ABSTRACT
OBJECTIVES: describe the profile of medication use and adherence, and the association with clinical and sociodemographic characteristics of high-risk pregnant women attended at a university hospital.
METHODS: cross-sectional study with data collected through a questionnaire applied on 386 pregnant women.
RESULTS: most participants were seen only by the gynecologist (75.1%), started prenatal in the first gestational trimester (86.8%), did not plan the pregnancy (61.9%), and performed an average of 8.2 (SD=4.4) prenatal consultations. The most frequent diagnoses were arterial hypertension (20.5%) and diabetes mellitus (19.7%). Prevalence of medication use was 99.7%, with an average of 5.1 (SD=2.1) medication per woman and 12.7% self-medication. Antianemics (88.9%) and analgesics (63.2%) were the most prevalent classes and 17.9% of the women reported the use of medication with significant gestational risk. Only 36.5% were considered adherent, 32.9% declared they were unaware of the indication of the medication in use and 42% did not receive guidance on the use of the medication during pregnancy. There is no evidence of association between the number of the medication used and clinical and sociodemographic aspects.
CONCLUSIONS: there is a need to develop strategies to improve the care of this population, with emphasis on strengthening multi-professional care.
Keywords:
High-risk pregnancy, Medication use, Pharmacoepidemiology
RESUMO
OBJETIVOS: descrever o perfil de utilização de medicamentos e de adesão, e a associação com as características clínicas e sociodemográficas de gestantes de alto risco atendidas em um hospital universitário.
MÉTODOS: trata-se de um estudo transversal com dados coletados mediante um questionário estruturado aplicado à 386 gestantes.
RESULTADOS: a maior parte das participantes era acompanhada apenas pelo ginecologista (75,1%), iniciou o pré-natal no primeiro trimestre gestacional (86,8%), não planejou a gravidez (61,9%) e realizou em média 8,2 (DP=4,4) consultas de pré-natal. Os diagnósticos mais frequentes foram hipertensão arterial (20,5%) e diabetes mellitus (19,7%). A prevalência de uso de medicamentos foi 99,7%, com média de 5,1 (DP=2,1) medicamentos por mulher e 12,7% de automedicação. Os antianêmicos (88,9%) e analgésicos (63,2%) foram as classes farmacológicas mais prevalentes e 17,9% das gestantes referiram uso de fármacos com risco gestacional relevante. Apenas 36,5% das gestantes foram consideradas aderentes ao tratamento, 32,9% declararam desconhecer a indicação dos medicamentos em uso e 42% não receberam orientações sobre o uso de medicamentos durante a gestação. Não há evidências de associação entre o número de medicamentos utilizados e os aspectos clínicos e sociodemográficos.
CONCLUSÃO: é necessário desenvolver estratégias para melhorar o atendimento desta população e o uso racional de medicamentos, com ênfase no fortalecimento do cuidado multiprofissional.
Palavras-chave:
Gravidez de alto risco, Uso de medicamentos, Farmacoepidemiologia
IntroductionPregnancy should be seen as a physiological event inherent to the health of the woman who opts for motherhood. However, the pregnant state promotes changes in the metabolic processes, and in some pregnant women it can lead to unfavorable clinical conditions for the health of the mother, of the fetus, or of the newborn, which is called high-risk pregnancy.
1Certain factors contribute to an unfavorable gestational prognosis, among which the following can be highlighted: the mother’s age, harmful sociodemographic conditions, previous reproductive history, obstetric disease in the current pregnancy, and previous or acquired health problems during gestational evolution, such as hypertension, diabetes, obesity, and among others.
2The pharmacological management of symptoms, complications, and comorbidities during pregnancy is a common occurrence, and this approach is even more necessary in high-risk pregnant women. Thus, the use of medication by pregnant women has been the object of study by several researchers, especially after the 1950s, with the notorious incident caused using thalidomide. This medication was used in the management of nausea and vomiting during pregnancy and was responsible for the birth of around 10,000 children with phocomelia, a congenital malformation which is considered rare.
3Clinical studies involving analysis of the medication effects used during pregnancy find ethical impediments related to embryo/fetal exposure to undesirable effects. Consequently, most drugs are placed on the market without a well-established safety profile regarding their use by pregnant women. In this context, pharmaco-epidemiological studies are an important tool to better understand the profile of medication use and its effects on this population.
4Considering the limited number of publications addressing the use of medications by high-risk pregnant women in Brazil and the factors associated thereto, the present study aimed to describe the profile of medications use and adherence to pharmacotherapy and the association with clinical and sociodemographic characteristics of high-risk pregnant women treated at a university hospital.
