ABSTRACT
OBJECTIVES: to evaluate the temporal trend of hospitalizations for pelvic inflammatory disease in Brazil and its regions between 2000 and 2019.
METHODS: longitudinal ecological study with data from the Hospital Information System. The analysis of temporal trends in hospitalization rates by age group was performed using segmented linear regression (joinpoint regression). Both annual percent change total and by age groups were estimated for Brazil and each region.
RESULTS: Brazil had an average reduction of 5.2% per year in the period and the age groups most affected were 20 to 29 and 30 to 39 years. North region had the highest rates and South and Southeast regions, the lowest. Midwest region had the largest annual average reduction (8.1%), followed by the Northeast (5.7%), Southeast (5.0%), North (4.6%) and South (4.3 %). The only age group that showed a significant increase was that of 10 to 19 years in the Southeast in the period from 2008 to 2019 (0.9%) and in the Northeast in the period from 2014 to 2019 (3.3%).
CONCLUSIONS: hospitalization due to pelvic inflammatory disease has significantly decreased in Brazil. The increase observed for adolescents in the Southeast and Northeast in the most recent period points to problems in the prevention and control of sexually transmitted infections in this age group.
Keywords:
Pelvic inflammatory disease, Time series studies, Hospitalization
RESUMO
OBJETIVOS: avaliar a tendência temporal de internações por doença inflamatória pélvica no Brasil e regiões entre 2000 e 2019.
MÉTODOS: estudo ecológico longitudinal com dados do Sistema de Informações Hospitalares. A análise das tendências temporais das taxas de internação hospitalar por faixas etárias foi feita por regressão linear segmentada (joinpoint regression). Foram estimadas variações percentuais anuais gerais e por faixas etárias para o Brasil e cada região.
RESULTADOS: o Brasil teve uma redução média de 5,2% ao ano no período e as faixas etárias mais afetadas foram 20 a 29 e 30 a 39 anos. A região Norte apresentou as maiores taxas e as regiões Sul e Sudeste as menores. A região Centro-Oeste teve a maior redução média anual (8,1%), seguida das regiões Nordeste (5,7%), Sudeste (5,0%), Norte (4,6%) e Sul (4,3%). A única faixa etária que apresentou um aumento significativo foi a de 10 a 19 anos nas regiões Sudeste no período de 2008 a 2019 (0,9%) e no Nordeste no período de 2014 a 2019 (3,3%).
CONCLUSÕES: a internação hospitalar por doença inflamatória pélvica reduziu no Brasil de forma importante. O aumento verificado para adolescentes no Sudeste e Nordeste no período mais recente aponta para problemas na prevenção e controle das infecções sexualmente transmissíveis nesta faixa etária.
Palavras-chave:
Doença inflamatória pélvica, Estudos de séries temporais, Hospitalização
IntroductionPelvic inflammatory disease (PID) consists in an infection of the female upper genital tract due to the rise of microorganisms, which can result in endometritis, salpingitis, oophoritis, tubo-ovarian abscess and pelviperitonitis. The most frequently associated pathogens are
Chlamydia trachomatis (10.0%) and
Neisseria gonorrhoeae (43.6%).
1According to World Health Organization (WHO), 131 million new cases of
Chlamydia trachomatis e 78 million of
Neisseria gonorrhoeae occur each year, worldwide.
2In 2012, the estimated global prevalence of infection by
Chlamydia trachomatis was 4.2% and by
Neisseria gonorrhoeae 0.8% among women between 15 and 49 years of age. Frequently, such infections are asymptomatic, resulting in diagnosis delay and postponing adequate treatment.
3 It is estimated that approximately 15% of infections by
Chlamydia trachomatis evolve to PID, and possibly this number is even higher regarding infections by
Neisseria gonorrhoeae. The cost for treatment in cases of PID in USA was estimated in $ 1,955.00 per patient, without inclusion of follow-up and treatment for complications. In this country, 4.4% of women aged between 18 and 44 years (approximately 2.5 million) reported previous history of PID.
4 In addition, surveys points to more than a million women in US present at least one episode of PID each year, and 20% of these need hospitalization for treatment.
5In Brazil, it is challenging to understand the entire magnitude of PID incidence, because in addition of not being a disease of compulsory notification, the screening of
Chlamydia trachomatis and
Neisseria gonorrhoeae in asymptomatic patients do not occur as well. Chronic cases of PID may lead to severe consequences, such as higher susceptibility to infection and transmission of Human Papillomavirus (HPV) and Human Immunodeficiency Virus (HIV).
