.
23A Latin America multi-country collaborative study describe the clinical characteristics of maternal deaths associated with Covid-19. It indicates that pregnant women in Latin America faced barriers to access intensive care services when required, and it was determinant of a worsening in maternal mortality in the region.
24 In Brazil, since the beginning of pandemic, the delay in adopting public health measures necessary to control the epidemic has exacerbated the spread of the disease, resulting in several avoidable death.
25,26Although the institutional crisis, the breakdown of federalism, and the lack of national coordination in the SUS were overcome during the first half of 2023, the effects on the health system tend to persist for some time. The pressure of queues and backlogs of non-attendance on services aggravate cases. There is a need to adapt them to the new demands linked, for example, to the rehabilitation of survivors and the long covid.
Concerning the deaths of pregnant and puerperal women, if this persistence is prolonged, the problems contributing to the excess maternal mortality tend to last or even worsen. In this scenario, controlling the severity of Covid-19 via vaccines will possibly reduce maternal mortality, but with low impact due to the persistence of social and political elements. In this sense, as efforts and resource allocation toward prevention and treatment of Covid-19 continue, essential health services must be maintained, particularly in low- and middle-income countries, such as Brazil.
27Our analysis has limitations. Mortality data represent data available at the time of the study. The data, however, may change due to updates in the coming months. Another limitation concerns the low level of testing in Brazil. It prevents us from accurately knowing the number of pregnant and postpartum women infected with Covid-19. However, this information does not compromise the estimated calculation we use since mortality odds ratios are accurate when the population base is unknown. We also know that there is some imbalance between the age group in which most pregnant women are concentrated and the group with the highest prevalence of comorbidities. However, we performed our analyses disregarding the order of pregnancies, and we believe that this minimized potential selection bias.
In the end, the Covid-19 pandemic had considerable impact on maternal health, not only by leading to increased deaths, but also by increasing social health inequity.
28 Barriers to access and usage of essential health services are a challenge to achieving health-related Sustainable Development Goals. Declines in healthcare utilization during the Covid-19 pandemic amplified the pandemic's harmful impacts on health outcomes and threaten to reverse gains in reducing maternal and child mortality. The results of our analysis are sufficient to recommend that SUS preparation should include surveillance and the sectors most directly linked to confrontation measures and those who will deal with the repercussions of the emergency on using the SUS. From the experience of 2020-2022, care for pregnancy, childbirth, and the puerperium is one of those most needs to be prepared.
References1. United Nations.Goal 3: Ensure healthy lives and promote well-being for all at all ages. [access in 2023 Jul 20]. Avaliable from:
https://www.un.org/sustainabledevelopment/health/2. Motta CT, Moreira MR. Will Brazil comply with the SDG 3.1 of the 2030 Agenda? An analysis of maternal mortality, from 1996 to 2018. Ciên Saúde Colet. 2021; 26 (10): 4397-409.
3. Guimarães RM, Reis LGC, Souza Mendes Gomes MA, Magluta C, Freitas CM, Portela MC. Tracking excess maternal deaths associated with COVID-19 in Brazil: a nationwide analysis. BMC Pregnancy Childbirth. 2023; 23 (1): 22.
4. Michels BD, Iser BPM. Maternal mortality by Covid-19 in Brazil: updates. Rev Bras Saúde Mater Infant. 2022; 22(2): 445-6.
5. Souza ASR, Amorim MMR. Mortalidade materna pela COVID-19 no Brasil. Rev Bras Saúde Mater Infant. 2021; 21 (Supl. 1): 253-6.
6. Mosnaim G, Carrasquel M, Wolfson AR, Peters J, Lang D, Rathkopf M. Social Determinants of Health and COVID-19. J Allergy Clin Immunol Pract. 2023 Nov; 11 (11): 3347-55.
7. The Lancet. COVID-19 in Brazil: "So what?" [Editorial]. Lancet. 2020 May; 395 (10235): 1461.
8. Ferrante L, Duczmal L, Steinmetz WA, Almeida ACL, Leão J, Vassão RC,
et al. How Brazil's President turned the country into a global epicenter of COVID-19. J Public Health Policy. 2021; 42 (3): 439-51.
9. Joseph NT, Wylie BJ. Maternal deaths in Brazil from severe COVID-19 respiratory disease: time for a global commitment to ending health disparities. BJOG. 2020; 127 (13): 1627.
10. Orellana J, Jacques N, Leventhal DGP, Marrero L, Morón-Duarte LS. Excess maternal mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic. PLoSOne. 2022; 17 (10): e0275333.