MethodsThis is a cross-sectional study conducted at the Outpatient Clinic for High-Risk Pregnant Women at the
Hospital das Clínicas da Faculdade de Medicina in Ribeirão Preto,
Universidade de São Paulo of São Paulo, Brazil (HCFMRP-USP), located in the city of Ribeirão Preto (in the state of São Paulo), between May 2014 and August 2015. This clinic is composed of a multi-professional team and is subdivided into five specialties, namely: infectious diseases in obstetrics; obstetric endocrinology; fetal and twin malformations; gestational hypertension; and prematurity and obesity.
The conduct of the research was approved with a technical advice registered in the
Sistema Nacional de Informação(National Information System) on Ethics in Research involving Human Beings (CAAE nº 12830113.4.0000.5403).
The study population consisted of high-risk pregnant women in prenatal care at HCFMRP-USP, with a minimum age of 18 years and a gestational age of at least 12 weeks. The impossibility for the pregnant woman to express herself individually was adopted as the sole exclusion criterion.
The sample size was estimated considering the calculation for prevalence studies.
5 A 95% confidence coefficient and an absolute precision of 5% were adopted for the proportion estimate. To maximize the variance, this proportion was considered equal to 50% in each stratum, resulting in a minimum sample size of 384 patients, distributed among the five specialties of the outpatient clinic for high-risk pregnant women, in proportion to the average medical care for each one.
Individual interviews were conducted to collect data: sociodemographic (age, education, professional status, income, race, marital status and place of residence); access to health services (access to a private health plan, follow-up with physicians of another specialty, in addition to the gynecologist/obstetrician and follow-up with another health professional); on pregnancy (parity, pregnancy planning, gestational age at the beginning of prenatal care, place of beginning of prenatal care, number of prenatal consultations, and ultrasounds performed up to the time of the interview); and information on medication and correlates (data on prescribed medication and self-medication use of medications without a medical prescription or indication of a health professional
, knowledge of the indication and adherence to treatment).
The medicationwere listed according to the Anatomical Therapeutic Chemical (ATC) classification
6 and the category of gestational risk proposed by the American agency Food and Drug Administration (FDA).
7 According to FDA, medications are distributed in the following categories: A (absent risk): medication did not show risk to the fetus in the first trimester of pregnancy in controlled studies with pregnant women; B (no evidence of risk in humans): no controlled studies in pregnant women or animal studies have shown fetal risk or revealed unconfirmed risks in controlled studies with pregnant women; C (risk cannot be excluded): no studies in animals and pregnant women, or studies in animals revealed risks not confirmed in studies with pregnant women; D (positive risk evidence): positive evidence of human fetal risk, but the potential benefits may justify the risk in cases of serious or life-threatening illnesses, and there are no other safer medication; X (contraindicated use in pregnancy): studies in animals and pregnant women have shown evidence of risk to the fetus greater than any benefit to the pregnant woman.
Adherence was assessed using the modified Morisky-Green scale, a structured form with six closed-ended questions, with dichotomous answers (“yes” or “no”).
8 Pregnant women who had a percentage of correct answers greater than or equal to 80 % in the test were considered adherent to pharmacotherapy, and the others were considered non-adherent.
9Summary measures were calculated for all variables under study. A significance level of 5% and a 95% confidence interval for analytical statistics were adopted. Logistic regression models were applied to investigate the association between the dependent variable “number of medications”, categorized as “0-4 medication” and “≥5 medication”, and the independent variables (sociodemographic and clinical), by which the Odds Ratios (OR) and their respective confidence intervals were calculated, allowing the assessment of the existence and size of the association as variables. The logistic regression model was carried out considering that pregnant women are seen in different outpatient clinics, which were considered non-hierarchical clusters. Thus, when performing the logistic regression model, a correlation matrix was used to inform the model of the conglomerate to which each pregnant woman belongs and mathematically adjust its characteristics, producing the estimated effects (OR) of each variable studied adjusted for the differences in distributions that each conglomerate can present. The cut-off value of five or more medications was chosen to characterize the polypharmacy situation.
10ResultsA total of 386 pregnant women were interviewed. Among the 450 women approached, 46 (10.2 %) did not meet the inclusion criteria and 18 (4%) did not accept to participate. Pain and malaise were the main causes of the refusals.
Age ranged from 18 to 46 years, with an average of 28.7 years (SD: 6.2). About 30 % of pregnant women had 9 years or less of schooling, 47.7 % were white, most did not work (54.7 %), had per capita income below one minimum wage (66.1 %), were dependent exclusively on the
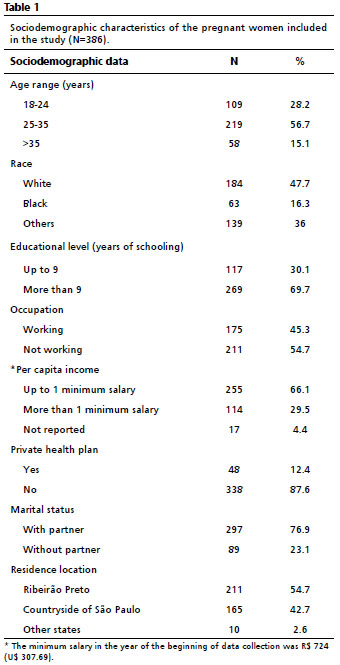
Sistema Unico de Saúde (SUS) (Public Health System) (87.6%) and had a partner (76.9 %) (Table 1). Most of the study participants also reported not following up with a physician from another specialty besides the gynecologist (75.1%; n=290) or with another health professional (75.6%; n=292).