6PID diagnosis is associated with the occurrence of sterility, preterm birth, ectopic pregnancy, cervical cancer, puerperal infections, chronic pelvic pain and recurrent infections of the upper genital tract.
7 After an episode, the prevalence of ectopic pregnancy is 15%, chronic pelvic pain is 18% and infertility due to Fallopian tube obstruction is 50%.
4 Furthermore, infections by
Chlamydia trachomatis and
Neisseria gonorrhoeae during pregnancy may be related to preterm births, premature rupture of membranes, fetal losses, intrauterine growth restriction and puerperal endometritis, besides conjunctivitis and neonatal pneumonia.
8Few studies investigated the prevalence of
Chlamydia trachomatis infection in Brazilian female population, with results varying from 10.7% to 58.54%.
6,9Frequently, PID is reported in young women at menacme (15 to 24 years), sexually active, with multiple partners, cervical ectopy, other sexually transmitted infections (STI), smoking, vaginal douching, insertion of intrauterine device (IUD) for less than 20 days and previous history of PID. Furthermore, other risk factors are low socioeconomic status, living in urban environment, being black, acting in sex work, being previously submitted to abortion, among others. On the other hand, the use of condom decreases the risk of contracting the disease.
1,7,10,11 Besides, it is well known that PID is a sensitive condition to Primary Healthcare (PHC), which implies that proper care in this level has the potential of decreasing its incidence.
Hereupon, some studies identified a diminish in PID hospitalizations after the implementation of Family Health Strategy (FHS).
12In face of the importance of PID in the country’s epidemiologic scenario, the scarceness of researches regarding the subject is startling, mainly concerning the trend of hospitalizations by this disease in the last years. In this way, the aim of this study was to assess the temporal trend of hospitalizations for PID in Brazil and its regions between 2000 and 2019.
MethodsA longitudinal ecological study was carried out (temporal trend). The study population comprised women of an age range from 10 years or more that underwent hospitalization registered in the Hospital Information System of SUS (Unified Health System) – SIH/SUS (Portuguese acronym) in Brazil in the period from 2000 to 2019.
Hospitalizations were selected by place of residence of women with 10 or more years whose cause of hospitalization was classified as “Inflammatory Diseases of female pelvic organs” (International Statistical Classification of Diseases and Related Health Problems- ICD: N70-N77).
13 Data on population, for calculation of hospitalization rates, were also obtained from DATASUS. Data were obtained by year, great regions and age ranges.
Rates of hospitalization were estimated (for 100,000 women), specifically for PID, stratified by age ranges and great regions in Brazil. Rates were presented in the form of line graphs. The total rate was standardized for age by the global standard population.
14The analysis of temporal trends from rates was carried out with the use of segmented linear regression (joinpoint regression), using statistic software
Joinpoint Regression, version 4.8.0.1 (
Statistical Research and Applications Branch, National Cancer Institute, Rockville, MD, EUA). This model of regression enables to estimate the average annual change for the period of study and the points (years) of modification of trend. The software uses minimum and maximum joinpoints (until reach the maximum number), verifying if the changes are statistically significant. The test of significance uses the Monte Carlo permutation test. This permutation tests a pack of data in order to select joinpoints. The Annual Percent Change (APC) estimated from the coefficients, is a summary of the trends in the rates in short time intervals. The Average Annual Percent Change (AAPC) performs geometrical calculations accumulated in the APC trends. This method transforms geometrical calculations of inclination coefficients in a variable of annual percentage.
15The study was carried out with the search of information registered in the SUS IT Department – DATASUS (
http://tabnet.datasus.gov.br/).
16 For this reason, the research was dismissed of approval by the Human Research Ethics Committee, according to the resolution of CONEP number 510 from 4/7/2016.
ResultsFigure 1 shows rates of hospitalization for PID by age range in Brazil and great regions, from 2000 to 2019. In the analyzed period, it is noticed that the North region showed higher rates of hospitalization for PID, and the South and Southeast regions, the lower. Furthermore, it is observed that the most affected age range was 20 to 29 years, with the exception of South and Southeast regions, which showed higher values for the 30 to 39 years age range. Women in the age range above 60 years showed lower hospitalization rates in all regions. The graphics suggest decrease in the hospitalization rates in the higher portion of the analyzed period in all regions.
