ABSTRACT
OBJECTIVES: to analyze the prognostic nutritional index and factors associated with mortality in children and adolescents with heart disease who underwent cardiac surgery.
METHODS: this is a longitudinal, retrospective study that included 98 children and adolescents with heart disease from 0 to 14 years old, and assessed the prognostic nutritional index and nutritional status, through the body mass index for age, weight for height, weight for age and height for age. Multiple logistic regression analysis was performed.
RESULTS: malnutrition was present in 27 patients, 68 were categorized as having a low prognostic nutritional index and 16 died. In the adjusted analysis, malnutrition (OR=4.11; CI95%=1.26-13.40; p=0.019), the low body mass index for age (OR=4.14; CI95%=1.26-13.61; p=0.019), low weight for height (OR=4.15; CI95%=1.29-13.35; p=0.017) and low weight for age (OR=5.20; CI95%=1.39-19.43; p=0.014) were associated with mortality.
CONCLUSIONS: malnutrition, low body mass index for age, weight for height and weight for age had shown a significant association with mortality. Despite being an easily applicable indicator of nutritional status, the findings suggest no association between the prognostic nutritional index and mortality in patients with congenital heart disease after cardiac surgery.
Keywords:
Nutritional status, Infant mortality, Cardiovascular diseases, Cardiac surgical procedures
RESUMO
OBJETIVOS: analisar o índice nutricional prognóstico e os fatores associados a mortalidade em crianças e adolescentescardiopatas submetidas à cirurgia cardíaca.
MÉTODOS: estudo longitudinal, retrospectivo, que incluiu 98 crianças e adolescentes cardiopatas entre zero a 14 anos e avaliou o índice nutricional prognóstico e o estado nutricional, através dos indicadores índice de massa corporal para idade, peso para estatura, peso para idade e estatura para idade. Foi realizada análise de regressão logística múltipla.
RESULTADOS: a desnutrição esteve presente em 27 pacientes, 68 foram categorizados como baixo índice nutricional prognóstico e 16 foram a óbito. Na análise ajustada, a desnutrição (OR=4,11; IC95%=1,26-13,40; p=0,019), o baixo índice de massa corporal para idade (OR=4,14; IC95%=1,26-13,61; p=0,019), o baixo peso para estatura (OR=4,15; IC95%=1,29-13,35; p=0,017) e baixo peso para idade (OR=5,20; IC95%=1,39-19,43; p=0,014) apresentaram associação com a mortalidade.
CONCLUSÃO: desnutrição, baixo índice de massa corporal para idade, peso para estatura e peso para idade mostraram associação significativa com a mortalidade. Apesar de ser um indicador do estado nutricional de fácil aplicação não foi observada associação do índice nutricional prognóstico com a mortalidade em pacientes com cardiopatias congênitas após cirurgia cardíaca.
Palavras-chave:
Estado nutricional, Mortalidade infantil, Cardiopatias, Procedimentos cirúrgicos cardíacos
IntroductionMalnutrition is a frequent phenomenon in children and adolescents with cardiovascular disease, and the main responsible factor is the inefficient usage of nutrients, due to the increase of energetic expenditure by virtue of clinical conditions, which are inherent to cardiac alterations.
1 Accordingly, they represent a major cause of recurrent hospitalizations and are associated with high rates of mortality.
2Around 80% of children with cardiovascular diseases need surgical intervention, whether corrective or palliative.
3 The evolution of surgical techniques enabled higher rate of survival, whereas the presence of malnutrition in these patients increases the risk of complications in the postoperative period due to higher metabolic demand.
4Nutritional status represents an important role in the incidence of morbidity and mortality in the postoperative period.
5 In this way, it is necessary to promote actions related to nutritional assessment even in the postoperative period. Nutritional assessment may establish and even prevent risk situations after surgery, observing that inadequate nutritional status in the period that antecedes it is frequently worsened in the postoperative period.
3,6The determination of nutritional status is complex, once many indexes are necessary to perform a complete and accurate description, such as food intake, anthropometric data and biochemical parameters.