In this study, 31.6% of the participants were primiparous; 61.9% had not planned the pregnancy, and 29.3% had a history of previous abortion. Among the interviewees, 86.8% (n=335) started prenatal care in the first trimester of pregnancy, 12.2% (n=47) in the second trimester and one pregnant woman reported having started monitoring in the last gestational trimester. Three women were unable to mention the time when prenatal care started. A portion of these pregnant women (10.6%; n=41) discovered pregnancy in the second trimester. The average number of prenatal consultations per pregnant woman was 8.2 (SD=4.4) and the average number of ultrasounds was 3.5 (SD=3.2).
At the time of the interview, 61.9% (n=239) of the women were in the last trimester, 33.2 % (n=128) in the second, and 4.9% (n=19) were in the first trimester.
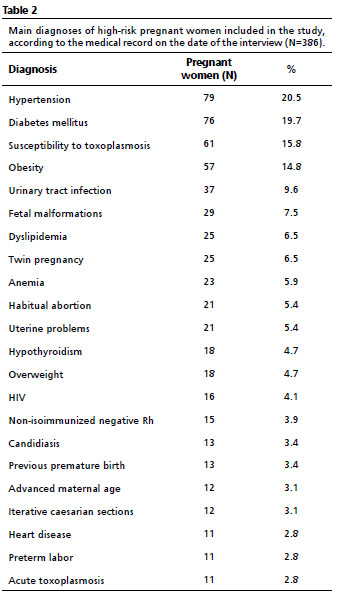
The most frequent diagnoses presented by high-risk pregnant women, according to the medical records data on the date of the interview, were arterial hypertension and diabetes mellitus (Table 2).
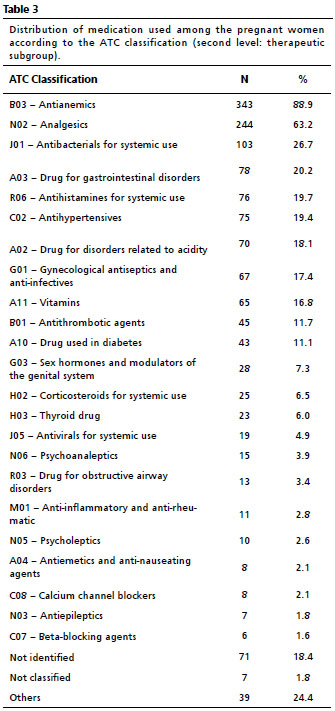
Regarding the use of medication, 99.7% (n=385) of the pregnant women had used at least one medication during pregnancy until the time of the interview, ranging from 0 to 15 and with an average of 5.1 d medication per woman (SD=2.1). A total of 160 medications containing 157 different active principles were used. Self-medication was reported by 12.7% (n=49) of the pregnant women. The most used classes of medication were antianemic (88.9%) and analgesics (63.2%) (Table 3).
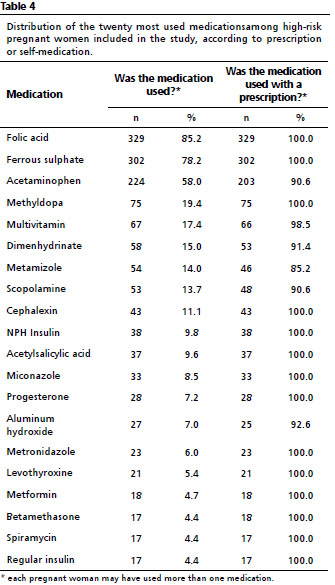
Among the medication most mentioned by pregnant women, folic acid, ferrous sulfate and acetaminophen stand out (Table 4).
According to the risk classification for medication use in pregnancy proposed by the FDA, most medications consumed by the interviewees are in categories C (35%, n=54) and B (25%, n=40), followed by medication drug categories D (11.3%, n=18), A (2.5%, n=4) and X (1.2%, n=2). As they are not approved for use in the United States, 17.5% (n=28) of the medications used are not included in the classification. Additionally, for 7.5% (n=12) of the medications, the risk category could not be identified, since the pregnant woman did not remember the name, referring to it only as “gynecological ointment”, a “throat tablet”, among others.
