ABSTRACT
OBJECTIVES: to verify the quality indicators of neonatal hearing screening programs, identify the most prevalent risk factors for hearing loss and analyze access to the Hearing Health Care Network.
METHODS: cross-sectional study using secondary data. The population are children born in public maternity hospitals from 2015 to 2019. Data collection was carried out in the database of programs and hearing health service. The absolute and relative frequencies of all variables collected and the median, the interquartile range and the Mann-Whitney test were calculated to analyze the access.
RESULTS: universality increased during the study period, but was not reached (71.9%; CI95%=70.4-73.3) and the referral rate for auditory diagnosis was within the recommended range (0.9%; CI95%=0.8-0.9). The most prevalent risk factors were congenital infections and heredity. There was an evasion of children to the hearing health service of 85.1% and the type of referral interfered with the age of the child at access. Eight children with hearing loss were diagnosed, in which seven had access to therapeutic interventions.
CONCLUSIONS: hearing screening was not universal. Access to the Hearing Health Care Network presents high evasion and interventions were offered to children with hearing loss.
Keywords:
Health services accessibility, Child, Hearing loss, Neonatal screening
RESUMO
OBJETIVOS: verificar os indicadores de qualidade dos programas de triagem auditiva neonatal, identificar os fatores de risco para deficiência auditiva mais prevalentes e analisar o acesso à Rede de Atenção à Saúde auditiva.
MÉTODOS: estudo transversal com uso de dados secundários. A população são as crianças nascidas em maternidades públicas no período 2015 a 2019. A coleta de dados foi realizada no banco de dados dos programas e do serviço de saúde auditiva. Foram calculadas as frequências absolutas e relativas de todas as variáveis coletadas e a mediana, o intervalo interquartil e o teste de Mann-Whitney para analisar o acesso.
RESULTADOS: a universalidade aumentou no período estudado, porém não foi atingida (71,9%; IC95%=70,4-73,3) e o índice de encaminhamento para diagnóstico auditivo esteve dentro do recomendado (0,9%; IC95%=0,8-0,9). Os fatores de risco mais prevalentes foram: infecções congênitas e hereditariedade. Observou-se uma evasão de 85,1% das crianças ao serviço de saúde auditiva e o tipo de encaminhamento interferiu na idade da criança no acesso. Foram diagnosticadas oito crianças com perda auditiva, na qual sete tiveram acesso as intervenções terapêuticas.
CONCLUSÕES: A triagem auditiva não foi universal. O acesso à Rede de Atenção à Saúde auditiva apresenta uma alta evasão e as intervenções foram ofertadas às crianças com perda auditiva.
Palavras-chave:
Acesso aos serviços de saúde, Criança, Perda auditiva, Triagem neonatal
IntroductionHearing loss in childhood can cause delays in speech and language development, academic performance and negatively impact social and emotional aspects.
1 The World Health Organization considers hearing loss a public health problem and estimates that approximately 34 million children worldwide have this alteration.
2 Actions to prevent, identify and intervene into hearing loss are economical and capable of providing benefits to individuals.
1,2In Brazil, the Neonatal Hearing Screening (NHS) programs aim to identify and intervene early on children with hearing loss and must be integrated into the Care Network for Persons with Disabilities and maternal and child monitoring actions. In all live births, hearing screening should be performed in the maternity ward and those who have Risk Factor for Hearing Loss (RFHL) or who fail, should be referred for monitoring or diagnosis at the Hearing Health Services (HHS). After confirmation of hearing loss, the child should start monitoring with an otolaryngologist and/or hearing rehabilitation, which may include the use of electronic devices: PersonalSound Amplification Device (PSAD) and Cochlear Implant (CI), parallel to speech therapy.
3 Programs must evaluate and monitor actions related to hearing health, through quality indicators.
3,4The identification of RFHI is a very valuable information for professionals, as it determines the path to be undertaken with NHS and follow-up in the HHS.
3 The main risk factors for hearing loss are permanence in the Intensive Care Unit, use of ototoxic medication and congenital infections and are among the most prevalent in the Brazil.
5,6In the state of Rio Grande do Norte, the NHS implementation took place in 2007. In the municipal maternity hospitals in the capital, coverage was 80% and the prevalence of sensorineural hearing loss was 0.52 for every 1000 screened in the period from 2007 to 2009.
