ABSTRACT
OBJECTIVES: to analyze a correlation between self-efficacy and social support of mothers of preterms in early postpartum.
METHODS: cross-sectional study, carried out with 120 mothers of preterm infants from a Maternity School, from June to September 2018. Sociodemographic, reproductive and scales were used to assess the Maternal Self-Efficacy and Social Support. A descriptive analysis was carried out and the Mann-Whitney Test, Kruskal Wallis Test and Spearman correlation were applied.
RESULTS: there was a positive correlation between self-efficacy, parity (p=0.017), years of schooling (p=0.017) and Social Support (p=0.002). An unexpected finding was a high self-efficacy among mothers up to eight years of schooling, in the countryside of the State and with low income.
CONCLUSION: social support, in all dimensions: material, affective, emotional, information and social interaction, proven to be a predictor of maternal self-efficacy.
Keywords:
Self-efficacy, Newborn, Premature, Social support, Child's health
RESUMO
OBJETIVOS: analisar a correlação entre autoeficácia materna e apoio social de mães de recém-nascidos prematuros no período de pós-parto precoce.
MÉTODOS: estudo transversal, realizado junto a 120 mães de prematuros de uma Maternidade Escola, no período de junho a dezembro de 2018. Utilizaram-se dados sociodemográficos, reprodutivos e escalas para Avaliação da Autoeficácia Materna e Apoio Social. Procedeu-se a análise descritiva e aplicaram-se os testes de Teste Mann-Whitney, Teste de Kruskal Wallis e correlação de Spearman.
RESULTADOS: evidenciou-se correlação positiva entre autoeficácia, paridade (p=0,017), anos de estudo (p=0,017) e Apoio Social (p=0,002). Um achado inesperado foi a alta autoeficácia entre mães com até oito anos de estudo, do interior do estado e de baixa renda.
CONCLUSÃO: o apoio social, em todas as dimensões: material, afetivo, emocional, de informação e interação social, mostrou-se preditor da autoeficácia materna.
Palavras-chave:
Autoeficácia, Recém-nascido, Prematuro, Apoio social, Saúde da criança.
IntroductionPrematurity affects approximately 15 million newnates worldwide every year, and its complications cause about one million deaths.
1 Compared to other countries, Brazil ranks the ninth position among the ten countries with high prematurity rates, a percentage of 11.2 per 100 births.
2 In Ceará, 60.7% ofdeaths in the early neonatal period were of premature newborns (NB).
3For
Sistema Único de Saúde (SUS) (Public Health System), it is essential to identify mothers' sociocultural context as well as their self-efficacy and social support network for premature newborns'care. In this scenario, the mother's self-efficacy has a direct influence on the NBs'physical, cognitive, and social development, in addition to reducing postpartum stress.
4 Social support involves material and psychological resources that people have access to through their social networks and provide support in different areas: emotional, material, educational, and among others.
4Health professionals working in the neonatal care unit are part of the secondary social support network that should promote maternal self-efficacy, since it configures the belief in personal capacity to organize and perform certain actions. Such belief influences the action of choices that will be performed and involves the time they have persevered facing obstacles and failures.
5In this context, the use of scales in the neonatology working process helps to identify the mother and childbinomial'snecessity, contributing to the assessment of self-efficacy and necessity of interventions to the NB, directing the plan of care.
6Studies using the efficacy and social support scales have shown that there is a relationbetween social support and self-efficacy.
7,8 An effective social support helps individual to face difficult moments and to deal with stressful events, improving skills and increasing self-efficacy.
6 A study evaluated the perception of the existence of social support as emotional, informational, material, affective, and positive social interaction to face different life situations using the Social Support Scale.
9The identification of social support seems to bring implications for the practice, such as the necessity to strengthen social emotional and informational support to enhance and direct intervention strategies in children'scomplex care.
10 Understanding this scenario allows health professionals to review their skills and abilities, favoring the co-responsibility of care, to the extent that they can mediate different institutional sectors in favor of meeting the needs of service users.
11,12Thus, the study is justified, although some mothers may feel able to perform the most complex tasks of parenthood, while others may have relatively diminished expectations of their caregiving abilities, especially facing premature birth, highlighting the necessity to conduct further studies on the subject, especially in a capital city in the Northeast of Brazil, which still presents a marked number of deaths of preterms, higher than in more developed regions in Brazil.
13Based on the foregoing, the objective of this study is to analyze the correlation between maternal self-efficacy and mothers' social support of preterms in the early postpartum period.
MethodsLongitudinal and prospective study conducted in the Neonatal Care Unit (NCU) in a maternity hospital in Fortaleza, capital of Ceará. The unit is part of the network of the university hospitals of the Ministry of Education and certified by the
Iniciativa Hospital Amigo da Criança (Child's Friend Hospital Initiative). The maternity unit is a reference for the high-risk pregnant women'scare, and in the first half of 2018 it had an average of 220 live births in the NICU, an average that remains the same today.
Based on this profile, a sample of 120 women was calculated, with a significance level of 5% and sampling error of 4%. Sample power was calculated a posteriori using the G*Power 3.1.9.2 program for the outcome of the correlation between self-efficacy and social support, with a value of 99%.
Mothers were selected by convenience from the continuous admission of the binomials during the period from June to December 2018. Inclusion criteria were: mothers who were discharged from the hospital but their neonates were hospitalized, and exclusion criteria: adolescent mothers, mothers with psychiatric history and death of the newborn during the study period. Of the 132 mothers addressed, 120 made up the sample, eight did not agree to participate, and four had stillborn babies.