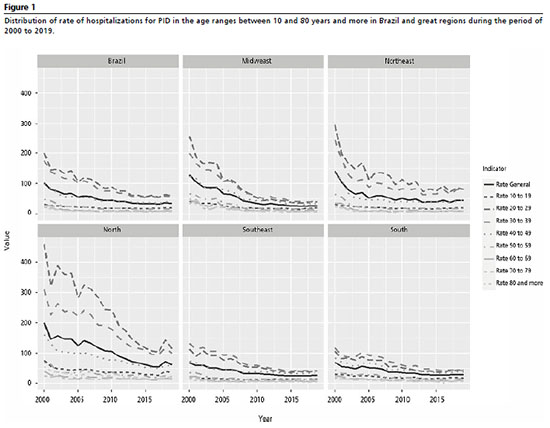
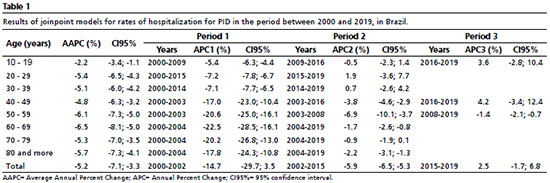
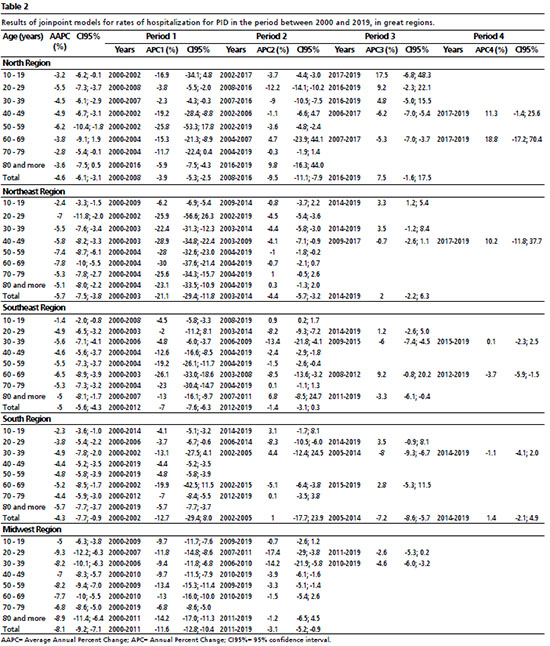
The analysis of joinpoint models indicates that the hospitalization rate for PID in Brazil as a whole had an average reduction of 5.2% per year during the period from 2000 to 2019. The Midwest region had the higher average annual reduction (8.1%), followed by Northeast (5.7%), Southeast (5.0%), North (4.6%) and South (4.3%) regions. The age ranges with higher decrease in the period were 60 to 69 years in Brazil, in the Northeast and Southeast, of 50 to 59 years in the North, of 80 or more years in the South and 20 to 29 years in the Midwest (Tables 1 and 2).
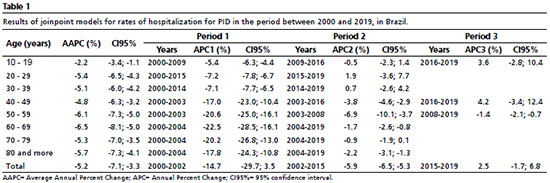
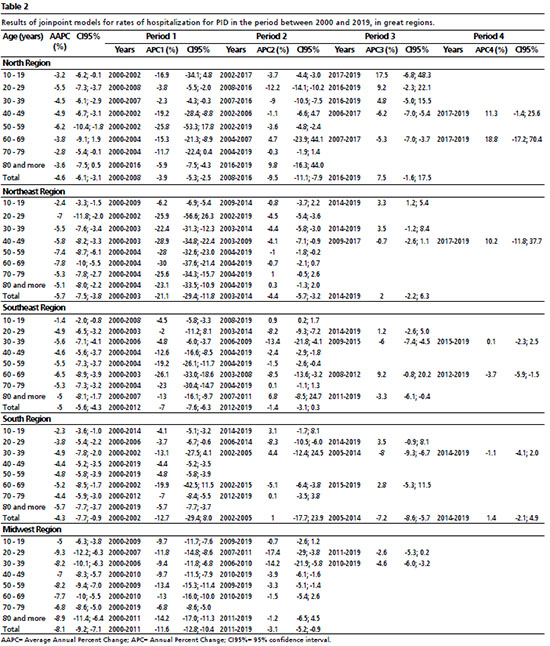
Considering all regions and age ranges, only the age ranges of 60 to 69 years and 80 or more in the North region did not show significant decrease in the period from 2000 to 2019. When observing the segments of periods in age ranges and regions, most showed significant decrease in period 1, approximately half in period 2, a minority in period 3 and only the age range from 60 to 69 years in Southeast region in period 4. The only age range that showed a significant increase was the 10 to 19 years age range in Southeast region in the period from 2008 to 2019 and Northeast region in the period from 2014 to 2019. (Tables 1 and 2).