11. Tenorio DS, Matos Brasil AG, Nogueira BG, Rolim Lima NN, Araújo JEB, Rolim Neto ML. High maternal mortality rates in Brazil: Inequalities and the struggle for justice. Lancet Reg Health Am. 2022; 14: 100343.
12. Gonçalves MR, Reis RCP, Tólio RP, Pellanda LC, Schmidt MI, Katz N,
et al. Social Distancing, Mask Use, and Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, Brazil, April-June 2020. Emerg Infect Dis. 2021; 27 (8): 2135-43.
13. Agência Brasil. Brazil hits 700,000 deaths from COVID-19. [
Internet]. [access in 2023 Jul 20]. Avaliable from:
https://agenciabrasil.ebc.com.br/en/saude/noticia/2023-03/brazil-hits-700000-deaths-covid-114. Gonçalves BMM, Franco RPV, Rodrigues AS. Maternal mortality associated with COVID-19 in Brazil in 2020 and 2021: Comparison with non-pregnant women and men. PLoS One. 2021; 16 (12): e0261492.
15. Francisco RPV, Lacerda L, Rodrigues AS. Obstetric Observatory BRAZIL - COVID-19: 1031 maternal deaths because of COVID-19 and the unequal access to health care services. Clinics (Sao Paulo). 2021; 76: e3120.
16. Guimarães RM. COVID-19 challenges Brazil to comply with agenda 2030 to reduce maternal mortality. Lancet Reg Health Am. 2023; 21: 100491.
17. Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A,
et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021; 175 (8): 817-26.
18. Takemoto MLS, Menezes MO, Andreucci CB, Knobel R, Sousa LAR, Katz L,
et al. Maternal mortality and COVID-19. J Matern Fetal Neonatal Med. 2022; 35 (12): 2355-61.
19. Di Toro F, Gjoka M, Di Lorenzo G, Santo D, Seta F, Maso G,
et al. Impactof COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect. 2021; 27 (1): 36-46.
20. Simbar M, Nazarpour S, Sheidaei A. Evaluation of pregnancy outcomes in mothers with COVID-19 infection: a systematic review and meta-analysis. J Obstet Gynaecol. 2023; 43 (1): 2162867.
21. Hessami K, Homayoon N, Hashemi A, Vafaei H, Kasraeian M, AsadiN. COVID-19 and maternal, fetal and neonatal mortality: a systematic review. J Matern Fetal Neonatal Med. 2022; 35 (15): 2936-41.
22. Smith ER, Oakley E, Grandner GW, Rukundo G, Farooq F, Ferguson K,
et al. Clinical risk factors of adverse outcomes among women with COVID-19 in the pregnancy and postpartum period: a sequential, prospective meta-analysis. Am J Obstet Gynecol. 2023; 228 (2): 161-77.
23. Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I,
et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021; 9 (6): e759-72.
24. Maza-Arnedo F, Paternina-Caicedo A, Sosa CG, Mucio B, Rojas-Suarez J, Say L,
et al. Maternal mortality linked to COVID-19 in Latin America: Results from a multi-country collaborative database of 447 deaths. Lancet Reg Health Am. 2022; 12: 100269.
25. Szwarcwald CL, Boccolini CS, Silva de Almeida W, Soares Filho AM, Malta DC. COVID-19 mortality in Brazil, 2020-21: consequences of the pandemic inadequate management. Arch Public Health. 2022; 80 (1): 255.
26. Diniz D, Brito L, Rondon G. Maternal mortality and the lack of women-centered care in Brazil during COVID-19: Preliminary findings of a qualitative study. Lancet Reg Health Am. 2022; 10: 100239.
27. Ahmed T, Roberton T, Vergeer P, Hansen PM, Peters MA, Ofosu AA,
et al. Healthcare utilization and maternal and child mortality during the COVID-19 pandemic in 18 low- and middle-income countries: An interrupted time-series analysis with mathematical modeling of administrative data. PLoS Med. 2022; 19 (8): e1004070.
28. Castañeda-Orjuela C, Hilarion Gaitan L, Diaz-Jimenez D, Cotes-Cantillo K, Garfield R. Maternal mortality in Colombia during the COVID-19 pandemic: time series and social inequities. BMJ Open. 2023; 13 (4): e064960.
Author's contribution: Guimarães RM and Moreira MR: conception, data analysis, critical review and final drafting of the manuscript. All the authors have approved the final version of the article and declare no conflict of interest.
Received on March 7, 2023
Final version presented on December 29, 2023
Approved on February 2, 2024
Associated Editor: Leila Katz
 ; Marcelo Rasga Moreira2
; Marcelo Rasga Moreira2