It is also worth noting that 86.3 % (n=333), 79.8% (n=308), and 66.8% (n=258) of the pregnant women used at least one drug in categories A, C, and B, respectively. Medications in categories D and X were less used, being consumed by 17.1% (n=66) and 0.8% (n=3) of women, respectively.
Only 36.5% of pregnant women (n=141) were considered adherent to the pharmacological treatment prescribed by the physician, 32.9% (n=127) declared they were unaware of the indication of the medication they used and 42% (n=162) did not receive guidance on the use of medications during pregnancy.
After applying the Logistic Regression Model, adjusted by the clinic where the pregnant woman was seen, there was no evidence of an association between the number of medications used by pregnant women and the clinical and sociodemographic aspects (χ² Wald=6.271;
p=0.180; R²=0.53) (Table 5).
DiscussionDespite the high prevalence of medication use among the participants, only 36% of the pregnant women were considered adherent to pharmacological treatment. The class antianemics, of which benefits and indications during pregnancy are already known
2, was the most mentioned class, which may be an indicator of regular prenatal care. However, the low adherence to pharmacological treatment is concerning, since in high-risk pregnancies, pharmacological therapy, when properly prescribed considering the risks and benefits, is important for maintaining the health of the mother and fetus. Self-medication reported by 12.7 % of pregnant women is also alarming, since many drugs have teratogenic effects and are contraindicated, because they put the pregnancy at risk.
2The insertion of females in the job market and the development of new reproductive techniques promoted the expansion of women’s reproductive age and the increase in the number of primiparous women with advanced age. Studies reveal a worldwide trend towards an increase in the frequency of pregnancies in older women, to the detriment of a decrease in pregnancies in women under 20 years.
2 This trend was observed in this study, which found a lower prevalence of younger pregnant women (28.2%). However, it must be considered that this may be related to the inclusion bias of high-risk pregnant women, who are often older. The study population consisted of a majority of women with partners, predominantly white, with low income, economically dependent on their partners and dependent exclusively on the SUS for assistance.
Most pregnancies were not planned (61.9%), which may have an impact on pregnancy risk, since preconception preparation is important for the development of a healthy pregnancy and impacts maternal and child morbidity and mortality rates.
11 In addition, women who are unaware of their pregnancy are more likely to use medicationthat are potentially harmful to the embryo/fetus. The risk is even greater when we consider that a relevant portion of the pregnant women had a history of previous abortion (29.3%). On the other hand, most women were in the first trimester of pregnancy when they confirmed pregnancy (88.6%), and even during this period, started prenatal care (86.8%), which is considered ideal.
12 The average number of prenatal and ultrasound consultations performed by pregnant women is also in line with the recommendation from SUS.
13Various initiatives in the area of healthcare are being carried out in Brazil with the aim of expanding access and improving the quality of prenatal care. In 2011, the
Rede Cegonha (Stork Net) was launched by the Ministry of Health, a government strategy that aims to implement care focused on reproductive planning, qualified childbirth, humanized care during pregnancy and puerperium, and safe childbirth and healthy child development.
12 The evaluation of the results of
Rede Cegonha points to a significant increase in the number of women with access to appropriate technology for childbirth and a reduction in practices considered harmful.
13 The early initiation and regularity of assistance provided to pregnant women participating in this study may suggest improvements in access to health services, greater awareness of the importance of prenatal care, as well as indicating the knowledge pregnant women have regarding potential risk factors for the fetus, which determines how quickly they seek for the health service.
In contrast, the fact that some interviewees came from other regions and States, suggests that in some locations there is still a certain vulnerability in access to women’s healthcare and in the mechanisms of integration in the healthcare network. In addition, although the reference hospital units for high-risk pregnancies must have a multidisciplinary team to assist pregnant women, women who have recently given birth, and newborns,
14 only 24.9% of the interviewees reported going to follow-up appointments with physicians of another specialty (besides the gynecologist) and only 24.4% reported seeing other health professionals. It is worth mentioning that the integration of different knowledge, a proposal of interprofessional work, assumes that a professional alone cannot address all dimensions of care. Encouraging teamwork is essential to promote the integrality and resoluteness of actions and to offer better quality services to women, their companions, and newborns.
4,8,13Regarding diagnoses, hypertension, diabetes mellitus, susceptibility to toxoplasmosis, obesity, and infections were the most prevalent, similarly to what was observed in other Brazilian studies.
15,16 It is known that these diagnoses are contributing factors for complications during pregnancy, since they worsen maternal and child prognosis.
15,16Regarding the use of medications by pregnant women, the pharmacological responses may differ from those predicted due to pharmacokinetic and pharmacodynamic changes in the mother and fetus. The difference in intensity and duration of the effect of some medications during pregnancy is noticeable, due to the physiological status of the pregnant woman: slowing of gastric emptying, decreased intestinal motility, increased blood volume and cardiac output, relative reduction of plasma proteins, potential increase hepatic metabolism, increased renal perfusion, glomerular filtration, and dieresis.