7 A more recent study found a weighted average of municipalities covered by the NHS of only 45.9% in 2017.
8Global hearing health indicates obstacles that impede to achieve the quality indicators for a good program, such as the distance from the residence to the service, the parents’ socioeconomic conditions and the evasion of families. The low supply of qualified professionals and specialized services interfere with access to hearing health services, directly impacting the intervention of children with hearing loss.
9-11 Therefore, the objective of this study was to verify the quality indicators of newborn hearing screening programs, identify the most prevalent risk factors for hearing loss and analyze access to the Hearing Health Care Network for children in the state of Rio Grande do Norte.
MethodsThis research is part of the study entitled “Evaluation of children’s hearing health policy in the state of Rio Grande do Norte” approved by the Research Ethics Committee of the Onofre Lopes University Hospital of the Federal University of Rio Grande do Norte under CAAE number 25214819.4.0000.5292 on April 29, 2020.
This is a cross-sectional study using secondary data. The study sample consisted of 37,180 children born in public maternity hospitals. The inclusion criteria were all children born in the maternity hospitals selected for the study from 2015 to 2019. There was no exclusion criterion.
The maternity hospitals selected were the two municipal public maternity hospitals located in Natal, capital, and a public maternity hospital located in Santa Cruz, a city 120 km from the capital, which were chosen because they referred to the same HHS in Natal and because they had pioneering programs in the state. The HHS is the SUVAG (Portuguese acronym for Guberina’s Universal Verbotonal Auditory System) center, which is a specialized hearing health care service and serves all age groups, with an emphasis on children.
The three programs used Transient Otoacoustic Emissions (TOE) as an assessment method, the speech therapists performed the screenings in the rooming-in and outpatient clinics and presented the same flow of care, in which the hearing screening was performed in two stages (test and retest) . It was considered “pass” when the child had the presence of otoacoustic emissions in both ears and “fail” when there was no presence of emissions in one or both ears tested. Whenever the test “failure” occurred, a retest was scheduled, which took place within a period of up to 30 days after the test. In case of failure in the retest, the child was referred for auditory diagnosis at the HHS. The child who had a RFHL
3,12,13 was also referred for hearing monitoring at the HHS. Auditory diagnosis consists of an assessment to identify hearing loss and auditory monitoring consists of periodic assessments to identify late and/or progressive hearing loss.
All children referred for monitoring and auditory diagnosis at the HHS were attended by four specialties: otorhinolaryngology, psychology, social services and speech therapy to carry out the auditory assessment, which is comprised of anamnesis, behavioral assessment (instrumental and audiometry with visual reinforcement), measures of acoustic immittance (tympanometry and acoustic reflex research) and TOE and Brainstem Auditory Evoked Potential (BAEP) and auditory steady state response. In cases of confirmed hearing loss, children were referred for intervention according to the classification of hearing loss and those with indication for surgical intervention with the Cochlear Implant were referred to another HHS in the network.
Data collection was carried out in January and February 2021 in two stages. In the first step, the following were extracted from the database of each program: the date of birth, date, result and conduct of the hearing screening, RFHL (yes or no and which ones) in the years 2018 and 2019 and attendance at the HHS (yes or not). In the second stage, in the HHS diagnostic sector bank, the following were extracted: age of the child at the first consultation, conclusion of the auditory evaluation (yes or no), result of the auditory evaluation (hearing loss or normal hearing) and for cases of confirmation of the Hearing loss classification, age at diagnosis, initiation of speech therapy (yes or no), hearing aid use (yes or no) and CI implantation (yes or no) and implant laterality (unilateral or bilateral).
The RFHL considered were altered apgar, arbovirus during pregnancy, craniofacial anomalies involving ear and temporal bone, severe perinatal anoxia, heredity, hyperbilirubinemia, congenital infections (toxoplasmosis, rubella, cytomegalovirus, herpes, syphilis and HIV), postnatal bacterial or viral infections (cytomegalovirus, herpes, measles, chickenpox and meningitis), small for gestational age, weight less than 1500g, prematurity, parental concern, syndrome that usually express hearing loss, use of ototoxic drugs, use of mechanical ventilation and stay in the Neonatal Intensive Care Unit (NICU) for more than 5 days.