6 Various tools were created in order to assess nutritional status.
7 Onodera
et al.
8 suggested the use of the Prognostic Nutritional Index (PNI) to assess the nutritional status of patients with many diseases.
6,9 It is an indicator that quantifies nutritional and immunological aspects from serum albumin and Total Lymphocyte Count (TLC)
8 and it has been largely used to assess the risk of surgical morbimortality.
5PNI seems to be an easily applicable tool; objective, fast and easy to obtaindata, although little evidence in pediatrics reports the usage of this indicator.
6,10 In one of them, the PNI was evaluated as predictor of worsening of kidney function in children with chronic kidney disease.
6There is only one study carried out with children that underwent cardiac surgery, however, the rate of mortality outcome was not analyzed and only patients under 18 years of age were included.
10 Due to the gap in literature, the aim of this study was to analyze the PNI and factors associated with mortality in children and adolescents that underwent cardiac surgery.
MethodsThis is a longitudinal retrospective study, with quantitative approach. The study population was composed by children and adolescents between 0 to 14 years of age that underwent cardiac surgery from January 2017 to May 2020. The survey was carried out in the University Hospital of the Federal University of Maranhão (HU-UFMA – Portuguese acronym), at Mother and Child Unit, located at the city of São Luís, which provides care exclusively for the Unified Health System (SUS – Portuguese acronym) and represents a structure of reference for pediatric cardiac surgery in the state.
The sample size calculation was performed using Microsoft Office Excel
®software, based on the number of patients that underwent cardiac surgery in the Hospital’s pediatrics sector, in the period between January 2017 and May 2020. Considering a sampling error of 5% and a 95% confidence interval for heterogeneous samples, it was established as minimum sample 89 patients. Due to the sample size in relation to the population, data collection was performed with all of the patients, posteriorly withdrawing those who match the non-inclusion criteria.
The non-inclusion criteria were: 1. genetic syndromes (Turner syndrome, Down Syndrome, or unknown syndrome); 2. Chronic kidney disease; 3. Hepatic insufficiency. A total of 114 patients underwent surgery in the evaluated period, 98 patients were included (Figure 1).
Data collection was performed in specific charts and forms from the Nutrition Service. Anthropometric data, weight and height, were collected in the admission of patients and biochemical exams, C-Reactive Protein (CRP), albumin and TLC, were collected at the postoperative period.
The explanatory variables were: sex, age (<2 years/≥2 years), (CRP) (<0.5mg/L/≥0.5mg/L), albumin, TLC, types of surgery, types of cardiovascular disease, pulmonary hypertension (yes/no), presence of malnutrition (yes/no), weight for height (W/H), weight for age (W/A), body mass index for age (BMI/A), height for age (H/A) and PNI. The outcome variable: death.
Cardiovascular diseases were categorized as cyanotic and acyanotic. Cardiac surgeries were classified with the STS-EACT (Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery) mortality score, which stratifies mortality according to data from each surgical procedure in five categories.
11The H/A (0 to 14 years), BMI/A (0 to 14 years), W/H (up to 5 years) and W/A (up to 10 years) indicators of every patients were assessed and classified as malnourished (yes/no) using the classification of the recommended indicator for age: W/H in <2 years and BMI/A in ≥2 years.
12 The H/A, BMI/A, W/H and W/A indicators were classified as low (yes/no) and analyzed with the Z-score, considering the < -2 cutoff in the World Health Organization (WHO) 2006/2007 growth curves, using the software WHO Anthro
® 3.2.2 and WHO Anthro Plus
® 1.0.4.
The PNI was calculated using the following formula: 10x serum albumin value (g/dl) + 0.005 x TLC in the peripheral blood (by mm
3).
8 Based on this index, patients were divided in two groups: high PNI (PNI≥55) and low PNI (PNI<55).
10In order to minimize missing data in the database (6%), the multiple imputation strategy was used. Once they are quantitative variables, the chosen method was the Predictive Mean Matching. Multiple imputation was performed using the public domain application Multivariate Imputation by Chained Equations (MICE), operated in the R software.