DiscussionThe results found point out to a decrease in hospitalizations for PID, in all regions and almost all age ranges. A possible explanation for this reduction may be related to the increase in medical appointments at SUS. In 2013, the National Survey of Health (PNS – Portuguese acronym) indicated that in Brazil, 97% of people who sought for a medical appointment at the SUS primary healthcare succeeded obtaining it. In the great regions, the proportions of medical care at the first time of search oscillated around the national average and varied in 93.6% in the North Region to 96.3% in Southeast and South regions.
17 The 2019 PNS indicated that 82.3% of women that sought for medical appointments in the last 12 months had obtained it.
18The Midwest region had the highest annual average reduction of hospitalizations for PID, followed by Northeast, Southeast, North and South regions. A possible explanation for the decrease of hospitalizations for primary care sensitive conditions (ICSAP – Portuguese acronym) in the Northeast region may be linked to the implementation of the More Doctors Program (
Programa Mais Médicos) in Brazil, once after the second semester of 2013, this region had the higher number of professionals from this program. During this period, this region showed a decrease in hospitalizations for primary care sensitive conditions up to 35% between September 2012 and August 2015.
19 On the other hand, it is noticed that the absence of relationship with the FHS is associated with a higher risk of ICSAP in Paraná.
12The only age range that showed significant increase was 10 to 19 years in Southeast region in the period between 2008 and 2019 and Northeast region in the period between 2014 and 2019. This increase may be related to the frequency of condom use and risk behaviors by the women of this age range. Results from the National School-based Health Survey of 2015, for example, showed that 25.3% of Brazilian students in the age range of 16 to 17 years declared not having used condom at the first sexual intercourse and 40.3% declared not having used in the last intercourse. Furthermore, 15.6% affirmed not having received information about methods for protection against STIs at school.
20 The higher incidence of sexual transmitted infections is found in adolescents: lack of experience and information favors higher exposition to STI risk factors. In this stage of life, access to information is important, once STIs are avoidable if prevention is started at the beginning of adolescents’ sexual life. The exposure to risk factors in adolescence may favor complications to women in adulthood.
21 For example, in Rio Grande do Sul, the prevalence of
Chlamydia Trachomatis was more frequent in adult women that started their sexual lives with 15 years or less.
22 Another example occurred in São Paulo State, in which 62.4% of assessed women that started their sexual lives with more than 15 years did not use condom at the first sexual intercourse.
23The results of the present study indicated that the hospitalization rates demonstrated differences over time, being the higher rates found in North and Northeast regions, which may be related to regional socioeconomic inequalities. Socioeconomic factors may present a certain influence over the risk exposure to STIs in women of low socioeconomic status. A research conducted in Campinas, located in the Southeast region, indicated that women of high or medium socioeconomic status are more prone to use condoms as a barrier device for STIs than those of low socioeconomic status.
24 Educational level is another important element in regard of outlining these differences. Women with 8 years or less of schooling present higher prevalence of
Chlamydia Trachomatis than those with higher schooling.
22 A research conducted in the Northeast region indicated that women of low income and schooling have a 3 times higher risk of contracting cervical cancer than women of higher schooling. Women with 3 years or less of schooling showed little knowledge about the screening of this kind of cancer.
25 In addition to education, other factors impair the access to information and prevention of diseases, such as income, employment and quality of life.
Compared to other regions, North and Northeast regions show higher indexes of poverty. In North and Midwest regions, socioeconomic development influenced the population growth of these regions. However, social and health services did not meet the demand that was generated. On the other hand, socioeconomic improvements in the Northeast are concentrated in few regions.
26 These inequalities in the access to healthcare system may explain a part of regional differences in hospitalizations for PID.