17In relation to the fetus, the placenta was seen for many years as a physiological barrier that protected it from any pharmacological action, however it is now known that especially from the third embryonic week, many medications are able to cross the placental barrier and reach the blood circulation of the fetus which, due to not having all the organs fully developed (incomplete clearance) and due to the different distribution, is more subject to the negative effects of xenobiotics
3. Exposure can cause lethal damage (abortion); morphological, biochemical, physiological or behavioral damage (teratogenicity); or other damage of different natures, with immediate or late onset.
17,18Consequently, the prescriber must be careful when choosing pharmacotherapy for pregnant women, by prioritizing the non-pharmacological approach. Self-medication should also be discouraged. However, numerous times and especially in high-risk pregnancies, the use of medications is essential for the management of symptoms, of pre-existing health problems, or health problems acquired during pregnancy and/or even to treat diseases or malformations in the fetus.
17Almost all pregnant women participating in this study reported having used at least one medication during pregnancy until the time of the interview. This prevalence is similar to that reported in other Brazilian studies and even in worldwide studies.
3,19-21 However, this number should consider the influence of medications/supplements that are part of prenatal care and are recommended in protocols of the World Health Organization (WHO) and the Ministry of Health, such as folic acid and ferrous sulfate.
12 The class of antianemics was precisely that most mentioned by pregnant women, with ferrous sulfate being used by 85.2% and folic acid by 78.2 % of women.
The physiological need and the benefit of using antianemics during pregnancy are known, given that the pregnant woman has a deficit of folic acid and an approximately three times greater loss of iron. Thus, supplementation is recommended as part of prenatal care to reduce the risk of low birth weight and congenital malformations of the neural tube, in addition to iron deficiency and megaloblastic anemia in pregnant women.
17,22Supplementation with vitamins and multivitamins is also widely used during pregnancy and 16.8% of the interviewees used vitamins, most of which (98.5%) under medical prescription. It is known that the necessary amounts of vitamins and minerals during pregnancy are increased to supply fetal growth, metabolism, and maternal and placenta tissue development.
22 As most women of reproductive age do not take the recommended amounts of vitamins and minerals, many professionals resort to the prescription of supplements to remedy pre-existing nutritional deficiency that can be aggravated by the physiological changes resulting from pregnancy.
23Considering the different compositions of multivitamins and minerals available on the market, it is important that the prescriber and the pharmacist are attentive to providing the adequate amount of nutrients, without exceeding the recommended daily intake. Some excess nutrients during the first weeks of pregnancy such as vitamin A, may have a teratogenic effect.
23The high frequency of use of at least one drug during pregnancy can be considered an indicator of regular prenatal care. However, the average number of medications used per woman and the variability of medications should be analyzed with more caution. Self-medication, reported by 12.7% (n=49) of pregnant women is also of concern, despite the value being low compared to other studies with high-risk pregnant women conducted in Brazil, in which the prevalence was around 30%.
24,25Analgesics were used with or without prescription by most pregnant women (63.2 %), which is justified by the positional, pelvic, and musculoskeletal pain of pregnancy. Due to its relative safety, acetaminophen is the first line in the treatment of pain and fever throughout the gestational period, which is reflected in the high prevalence of use found in this study (58 %). Some studies demonstrate an association between uterine exposure to acetaminophen and prevalence of childhood asthma, attention deficit hyperactivity disorder, hyperkinetic disorders, and neurological impairments.
17 However, there is no conclusive evidence and acetaminophen continues to be considered a safe medication in pregnancy.
Metamizole, in turn, despite not having its use approved by the FDA due to the association with agranulocytosis, is widely used by pregnant women in Brazil. In this study, 14% of pregnant women used metamizole and 85.2% of these under prescription, suggesting prescribers’ confidence in the safety of the medication. A Brazilian study pointed out that the use of metamizole during pregnancy was a risk factor for the development of leukemia in children under two years of age in 13 state capitals.
26 Therefore, it is important to exercise caution when prescribing this medication to pregnant women and self-medication should be discouraged.
Although it was not a prevalent situation, it is important to highlight the presence of ten reports of the use of non-steroidal anti-inflammatory drugs (NSAIDs), seven of them with a medical prescription. Inhibition of prostaglandin synthesis associated with this pharmacological class has frequently caused premature closure of the fetal artery duct in the third trimester of pregnancy, which can cause pulmonary arterial hypertension in the newborn. In addition, the reduction of prostaglandins can also cause renal dysfunction in the fetus, inhibition of platelet aggregation in the mother and fetus, and prolongation of labor. Thus, the use of NSAIDs, especially in the third trimester, is strongly discouraged.