13The descriptive statistics are displayed as± meanstandard deviation or median and interquartile range for numerical variables and as frequency and proportion for categorical variables. The normal distribution of numerical variables was tested with the Saphiro-Wilk test. The variables with normal distribution were described as ± mean standard deviation, theothers as median and interquartile range.
Simple (unadjusted) and multiple (adjusted) logistic regression analyses between were performed between the study variables (sex, age, gestational age, CRP, albumin, TLC, cardiovascular disease, STS-EACTS mortality score, type of cardiovascular disease, PNI classification, malnutrition, low H/A) and the outcome variable (death). Continuous variables without evidence of linearity with death probability were analyzed categorically (age and CRP).
The selection of confounding variables for multiple logistic regression occurred by means of the building of a theoretical model, DAG (Directed Acyclic Graphs) with the DAGitty
® software (Figure 2). The results are shown in the form of Odds Ratio (OR) with confidence interval of 95%. STATA® 14.0 software was used in all analyses.
The present study was locally approved by the Research Ethics Committee of the Federal University of Maranhão (opinion nº. 4.240.637, CAAE n° 36433520.1.0000.5086).
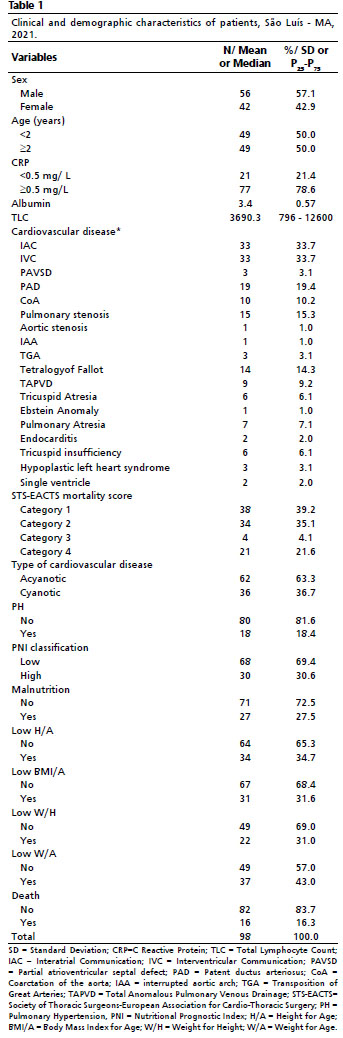
ResultsThe clinical and demographic characteristics of patients with cardiovascular diseases are shown in Table 1. Of the 98 participants, most were men (57.1%), half had less than 2 years of age and the most prevalent cardiovascular disease was interatrial communication (33.7%). Of the performed surgeries, 39.2% were classified in category 1 of the STS-EACTS score and there were no surgery classified in category 5.
Regarding the nutritional status in the postoperative period of patients, 69.4% were categorized as having low PNI. Malnutrition was observed in 27.5% of patients, and when assessed by the indicators, 34.7% had low H/A; 31.6% low BMI/A; 31% low W/H; 43% low W/A. 16.3% of patients died after cardiovascular surgery (Table 1).
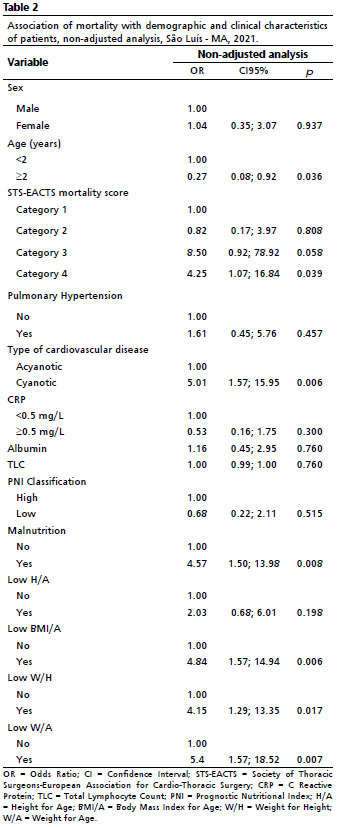
In the non-adjusted analysis, age, the STS-EACTS mortality score, cyanotic heart disease, malnutrition, low BMI/A, W/H and W/A shown association with mortality (Table 2).