3,12,13The universality quality indicator corresponds to the percentage of children screened in relation to the number of live births and it is recommended that this value be greater than or equal to 95%. The referral index for diagnosis indicator corresponds to the percentage of children referred for auditory diagnosis in relation to the number of children screened and the recommended value is less than 4%
.3Data were analyzed using the Statistic Package for Social Sciences (SPSS) software, version 20.0. First, the absolute and relative frequencies of all variables collected were calculated, followed by the 95% confidence intervals (CI95%) for the quality indicators. To analyze access to HHS, the median (Md) and interquartile range (IQR) of the variable age at first access were calculated, as well as the Mann-Whitney test to analyze whether the type of referral interfered with the child’s age at access. Finally, the characterization of the care trajectory of children with hearing loss based on therapeutic interventions was carried out.
ResultsDuring the study period, 37,180 children were born in the three maternity hospitals and 26,756 underwent NHS. It is observed that over the years the coverage increased and at the end it obtained an average of 71.9% (CI95%=70.4-73.3). The referral rate for diagnosis ranged from 0.6 to 1.4%, totaling 268 children and an average of 0.9% (CI95%=0.8-0.9). The two indicators in percentages are shown in Table 1.
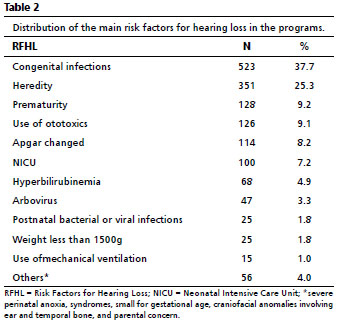
With regard to the presence of RFHL, 94.6% (n=25,372) of the children had no risk factors and 5.1% (n=1,384) had one or more risk factors. Each child with RFHL had, on average, 1.2 factors. Table 2 shows the frequencies and percentages of each of the 16 risk factors, the most prevalent being congenital infections and heredity.
Of the children referred to the HHS, there was a high dropout rate both in attendance, 1,217 (73.6%), and in the completion of the hearing assessment, 191 (11.5%), being lower in the cases of diagnosis. During auditory monitoring, a child with craniofacial anomaly involving the ear and temporal bone with hearing loss was identified, specifically cleft lip and palate, and was classified as conductive hearing loss of mild bilateral degree. As for the diagnosis, seven children were identified with profound bilateral sensorineural hearing loss. These findings are represented in Figure 1.
Children referred for auditory diagnosis were younger at first access (Md=2; IIQ= 3) than those referred for monitoring (Md=3; IIQ= 3), as shown in Figure 2. In addition, the Mann Whitney showed that the type of referral interferes with the age of access to the hearing health service (U=13508.00;
p<0.001).
Finally, the care trajectories of the eight children diagnosed with hearing loss were traced from the therapeutic interventions. The only child that was referred for auditory monitoring and presented hearing loss concluded the diagnosis at three months of age and did not return for the continuity of the intervention. The other seven performed the diagnosis after three months of age, four between three and six months, all started speech therapy in the HHS itself and were fitted with the hearing aid, then underwent bilateral CI surgery in the other HHS of the Network.
DiscussionEvaluation and monitoring of the results of the NHS program are fundamental for planning and executing health actions and analyzing access to the HHS makes it possible to infer how the Hearing Health Care Network is working. It can be seen that children with hearing loss obtained access to intervention, which is recommended by the hearing health policy. Nevertheless, the need for developing strategies to improve the adherence of families to the NHS program could be identified.
The universality indicator assesses the coverage of screened children and is based on federal law nº 12,303 of 2010.
14 The number of professionals and the supply of equipment available in the program directly impact on this indicator, which may explain the variability observed in the study. In Brazil, the evolution of coverage was accompanied by a slight increase in the supply of speech therapists and equipment to perform hearing screening in SUS in most federative units, and universality is still not a reality.
15 In the study by Mallmann
et al.
16 the coverage of neonatal hearing screening was 44.1% in 2013 in the Northeast region. One aspect that positively influences is the performance of hearing screening before hospital discharge.
1It is worth mentioning that the NHS is the first step in the line of care for people with disabilities. Failure to do so will have a negative impact on the child’s prognosis.