24During pregnancy, some factors favor the occurrence of infections by fungi, bacteria, and protozoa, especially in the urinary tract, such as: changes in bacterial flora, pH, and vaginal humidity, drop in immunity, hormonal changes, mechanical compression of the uterus, and dilatation of the renal pelvis and ureters. Treatment with antimicrobials is essential as infections are associated with higher rates of preterm birth, abortion and maternal and neonatal morbidity and mortality.
27 Such facts justify the high prevalence found of the use of systemic antibacterial (26.7%) and anti-infectious and gynecological antiseptics (17.4%). Considering that 4.4% of pregnant women declared only the use of “gynecological ointment” without reporting its components, which may contain such drugs in their composition, consumption may have been even higher.
Cephalexin (11.1%) was the most widely used antibiotic, with an indication for urinary tract infections (UTI). Cephalosporins are safe and well tolerated during pregnancy, with cephalexin being the most indicated. Nitrofurantoin and ampicillins can also be used, however fluoroquinolones, often prescribed for UTI outside pregnancy, are not recommended as there is a possible association with renal toxicity, heart defects, and central nervous system toxicity in the fetus. Spiramycin was also used by pregnant women in the study (4.4%), being the treatment of choice for the prevention of vertical transmission of toxoplasmosis.
17,27 Miconazole (8.5 %) and metronidazole (6%) were among the most used gynecological anti-infectives and antiseptics. In addition to the safety of the antimicrobial classes, it should also be considered that the increase in the glomerular filtration rate, volume, and cardiac output during pregnancy can lead to pharmacokinetic changes in antibiotics, which require dose adjustment or careful monitoring and evaluation.
27Medication used during pregnancy to relieve common symptoms of the period, such as nausea, vomiting, dizziness, heartburn, abdominal pain, colic, flatulence, and intestinal constipation, were also present among the most used (drug for gastrointestinal disorders, antihistamines for systemic use, and drug for acidity-related disorders). However, these symptoms should be managed preferably with non-pharmacological measures: elevation of the head of the bed; fractional meals; reduced intake of acidic, spicy and fatty foods; wearing comfortable shoes and clothes; proper posture; moderate exercise; acupuncture; among others.
17Heartburn and gastroesophageal reflux are common symptoms especially in the third trimester of pregnancy and can be minimized with the use of H2 receptor antagonists, proton pump inhibitors, and antacids, which explains the presence of aluminum hydroxide (7%) among the most used medication.
17,28 Dimenhydrinate (15%) is useful in controlling nausea and vomiting in early pregnancy, with or without pyridoxine (vitamin B6). Scopolamine (13.7%) was also present among the most used, possibly for the management of nausea and colic in early pregnancy or in associations with analgesics. These medications are considered safe in pregnancy, except for scopolamine, which should be avoided due to the absence of studies that prove its safety.
28It is important to highlight that some of the medications most used by pregnant women in this study, such as methyldopa, NPH and regular insulins, acetylsalicylic acid, progesterone, levothyroxine, metformin and betamethasone, unlike the medications previously mentioned, are not regularly used in pregnancy. However, they are commonly used to treat conditions that determine high-risk pregnancies, such as arterial hypertension, gestational diabetes mellitus, hypothyroidism, risk of premature birth, and among others.
Alarming data obtained in the study is the high frequency of use of medications in categories C, D or X, according to the FDA. However, it is important to note that the FDA has been proposing changes in this risk categorization system, considering it simplistic. The ideal approach would also be to consider the dose, the duration of the exposure, the route of administration, and the embryonic age at the time of exposure, in addition to the genetic susceptibility and other individual characteristics of the woman.
28,29 In the update published in 2014, the letters were deleted and it was suggested that the prescriber consider the available data on the medications, the characteristics of the pregnant woman, the real need to employ pharmacotherapy, and weigh the risk versus the benefit to decide on the use.
17Any risk classification of drugs in pregnancy is incomplete, since it is impracticable to control all conditions of exposure, health status, and family history of the pregnant woman and concomitant exposures. Thus, the classification proposed in this work using the letter system is still widely used in scientific circles, especially in pharmacoepidemiology.
17,29Despite the risk associated with the use of medications during pregnancy, the benefit of pharmacological therapy in high-risk pregnant women for maintaining the health of the mother and fetus is undeniable. In this sense, adherence to the treatment prescribed by the physician is essential and the low adherence obtained in the present study is alarming. The pregnant woman should be guided by the multidisciplinary team so that she has the perception that the benefits of the prescribed pharmacotherapy outweigh the risks, empowering her regarding her health condition and favoring treatment adherence. Aspects such as drug access, cultural interferences, treatment complexity, forgetfulness, and confusion with dosing regimens can also impact on low adherence and must be addressed. The finding that a significant percentage of pregnant women did not know the reason for physician indication of medication use and did not receive guidance on them reinforces the educational role of the health team in promoting adherence.
30Some studies of medication use by pregnant women report an association between sociodemographic and clinical variables with the number of medications used. There are reports that women with a higher education level, non-primiparous or with a higher number of prenatal consultations, use more medications during pregnancy.