Patients with age higher than 2 years shown a decrease of 73% in chances of death (OR=0.27; CI95%=0.08-0.92;
p=0.036%. The association between STS-EACTS mortality score and death outcome was significant only in category 4, that is, surgeries belonging to this category shown higher chances of leading patients to death. (OR= .25; CI95%=1.07-16.84;
p=0.039). Likewise, cyanotic cardiovascular diseases increased chances of death up to 5 times (OR=5.01; CI95%=1.57-15.95;
p=0.006) (Table 2).
The anthropometric indicators, low BMI/A (OR= 4.84; CI95%=1.57-14.94;
p=0.006), low W/H (OR=4.15; CI95%=1.29-13.35;
p=0.017) and low W/A (OR=5.4; CI95%=1.57-18.52;
p=0.007) as well shown association with mortality. Compared to patients with adequate nutritional status, malnourished patients had shown 4 times more chances of death (OR=4.57; CI95%=1.07-16.84;
p=0.039) (Table 2).
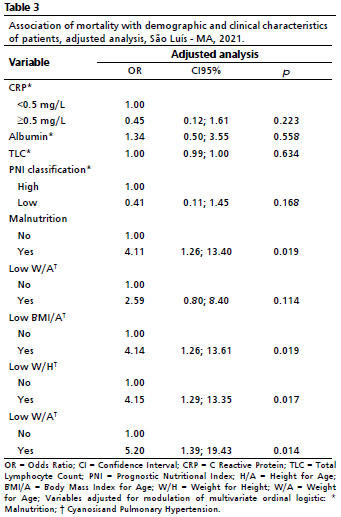
After adjusting analysis for the confounding factors (Table 3), there were no associations of PNI, CRP, albumin, TLC and H/A with mortality. Patients classified as malnourished were 4 times more likely to die. (OR=4.11; CI95%=1.26-13.40;
p=0.019).
The anthropometric indicator low BMI/A had shown association with mortality even after adjusting for confounding factors (OR=4.14; CI95%=1.26-13.61;
p=0.019), as well as low W/H (OR= 4.15; CI95%=1.29-13.35;
p=0.017) and low W/A (OR=5.20; CI95%=1.39-19.43;
p=0.014) (Table 3).
DiscussionCardiovascular diseases are the most common congenital malformations worldwide and are an important cause of early morbidity and mortality.
14 The present study evidenced that older children were less likely to die after cardiovascular surgery. One of the possible hypothesis would be that patients who underwent surgery at older age usually have less complex cardiovascular diseases,
15 and therefore, show higher chances of survival after surgery.
The use of stratification of cardiovascular surgeries by relatively similar levels of complexity, such as performed in our study, is necessary to the mortality analysis due to the high number of different surgical procedures in patients with congenital cardiovascular diseases.
16 Agreeing with the present results, a comparative study between two tools of mortality stratification, STS-EACTS tool among them, identified that children with higher scores, that is, with need for more complex surgeries, had shown higher mortality risk.
17The results of this study corroborates the hypothesis that the postoperative nutritional status can be decisive to increase the chance of mortality after cardiovascular surgery.
18,19 The presence of malnutrition in studied patients increased the chance of mortality 4 times, reinforcing negative effects of malnutrition that are widely documented in the literature as factors of morbimortality in cardiovascular surgery.
18-21The described association may be explained by the postoperative metabolic response, characterized by altered energetic demands, complex inflammatory status and higher protein catabolism,
3,22 added to malnutrition, which can by itself impair the results of the corrective surgery.
19Thus, postoperative nutritional diagnosis in cardiovascular surgeries allows for early therapeutic intervention, decreasing risks of postoperative complications.