3,17 The expansion of neonatal screening and the reduction of existing inequalities can be achieved with investments in the quality of Primary Health and prenatal care.
16 The best-informed mothers have more positive attitudes in relation to the universal programs of NHS.
18The referral index indicator for diagnosis in all programs is within the recommended by NHS Guidelines
3 and in line with a Brazilian study.
5 This indicator is influenced by the hearing screening protocol used, the use of automatic ABR is recommended in cases of failure in the test with evoked otoacoustic emissions to reduce false negatives.
3 Adherence to the program also influences, as failure to attend the retest will result in a decrease in this indicator. Finally, the profile of the population served, the mapping of RFHLspecific to the enrolled population,
19 the more prevalent the RFHL, the more likely the NHS failure to occur.
The risk factors also reflect the diagnosis of the community in which the program is inserted.
19 The findings corroborate the literature. Congenital infections are among the most prevalent factors in Brazil,
5,6 with emphasis on syphilis, which is considered a public health problem and has been increasing in recent years.
20 As for heredity, this is also reported in the scientific community, however less frequent.
5,6 The most recent documents on this subject are the American recommendation
1 and the technical note of the Multiprofessional Committee on Hearing Health (MCHH),
21 which excluded prematurity, but there is still a program that considers it as a factor.
5 the importance of continuing education for health professionals.
Hearing monitoring provides the diagnosis of late and/or progressive hearing loss,
3 however a high evasion was observed both in the first consultation and at the conclusion of the hearing assessment. Dropout is a worldwide problem in NHS programs, and guidance to parents is essential, which needs to be adapted to the various educational, social, economic and health factors for greater effectiveness.
22 In monitoring, in addition to monthly follow-up of hearing development and of language in Primary Health Care, a hearing assessment is recommended when the child is between 7 and 12 months old
3 The median age of access to the HHS was much lower than that reported, 11.6 months,
23 and recommended in the hearing health policy, which can be justified by the hearing screening protocol of the programs, which use only transient evoked otoacoustic emissions (TEOAE), in which immediate referral to the HHS allows children access to the BAEP test.
Audiological diagnosis is the next phase of the NHS programs, being extremely important, as it allows the identification of hearing loss and intervention.
1,3Evasion in this phase demonstrates a rupture in the continuity of care and reflects the obstacles of the Network of Care for People with Disabilities, which are the waiting lists for health services, flaws in the regulatory system, the low supply of care and specialist professionals such as speech therapists and the concentration of services in more urban areas.
9,24-26 The HHS does not have an active search program for the completion of the hearing assessment, which could help the early diagnosis of hearing loss and enable the child to remain in the Health Care Network, being valid for cases of diagnosis and monitoring auditory.
On the other hand, access to therapeutic interventions for children with hearing loss demonstrate the guarantee of full access. The Care Network for People with Disabilities integrates different units and levels of hearing health care. NHS, diagnosis and rehabilitation are part of a continuous and inseparable process, in order to reach the expected outcome in children with permanent hearing loss. The use of electronic devices, which include hearing aids and CI, and attendance atspeech therapy are regulated in SUS public policies.
3 Children implanted bilaterally present the best performances in speech perception compared to the adaptation of bilateral hearing aids (HA) and bimodal adaptation (HA and CI).
27 The offer of the service that makes the CI device available represents a potential of the Health Care Network.
Access to the Child Hearing Health Care Network presents obstacles with an evasion above expectations and children with late ages in the stages of diagnosis and intervention in developing countries,
4,6,28 in addition, in Brazil, there are regional differences regarding the offer of services and specialized professionals, directly impacting access.
8,15,16,24 On the other hand, developed countries have better indicators regarding access to hearing health services,
4 such as the United States, which has universal coverage of screening and ages of diagnosis and intervention of around 2 and 3 months, respectively.
29In the present study, the organization of the Hearing Health Care Network can be observed in the universality indicator and in the regulation of children for specialized care. Even in a single Brazilian state, these results provide theoretical insights for decision-making processes and future research.
The limitations of the study are related to lack of data in the databases on socioeconomic factors of families and on the trajectory of all children in the HHS, in addition, some children may have accessed the other HHS or the supplementary health system, but it was not possible to enter the other HHS in the study, because it did not have a database. Studies to evaluate health services and the system of regulated access to health care are suggested, as these directly impact the results of NHS programs.