Private health insurance plans could provide other ways of access to healthcare beyond the SUS. However, NHS 2019 indicated that 71.5% of Brazilians depend solely on SUS to perform consultations and treatments. Of those who possess private health insurance plan, only 27.4% are women.
18 When the access to private health insurance plan is portrayed by regions, PNAD 2013 indicated that of the interviewees from Southeast region, only 37% had coverage.
27 The regions where women showed higher rates of hospitalization for PID were exactly the regions in which access to healthcare services, public or private, are scarcer.
The results found in this study pointed to a decrease in hospitalization rates over time. In the studied period, between 2000 and 2019, all age ranges had reduction, except for the 10 to 19 age range, which presented a significant increase for Southeast and Northeast regions. The reduction of hospitalizations suggests that women in the other age ranges had more access to information and/or health professionals over the studied periods. The disparities of reductions of hospitalizations found by region evidence the need for expanding public policies focused to women’s healthcare, mainly in the adolescence stage. In this sense, we highlight the creation of prevention programs concerning PID, as well as the awareness about possible consequences of sexual risk behaviors. We add to this proposal public policies that are conceived according to the socioeconomic reality of each region, being aware of local singularities, thus outlining possibilities of access to information, as well as stimulating the use of condoms and expanding the access to health professional by women in socioeconomic vulnerability conditions.
References1. Laureau SM, Beigi RH. Pelvic Inflammatory disease and tuboovarian abscess. Infect Dis Clin North Am . 2008; 22 (4): 693-708.
2. WHO (World Health Organization). Global health sector strategy on sexually transmitted infections 2016-2021: toward ending STIs. 2016 [access in 20202 ago 22]. Available from:
http://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-eng.pdf?sequence=13. Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLoSONE. 2015; 10 (12): e0143304.
4. Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Family Phys. 2019; 100 (6): 357-64.
5. Batista MSG. Doença inflamatória pélvica aguda: do diagnóstico ao tratamento. [dissertação]. Coimbra: Faculdade de Medicina da Universidade de Coimbra; 2011.
6. Reis-Góes FS, Lima FLO, Amorim CF, Santa Izabel TS. Prevalence of chlamydia trachomatis infection in the brazilian female population: a review article. RSD. 2020; 9 (7): e567974483.
7. Gontijo LS, Fonseca AOD, Bispo KS. Perfil epidemiológico da doença inflamatória pélvica nas mulheres atendidas nos centros de estratégia de saúde da família na cidade de Montes Claros/MG. Rev Pesq Saúde. 2016; 18 (3): 121-7.
8. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de DST, AIDS e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para atenção integral às pessoas com infecções sexualmente transmissíveis. 2020. [access in 2020 set 26]. Available from:
http://www.aids.gov.br/pt-br/pub/2015/protocolo-clinico-e-diretrizes-terapeuticas-para-atencao-integral-pessoas-com-infeccoes.
9. Santos LM, Ulian WL, Trindade JQ, Sousa FDM, Oliveira JFG, Pereira CCC,
et al. Prevalência da infecção endocervical de Chlamydia Trachomatis em universitárias do estado do Pará, Região Amazônica, Brasil. Reva Pan-Am Saúde. 2017; 8 (3): 27-33.
10. Quinet BB, Pereira CR, Luz FML, Silva GGT, Machado PAB, Salera RB,
et al. Doença inflamatória pélvica: atualização. RevMed Minas Gerais. 2012; 22 (5): S50-S54, 2012.
11. Santos JR, Gonçalves E. Rastreio de Infecções Sexualmente Transmissíveis não víricas nos adolescentes: qual o estado da arte. Nascer Crescer. 2016; 25 (3): 163-8.
12. Pitilin EB, Gutubir D, Molena-Fernandes CA, Pelloso SM. Internações sensíveis à atenção primária específicas de mulheres. Ciênc Saúde Colet. 2015; 20 (2): 441-8.
13. World Health Organization (WHO). Classificação Estatística Internacional de Doenças e problemas relacionados à saúde: CID-10. São Paulo: Edusp; 1994.
14. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A new WHO Standard. World Health Organization 2001; 14: 1-14. [access in 2020 set 26]. Available from:
https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf15. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000; 19: 335-51 (correction: 2001;20:655).