3 The fact that no association was found in this study may be related to the population, which has more serious health conditions when compared to low-risk pregnant women. Such conditions can determine a greater need for medications, and in a way decrease the influence of socioeconomic, demographic, and gestational characteristics on the use of medications.
A limitation of the study is the recall bias inherent in collecting data from a period prior to the interview; in addition, other medications may have been used after the interviews, factors that may have contributed to underestimate the number of medications mentioned.
This work was able to describe the pharmaco-epidemiological profile of high-risk pregnant women, which can contribute to the development of strategies related to improving the care of this population, as well as to the rational use of medications. A relevant strategy is to strengthen the performance of the multi-professional team, since physiotherapists, occupational therapists, psychologists, pharmacists, and nutritionists can contribute greatly to the pharmacological and non-pharmacological management of symptoms and health problems during pregnancy, in addition to favoring treatment adherence. It should be noted that the pharmacist can still assist prescribers in the management of pharmacotherapy, considering safety, pharmacokinetic, and pharmacodynamic variations, and the clinical and sociodemographic variables of pregnant women.
References1. Sampaio AFS, Rocha MJF, Leal EAS. High-risk pregnancy: Clinical-epidemiological profile of pregnant women attended at the prenatal service of the public maternity hospital of Rio Branco, Acre. Rev Bras Saúde Matern Infant. 2018; 18 (3): 55-66.
2.Ministério da Saúde (BR). Gestação de alto risco: manual técnico. 5
th ed. Brasília (DF): Ministério da Saúde; 2012 [access in 2020 ago 18]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/manual_tecnico_gestacao_alto_risco.pdp3. Costa DB, Coelho HLL, Santos DB. Utilização de medicamentos antes e durante a gestação: Prevalência e fatores associados. Cad Saúde Pública. 2017; 33 (2): e00126215.
4. Storpirtis S, Mori ALPM, Yochiy A, Ribeiro E, Porta V. Farmácia Clínica e Atenção Farmacêutica. 1
st ed. Rio de Janeiro: Guanabara Koogan; 2008.
5.Medronho RA, Bloch KV, Luiz RR, Werneck GL. Epidemiologia. São Paulo: Atheneu; 2009.
6. World Health Organization (WHO). ATC/DDD: international language for drug utilization research. Noruega: WHO; [access in 2020 ago 20]. Available from:
http://www.whocc.no7. United States Food And Drug Administration. Labeling and prescription drug advertising: content and format for labeling for human prescription drugs. Fed Regist. 1979; 44: 37434-67.
8. Case Management Society of America (CMAG). Case management adherence guidelines: guidelines from the Case Management Society of America for improving patient adherence to medication therapies. Version 2.0; 2006; [access in 2022 ago 5]. Available from:
https://www.miccsi.org/wp-content/uploads/2016/01/CMAG2.pdf9.Leite SN, Vasconcellos MPC. Adesão à terapêutica medicamentosa: elementos para a discussão de conceitos e pressupostos adotados na literatura. Ciên Saúde Coletiva. 2003; 8 (3): 772-85.
10. Nascimento RCRM, Álvares J, Guerra Junior AA, Gomes IC, Silveira MR, Costa EA,
et al. Polifarmácia: uma realidade na atenção primária do Sistema Único de Saúde. Rev Saúde Pública. 2017; 51 (Suppl. 2): 1-12.
11. Borges ALV, Santos OA, Nascimento NC, Chofakian CBN, Gomes-Sponholz FA. Preconception health behaviors associated with pregnancy planning status among Brazilian women. Rev Esc Enferm. 2016; 50 (2): 208-15.
12. Ministério da Saúde (BR). Portaria n
o 1.459, de 24 de junho de 2011. Institui, no âmbito do Sistema Único de Saúde - SUS - a Rede Cegonha. Brasilia (DF): DOU 27 de junho 2011. [access in 2020 set 20]. Available from:
https://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011.html13. Leal MC, Bittencourt SA, Esteves-Pereira AP, Ayres BVS, Silva LBRAA, Thomaz EBAF,
et al.Avanços na assistência ao parto no Brasil: resultados preliminares de dois estudos avaliativos. Cad Saúde Pública. 2019; 35 (7): e00223018.
14. Ministério da Saúde (BR). Portaria n
o 1.020, de 29 de maio de 2013. Institui as diretrizes para a organização da Atenção à Saúde na Gestação de Alto Risco e define os critérios para a implantação e habilitação dos serviços de referência à Atenção à Saúde na Gestação de Alto Risco, incluída a Casa de Gestante, Bebê e Puérpera (CGBP), em conformidade com a Rede Cegonha. Brasilia (DF): DOU 31 de maio de 2013. [access in 2020 set 2]. Available from:
https://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt1020_29_05_2013.html15. Leite FMC, Amorim MHC, Nunes GF, Soares MFS, Sabino NQ. Perfil sociodemográfico e obstétrico de puérperas internadas em uma maternidade de alto risco no município da Serra, ES. Rev Bras Pesq Saúde. 2009; 11 (1): 22-6.