23 Although these results are not recent, they reinforce the relevance of routine nutritional assessment in patients with congenital cardiovascular diseases, specially before surgery.
One of the combinations of albumin with the TLC found in the literature is the PNI, by Onodera
et al.,
8 which is easy to calculate
24-26 using preoperative laboratory data,
25 which in turn are objective markers of low cost.
24 Initially associated with surgical risk for patients with gastrointestinal malignancy,
8 PNI is currently used as a nutritional marker predictive of mortality in patients with several diseases, such as cancer,
25,26 Non-tuberculous mycobacterial infection,
27 chronic kidney disease,
28 burn wounds
29 and cardiovascular diseases.
9,24,30The exact mechanisms for which PNI is related to postoperative prognosis are not well comprehended, however, some of these potential mechanisms were reported. Firstly, the serum albumin level is widely used to assess nutritional and inflammatory systemic aspects of patients
26,28,29 and secondly, the lymphocytes represent a major role in immune response, and their functions and values are deeply altered after sepsis and other acute lesions such as complex surgeries.
29Regarding cardiovascular surgeries, it was observed that patients with coronary artery disease, with a mean follow-up of 7 years, had higher incidence not only of mortality by all causes, but also of cardiac mortality when presented lower preoperative PNI.
24A study carried out with 131 patients over 18 years old, accompanied for one year, in order to investigate the impact of the PNI in mortality by infectious endocarditis, demonstrated an association of this index with the mortality rate, being the PNI identified as independent predictor of mortality during hospitalization.
30 It was also observed an association with mortality in the postoperative period of cardiovascular surgery in adult patients, moreover, a higher PNI was related to a better survival rate.
9In the current study, this association was not observed.Factors such as sample size, small number of outcomes and assessed age group might explain this finding. This demonstrates that despite of having a well-proven prognostic value in abdominal and gastrointestinal surgeries,
29 there is little evidence about this tool in pediatrics.
We can mention the missing data as another limitation of our study, which was partially solved by multiple imputation. This method has been recommended once the exclusion of observations with missing data and analysis restriction to complete observations diminish the sample size and generates biased estimates.
13The strengths include the analysis of association of the PNI with mortality in children and adolescents who underwent cardiovascular surgery, with evidence that it is one of the first studies to approach such association, besides the multiple logistic regression analysis adjusted to the variables represented by the DAG, allowing for the adjustments to be executed by confounding variables, averting spurious associations.
We conclude that age, STS-EACTS mortality score, cyanotic cardiac disease, malnutrition, low BMI/A, W/H and W/A had shown significant association with mortality. In spite of being an indicator of nutritional status of easy application, there was no observed association of the PNI with mortality in children with cardiovascular disease after cardiovascular surgery.
References1. Lewis KD, Conway J, Cunningham C, Larsen BMK. Optimizing Nutrition in Pediatric Heart Failure: The Crisis Is Over and Now It’s Time to Feed. Nutr Clin Pract. 2018 Jun; 33 (3): 397-403.
2. Cappellesso VR, Aguiar AP. Cardiopatias congênitas em crianças e adolescentes: caracterização clínico-epidemiológica em um hospital infantil de Manaus-AM. Mundo Saúde. 2017 Mar; 41 (2): 144-53.
3. Souza NMG, Andrade GV, Bastos LF, Dantas AVVC, Cavalcante CTMB, Barbosa LP,
et al. Associação do estado nutricional e os desfechos clínicos em cirurgia cardíaca pediátrica. Acta Paul Enferm. 2020; 33: 1-8.
4. Silva L, Guedes JC, Simone RM, Melo V, Sousa CY. Preoperative nutritional risk through total lymphocyte content, serum albumine levels and strongkids tribal tool in children submitted to cardiac surgeries. Nutr Clin Diet Hosp. 2019; 39 (3): 50-7.
5. Hayashi J, Uchida T, Ri S, Hamasaki A, Kuroda Y, Yamashita A,
et al. Clinical significance of the prognostic nutritional index in patients undergoing cardiovascular surgery. Gen Thorac Cardiovasc Surg. 2020 Aug; 68 (8): 774-9.