16. Ministério da Saúde (BR). Departamento de Informática do SUS (DATASUS). Sistema de Informações Hospitalares do SUS (SIH/SUS). Brasília (DF): Ministério da Saúde (BR); 2020 [access in 2020 nov 23]. Available from:
http://tabnet.datasus.gov.br/17. Instituto Brasileiro de Geografia e Estatística (IBGE). Coordenação de Trabalho e Rendimento. Pesquisa nacional de saúde 2013: acesso e utilização dos serviços de saúde, acidentes e violências. Brasil, grandes regiões e unidades da federação. Rio de Janeiro: IBGE; 2015. 105p. [access in 2020 nov 19]. Available from:
https://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf18. Instituto Brasileiro de Geografia e Estatística (IBGE). Coordenação de Trabalho e Rendimento. Pesquisa nacional de saúde 2019: informações sobre domicílios, acesso e utilização dos serviços de saúde. Brasil, grandes regiões e unidades da federação. Rio de Janeiro: IBGE; 2020. 89p. [access in 2020 nov 19]. Available from:
https://biblioteca.ibge.gov.br/visualizacao/livros/liv101748.pdf19. Gonçalves RF, Sousa IMC, Tanaka OY, Santos CR, Brito-Silva K, Santos LX,
et al. Programa Mais Médicos no Nordeste: avaliação das internações por condições sensíveis à Atenção Primária à Saúde. Ciênc Saúde Colet. 2016; 21: 2815-24.
20. Instituto Brasileiro de Geografia e Estatística (IBGE). Coordenação de População e Indicadores Sociais. Pesquisa nacional de saúde do escolar: 2015. Rio de Janeiro: IBGE; 2016. 132 p. [access in 2020 nov 19]. Available from:
https://biblioteca.ibge.gov.br/visualizacao/livros/liv97870.pdf21. Rodrigues MJ. Doenças Sexualmente Transmissíveis (DST) na Adolescência. Nascer Crescer. 2010; 19 (3): S200.
22. Garcês AX, Martinez AMB, Gonçalves CV, Germano FN, Barral MFM, Vieira VC. Prevalência de Chlamydia Trachomatis e fatores de risco associados à infecção detectada em amostra endocervical. Rev Bras Ginecol Obst. 2013; 35 (8): 379-83.
23. Pinto VM, Basso CR, Barros CRS, Gutierrez EB. Fatores associados às infecções sexualmente transmissíveis: inquérito populacional no município de São Paulo, Brasil. Ciênc Saúde Colet. 2018; 23 (7): 2423-32.
24. Jiméne AL, Gotlieb SLD, Hardy E, Zaneveld LJD. Prevenção de doenças sexualmente transmissíveis em mulheres: associação com variáveis sócio-econômicas e demográficas. Cad Saúde Pública. 2001; 17 (1): 55-62.
25. Mendonça VG, Guimarães MJB, Lima Filho JL, Mendonça CG, Martins DBG, Crovella S,
et al. Infecção cervical por papilomavírus humano: genotipagem viral e fatores de risco para lesão intraepitelial de alto grau e câncer de colo do útero. Rev Bras Ginecol Obstet. 2010; 32 (10): 476-85.
26. Albuquerque MV, Lima LD, Ferreira MP, Fusaro ER, Lozzi FL. Desigualdades regionais na saúde: mudanças observadas no Brasil de 2000 a 2016. Ciênc Saúde Colet. 2017; 22 (4): 1055-64.
27. Viacava F, Bellido JG. Condições de saúde, acesso a serviços e fontes de pagamento, segundo inquéritos domiciliares. Ciênc Saúde Colet. 2016; 21 (2): 351-70.
Received on January 22, 2021
Final version presented on January 11, 2022
Approved on August 27, 2022
Author’s contribution: Perciney P: Conceptualization (Equal). Methodology (Equal). Writing – original draft (Equal). Writing – review and edition (Equal). Costa ALS:Writing – original draft (Equal). Writing – review and edition (Equal). Leite ICG: Conceptualization (Equal). Methodology (Equal). Writing – original draft (Equal). Writing – review and edition (Equal). Nogueira MC: Conceptualization (Equal). Methodology (Equal). Writing – original draft (Equal). Writing – review and edition (Equal).
All authors approved the final version of the article and declare no conflicts of the interest.
 ; Ana Luísa Soares Costa2
; Ana Luísa Soares Costa2 ; Isabel Cristina Gonçalves Leite3
; Isabel Cristina Gonçalves Leite3 ; Mário Círio Nogueira4
; Mário Círio Nogueira4