16. Buchabqui JA, Capp E, Ferreira J. Adequação dos encaminhamentos de gestações de alto-risco na Rede Básica de Atenção à Saúde de Porto Alegre, Rio Grande do Sul, Brasil. Rev Bras Saúde Matern Infant. 2006; 6 (1): 23-9.
17. Fuchs FD, Wannmacher L. Farmacologia Clínica e Terapêutica. 5
th ed. Rio de Janeiro: Guanabara Koogan; 2017.
18. Nakamura MU, Kulay-Junior L, Pasquale M. Uso de fármacos na gravidez: benefício e custo . Rev Bras Ginecol Obstet. 2008; 30 (1): 1-4.
19. Rocha RS, Bezerra SC, Lima JWO, Costa FS. Consumo de medicamentos, álcool e fumo na gestação e avaliação dos riscos teratogênicos. Rev Gaúcha Enferm. 2013; 34 (2): 37-45.
20. Demailly R, Escolano S, Quantin C, Tubert-Bitter P, Ahmed I. Prescription drug use during pregnancy in France: a study from the national health insurance permanent sample. Pharmacoepidemiol Drug Saf. 2017 Sep; 26 (9): 1126-34.
21. Daw JR, Hanley GE, Greyson DL, Morgan SG. Prescription drug use during pregnancy in developed countries: a systematic review. Pharmacoepidemiol Drug Saf. 2011 Sep; 20 (9):895-902.
22. World Health Organization (WHO). WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO; 2016. [access in 2020 set 2]. Available from:
https://www.who.int/publications/i/item/978924154991223. Hovdenak N, Haram K. Influence of mineral and vitamin supplements on pregnancy outcome. Eur J Obst Gynecol Reprod Biol
. 2012; 164 (2): 127-32.
24. Santos SLF, Pessoa CV, Arraes MLBM, Barros KBNT. Automedicação em Gestantes de Alto Risco: Foco em Atenção Farmacêutica. Rev Med UFC. 2018; 58 (3): 36-43.
25. Araújo DD, Leal MM, Santos EJV, Leal LB. Consumption of medicines in high-risk pregnancy: Evaluation of determinants related to the use of prescription drugs and self-medication. Braz J Pharm Sci. 2013 Sep; 49 (3): 491-9.
26. Couto AC, Ferreira JD, Pombo-De-Oliveira MS, Koifman S. Pregnancy, maternal exposure to analgesic medicines, and leukemia in Brazilian children below 2 years of age. Eur J Cancer Prev. 2015 May; 24 (3): 245-52.
27. Bookstaver PB, Bland CM, Griffin B, Stover KR, Eiland LS, McLaughlin M. A review of antibiotic use in pregnancy. Pharmacotherapy. 2015 Nov; 35 (11): 1052-62.
28. Briggs GG, Freeman RK, Towers CV, Forinash AB. Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. 11
th ed. United States: Wolters Kluwer Health; 2017.
29. United States Food And Drug Administration. Pregnancy and Lactation Labeling (Drugs) Final Rule. FDA [Internet]. [access in 2020 set 2]. Available from:
https://www.fda.gov/drugs/labeling-information-drug-products/pregnancy-and-lactation-labeling-drugs-final-rule30. Juch H, Lupattelli A, Ystrom E, Verheyen S, Nordeng H. Medication adherence among pregnant women with hypothyroidism-missed opportunities to improve reproductive health? A cross-sectional, web-based study. Patient Educ Couns. 2016 Oct; 99 (10): 1699-707.
Received on December 29, 2020
Final version presented on March 22, 2022
Approved on May 9, 2022
Authors’ contributionNagai MM is the researcher responsible for carrying out the project that originated this manuscript. Campos MSA and Ayres LR contributed to the data collection and statistical analysis. Zanetti MOB and Lemos CA contributed to the writing and submission of the manuscript. Duarte G and Pereira LRL oriented the project and assisted in the revision of the manuscript. All authors approved the final version of the article and declared that there was no conflict of interest.
 ; Maria Olívia Barboza Zanetti 2
; Maria Olívia Barboza Zanetti 2 ; Carla Assad Lemos 3
; Carla Assad Lemos 3 ; Marília Silveira de Almeida Campos 4
; Marília Silveira de Almeida Campos 4 ; Lorena Rocha Ayres 5
; Lorena Rocha Ayres 5 ; Geraldo Duarte 6
; Geraldo Duarte 6 ; Leonardo Régis Leira Pereira 7
; Leonardo Régis Leira Pereira 7