6. Zhang H, Tao Y, Wang Z, Lu J, Bhatt GC. Evaluation of nutritional status and prognostic impact assessed by the prognostic nutritional index in children with chronic kidney disease. Medicine (Baltimore). 2019 Aug; 98 (34): e16713.
7. Lee SI, Ko KP, Choi CH, Park CH, Park KY, Son KH. Does the prognostic nutritional index have a predictive role in the outcomes of adult cardiac surgery? J Thorac Cardiovasc Surg. 2020 Jul; 160 (1): 145-53.
8. Onodera T, Goseki N, Kosaki G. [Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients]. 1984 Sep; 85 (9): 1001-5. Japanese
9. Cheng YL, Sung SH, Cheng HM, Hsu PF, Guo CY, Yu WC,
et al. Prognostic Nutritional Index and the Risk of Mortality in Patients With Acute Heart Failure. J Am Heart Assoc. 2017 Jun; 6 (6): e004876.
10. Wakita M, Fukatsu A, Amagai T. Nutrition assessment as a predictor of clinical outcomes for infants with cardiac surgery: Using the prognostic nutritional index. Nutr Clin Pract. 2011 Apr; 26 (2): 192-8.
11. O’Brien SM, Clarke DR, Jacobs JP, Jacobs ML, Lacour-Gayet FG, Pizarro C,
et al. An empirically based tool for analyzing mortality associated with congenital heart surgery. J Thorac Cardiovasc Surg. 2009 Nov; 138 (5): 1139-53.
12. Mehta NM, Skillman HE, Irving SY, Coss-Bu JA, Vermilyea S, Farrington EA,
et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Pediatric Critically Ill Patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. J Parenter Enteral Nutr. 2017 Jul; 41 (5): 706-42.
13. Camargos VP, César CC, Caiaffa WT, Xavier CC, Proietti FA. Imputação múltipla e análise de casos completos em modelos de regressão logística: uma avaliação prática do impacto das perdas em covariáveis. Cad Saúde Pública. 2011 Dez; 27 (12): 2299-313.
14. Jortveit J, Klcovansky J, Eskedal L, Birkeland S, Døhlen G, Holmstrøm H. Endocarditis in children and adolescents with congenital heart defects: a Norwegian nationwide register-based cohort study. Arch Dis Child. 2018 Jul; 103 (7): 670-4.
15. Erikssen G, LiestØl K, Seem E, Birkeland S, Saatvedt KJ, Hoel TN,
et al. Achievements in congenital heart defect surgery : A prospective, 40-year study of 7038 patients. Circulation. 2015 Jan; 131 (4): 337-46.
16. Cavalcanti PEF, Oliveira Sá MPB, Santos CA, Esmeraldo IM, Chaves ML, Lins RFA,
et al. Estratificação da complexidade em cirurgias de cardiopatias congênitas: Comparação dos modelos Risk Adjustment for Congenital Heart Surgery (RACHS-1), escore básico de Aristóteles e escore de mortalidade da Society of Thoracic Surgeons-European Association for Cardio-Thoracic surgery (STS-EACTS). Braz J Cardiovasc Surg. 2015; 30 (2): 148-58.
17. Bobillo-Perez S, Sanchez-de-Toledo J, Segura S, Girona-Alarcon M, Mele M, Sole-Ribalta A,
et al. Risk stratification models for congenital heart surgery in children: Comparative single-center study. Congenit Heart Dis. 2019 Nov; 14 (6): 1066-77.
18. Radman M, Mack R, Barnoya J, Castañeda A, Rosales M, Azakie A,
et al. The effect of preoperative nutritional status on post-operative outcomes in children undergoing surgery for congenital heart defects in San Francisco (UCSF) and Guatemala city (UNICAR). J Thorac Cardiovasc Surg. 2014 Jan; 147 (1): 442-50.