The universality quality indicator in the three programs was not achieved; the index of referral for diagnosis was always within the recommended by the hearing health policy. Regarding access to hearing health services, there was an evasion, which was greater for children who were referred for hearing monitoring. Thus, the NHS allowed the capture of children with hearing loss and their insertion in the Health Care Network.
This study provided the visualization of implementation of the Hearing Health Care Network in the state of Rio Grande do Norte, through identification of organizational arrangements in the line of care with the offer of NHS in maternity hospitals and diagnosis and intervention in hearing health services.
References1. Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J Early Hearing Detect Interv. 2019; 4 (2): 1-44.
2. World Health Organization (WHO). Deafness and hearing loss.[Internet] [access in 2020 jul 8]. Available from:
https://www.who.int/health-topics/hearing-loss#tab=tab_23. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Diretrizes de Atenção da Triagem Auditiva Neonatal. Brasília (DF): Ministério da Saúde; 2012. [access in 2020 jul 8]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_atencao_triagem_auditiva_neonatal.pdf4. World Health Organization (WHO). Ear and hearing care: indicators for monitoring provision of services. Geneva: WHO; 2019. [access in 2020 jul 8]. Available from:
https://www.who.int/publications/i/item/ear-and-hearing-care-indicators-for-monitoring-provision-of-services5. Marinho ACA, Pereira, ECS, Torres, KCM, Andreza M, Ledesma ALL. Avaliação de um programa de triagem auditiva neonatal. Rev Saúde Pública. 2020; 54: 1-9.
6. Fichino SF. Avaliação da qualidade do programa saúde auditiva neonatal do município de São Paulo [tese]. São Paulo: Pontifícia Universidade Católica de São Paulo; 2021.
7. Cavalcanti HG. Prevalência das alterações audiológicas e fatores associados em recém-nascidos nas maternidades municipais de Natal- RN [tese]. Natal: Centro de Ciências da Saúde da Universidade Federal do Rio Grande do Norte; 2013.
8. Dias WCFGS, Paschoal MR, Cavalcanti HG. Análise da cobertura da triagem auditiva neonatal no Nordeste brasileiro. Audiol Commun Res. 2017; 22: 1-7.
9. Meyer AC, Marsolek M, Brown N, Coverstone K. Delayed identification of infants who are deaf or hard of hearing Minnesota, 2012-2016. Morb Mortal Wkly Rep. 2020 Mar; 69: 303-6.
10. Barr M, Duncan J, Dally K. A systematic review of services to DHH children in rural and remote regions. J Deaf Stud Deaf Educ. 2018 Abr; 23 (2): 118-30.
11. Maciel FJ, Friche AAL, Januário GC, Santos MFN, Reis RA, Neto RO, et al. Análise espacial da atenção especializada na Rede de Cuidados à Pessoa com Deficiência: o caso de Minas Gerais. CoDAS. 2020; 32 (3): 1-7.
12. Lewis DR, Marone SAM, Mendes BCA, Cruz OLM, Nobrega M. Comitê multiprofissional em saúde auditiva: COMUSA. Braz J Otorhinolaryngol. 2010 Fev; 76 (1): 121-8.
13. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Protocolo de atenção à saúde e resposta à ocorrência de microcefalia relacionada à infecção pelo vírus Zika. Brasília (DF): Ministério da Saúde; 2015. [access in 2020 jul 8]. Available from:
https://www.sbp.com.br/fileadmin/user_upload/2015/12/PROTOCOLO-SAS-MICROCEFALIA-ZIKA-dez-15.pdf14. Presidência da República (BR). Casa Civil. Subchefia para Assuntos Jurídicos. Lei nº 12.303, de 2 de agosto de 2010. Dispõe sobre a obrigatoriedade de realização do exame denominado Emissões Otoacústicas Evocadas. Brasília (DF): DOU de 3 de agosto de 2010. [access in 2020 jul 8]. Available from:
https://www.planalto.gov.br/ccivil_03/_ato2007-2010/2010/lei/l12303.htm15. Oliveira TS, Dutra MRP, Cavalcanti HG. Triagem Auditiva Neonatal: associação entre a cobertura, oferta de fonoaudiólogos e equipamentos no Brasil. CoDAS. 2021; 33 (2): 1-8.