19. Lim CYS, Lim JKB, Moorakonda RB, Ong C, Mok YH, Allen JC,
et al. The Impact of Pre-operative Nutritional Status on Outcomes Following Congenital Heart Surgery. Front Pediatr. 2019 Oct; 7: 429.
20. Le Roy C, Larios G, Springmüller D, Clavería C. Nutritional assessment in infants with congenital heart disease: Comparison of two anthropometric classifications. Rev Chil Pediatr. 2017 Dec; 88 (6): 744-50.
21. Ross F, Latham G, Joffe D, Richards M, Geiduschek J, Eisses M, et al. Preoperative malnutrition is associated with increased mortality and adverse outcomes after paediatric cardiac surgery. Cardiol Young. 2017 Nov; 27 (9): 1716-25.
22. Ruiz AJ, Buitrago G, Rodríguez N, Gómez G, Sulo S, Gómez C, et al. Clinical and economic outcomes associated with malnutrition in hospitalized patients. Clin Nutr. 2019 Jun; 38 (3): 1310-6.
23. Seltzer MH, Bastidas JA, Cooper DM, Engler P, Slocum B, Fletcher HS. Instant Nutritional Assessment. J Parenter Enter Nutr. 1979; 3 (3): 157-9.
24. Wada H, Dohi T, Miyauchi K, Jun S, Endo H, Doi S, et al. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J Cardiol. 2018 Aug; 72 (2): 155-61.
25. Cadwell JB, Afonso AM, Shahrokni A. Prognostic Nutritional Index (PNI), independent of frailty is associated with six-month postoperative mortality. J Geriatr Oncol. 2020 Jun; 11 (5): 880-4.
26. Zhang W, Ye B, Liang W, Ren Y. Preoperative prognostic nutritional index is a powerful predictor of prognosis in patients with stage III ovarian cancer. Sci Rep. 2017 Aug; 7 (1): 9548.
27. Hachisu Y, Murata K, Takei K, Tsuchiya T, Tsurumaki H, Koga Y,
et al. Prognostic nutritional index as a predictor of mortality in nontuberculous mycobacterial lung disease. J Thorac Dis. 2020 Jun; 12 (6): 3101-9.
28. Barutcu Atas D, Tugcu M, Asicioglu E, Velioglu A, Arikan H, Koc M,
et al. Prognostic nutritional index is a predictor of mortality in elderly patients with chronic kidney disease. Int Urol Nephrol. 2022 May; 54 (5): 1155-62.
29. Seo YJ, Kong YG, Yu J, Park JH, Kim SJ, Kim HY,
et al. The prognostic nutritional index on postoperative day one is associated with one-year mortality after burn surgery in elderly patients. Burn Trauma. 2021; 9: tkaa043.
30. Kahraman S, Agus HZ, Kalkan AK, Uzun F, Ertürk M, Kalkan ME,
et al. Prognostic nutritional index predicts mortality in infective endocarditis. Turk Kardiyol Dern Ars. 2020 Jun; 48 (4): 392-402.
Received on August 30, 2021
Final version presented on February 18, 2022
Approved on May 9, 2022
Author’s contributionSilva BM: conception and writing of the article; collection, analysis and interpretation of data. Batista CLC, Pires BRF, Oliveira EC and Lima Jr. JRM: critical review. Barros TA: data collection. Cruvel JMS: analysis and interpretation of data. Statistical analysis and writing. All authors approved the final version of the article and declare no conflict of interest.
 ; Christyann Lima Campos Batista 2
; Christyann Lima Campos Batista 2 ; Bruna Renata Fernandes Pires 3
; Bruna Renata Fernandes Pires 3 ; Eliete Costa Oliveira 4
; Eliete Costa Oliveira 4 ; Tatiana Abreu Barros 5
; Tatiana Abreu Barros 5 ; José de Ribamar Medeiros Lima Júnior 6
; José de Ribamar Medeiros Lima Júnior 6 ; Juliana Moreira da Silva Cruvel 7
; Juliana Moreira da Silva Cruvel 7