16. Mallmann MB, Tomasi YT, Boing AF. Neonatal screening teste in Brazil: prevalence rates and regional and socioeconomic inequalities. J Pediatr (Rio J). 2020; 96 (4): 487-94.
17. Gabriel MM, Geyer L, McHugh C, Thapa J, Glynn F, Wasshe P, et al. Impact of Universal Newborn Hearing Screening on cochlear implanted children in Ireland. Int J Pediatr Otorhinolaryngol. 2020 Jun; 133: 109975.
18. Lam MYY, Wong ECM, Law CW, Lee HHL, McPherson B. Maternal knowledge and attitudes to universal newborn hearing screening: Reviewing an established program. Int J Pediatr Otorhinolaryngol. 2018 Feb; 105: 146-53.
19. Pimentel MCR, Figueiredo N, Lima, MLLT. Validação de uma matriz de indicadores para avaliação do Programa de Triagem Auditiva Neonatal. Rev CEFAC. 2020; 22 (6): e9420.
20. Ministério da Saúde (BR). Secretário de Vigilância em Saúde. Boletim Epidemiológico: Sífilis 2019. Brasília (DF): Ministério da Saúde; Outubro de 2019. [access in 2020 jul 8]. Available from:
http://www.aids.gov.br/pt-br/pub/2019/boletim-epidemiologico-sifilis-201921. Nota Técnica - Comitê Multiprofissional em Saúde Auditiva – COMUSA. Triagem Auditiva Neonatal Universal em tempos de pandemia. [access in 2020 jul 8]. Available from:
https://www.sbfa.org.br/portal2017/pdf/cvd19-nota-tecnica-comusa.pdf22. Qirjazi B, Toçi E, Tushe E, Burazeri G, Roshi E. Mothers’ perceptions of universal newborn hearing screening in transitional. PLoS One. 2020 Aug; 15 (8): e0237815.
23. Carneiro CS, Pereira MCCS, Lago MRR. Monitoramento audiológico em bebês com indicadores de risco para deficiência auditiva. Disturb Comum. 2016; 28 (3): 512-22.
24. Rech RS, Bulgarelli PT, Condessa AM, Santos CM, Hilgert JB, Goulart BNG. Acesso e uso de serviços de fonoaudiologia em Porto Alegre, Brasil: estudo populacional. Ciên Saúde Coletiva. 2020; 25 (3): 817-25.
25. Neves ET, Okido ACC, Buboltz FL, Santos RP, Lima RAG. Acesso de crianças com necessidades especiais de saúde à rede de atenção. Rev Bras Enferm. 2019; 72 (3): 65-71.
26. Silva VA, Busnello ARR, Cavassin RC, Loureiro APC, Moser ADL, Carvalho DR. Acesso à fisioterapia de crianças e adolescentes com deficiência física em instituições públicas. Ciênc Saúde Coletiva. 2020; 25 (7): 2859-70.
27. Chang Y-S, Hong SH, Kim EY, Choi JE, Chung W-H, Cho Y-S, et al. Benefit and predictive factors for speech perception outcomes in pediatric bilateral cochlear implant recipients. Braz J Otorhinolaryngol. 2019; 85 (5): 571-7
28. Fichino SN, Avelino VLF, Lewis DR. Características demográficas e audiológicas da população pediátrica de um centro de referência em saúde auditiva de São Paulo. Disturb Comun. 2018; 30 (3): 570-84.
29. Stewart JE, Bentley JE. Hearing loss in pediatrics: what the medical home needs to know. Pediatr Clin North Am. 2019 Abr; 66 (2): 425-36.
Received on November 2, 2021
Final version presented on April 14, 2022
Approved on April 25, 2022
Authors’ contributionDutra MRP performed data collection, project execution, manuscript preparation and review. Cavalcanti HG performed and reviewed the manuscript. Ferreira MAF supervised the project, drafted and revised the manuscript. All authors approved the final version of the article and declared no conflict of interest.
 ; Hannalice Gottschalck Cavalcanti 2
; Hannalice Gottschalck Cavalcanti 2 ; Maria Ângela Fernandes Ferreira 3
; Maria Ângela Fernandes Ferreira 3