During the period of data collection, the researchers made daily visits to the hospital in order to collect mothers that entered the service. The filling out of the questionnaires took about 20 minutes and occurred in a reserved room. It is worth mentioning that the researchers became present in a daily routine of the service, facilitating the contact and proximity with the participants.
Thus, three instruments were applied, the first was a questionnaire involving sociodemographic data and reproductive health.
6 The second was the
Escala de Autoeficácia Materna Parental Percebida14 (Perceived Parental Self-EfficacyScale), composed of twenty items with Likert-type answers with four options of answer. The score of the scale was calculated by the arithmetic mean, where the higher the score, the higher the perceived maternal self-efficacy ranging between 19 and 76 points. The scale is composed of four subdomains or factors: factor 1 refers to the mother's procedures in care in relation to the baby and assesses maternal perceptions about her ability to perform activities such as Feeding; factor 2 maternal evaluation about her ability to elicit behavioral changes; factor 3 maternal perceptions about the ability to understand and identify behavioralchanges; factor 4 represents the situational signs and beliefs that analyze maternal beliefs in relation to her ability to maintain interaction with the baby.
14The last instrument applied was the
Escala de Apoio Social15 (Support Social Scale) with 19 questions and Likert-type answers with five options ranging from 1 (never) to 5 (always), where a higher score reflects higher levels of social support. The scale scores between19 and 95 points, with scores above 57 considered as satisfactory. In its original form, the
MOS-SSS was designed to cover five dimensions of social support: material - provision of practical resources and material help; affective - physical demonstrations of love and affection; positive social interaction - counting on people with whom to relax and have fun; emotional - social network ability to satisfy individual needs regarding emotional problems, for example, situations that require secrecy and encouragement in difficult moments in life; information - counting on people who advise, inform, and guide. Instruments 2 and 3 presented in its validations Cronbach's alpha greater than 0.91, showing high internal consistency.
After the collection, the data were compiled in Microsoft Office Excel and analyzed in the Statistical Package for the Social Sciences (SPSS), version 22.0 for Windows and presented in tables. Descriptive statistics were used, through mean frequency and for Chi square, Mann-Whitney test, Kruskal Wallis tests and Spearman correlation and multiple linear regression, with a significance level of 5%.
The study was approved by the Research Ethics Committee of the institution under CAAE 89651418.0.0000.5050 with approval on May 29, 2018.
ResultsThe mothers' age ranged from 18 to 46 years old, with a mean of 25.7 years; they were married/stable union (75%), with more than nine years of schooling (64%), most were unpaid (60.8%), with family income between one and two salaries, and 73 (60.8%) received support from the governmental
Bolsa Família(Family Welfare) Program. When the sociodemographic data were compared with the scales, a comparison of the means showed an association between years of study and Maternal Self-efficacy (
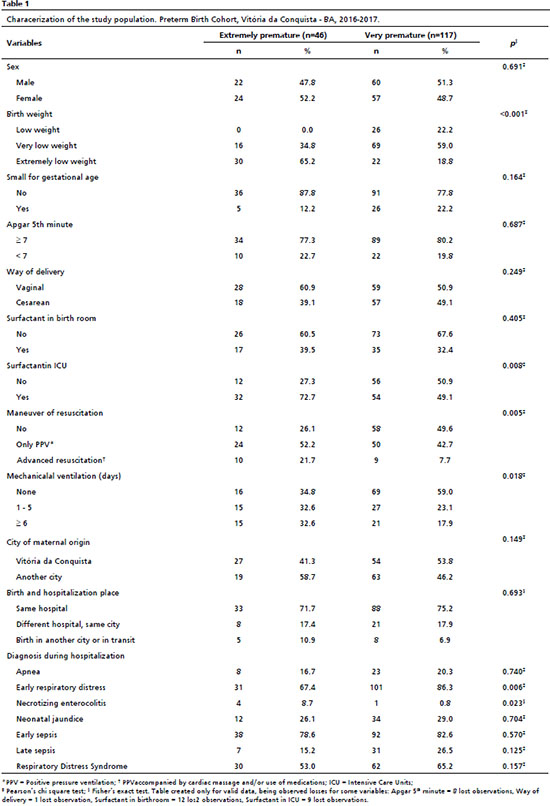
p=0.017). Overall, the average self-efficacy and social support scores of mothers were satisfactory, with scores between 57 to 64 points (self-efficacy) and 64 to 82 points (social support), close to the maximum scores of the respective scales (Table 1).
Regarding to data on pregnancy and puerperium, more than half of the mothers were multiparous (53.3%), with babies less than seven days old (49.3%) and gestational age at birth classified as borderline premature with gestational age (GA) of ≥ 31 and < 34 weeks (45.8%). Most puerperal women (98.3%) had prenatal care (40%) six or more consultations, (52.5%) reported receiving guidance on baby care and (50%) about breastfeeding. As for the participation in groups for pregnant women, (84.2%) commented they had not participated. Most mothers (89.2%) stated that they would have support to perform baby's care. As for the information sources on care, (43.3%) referred to health professionals, (26.7%) family members, and (25.8%) searches on the internet/social networks.
The study showed that multiparous women, with more than 15 days of hospitalization and with a borderline prematurepresented a high parental efficacy (
p=0.017). Puerperae women who had more than six prenatal consulations and who received guidance on breastfeeding and baby care also presented high scores. Mothers who did not participate in pregnancy groups, who did not have support to perform baby care, and who sought information about baby care on the internet/network showed lower efficacy (Table 2).
There is a significant correlation of the social support scale with the domains (Table 3): Material (
p=0.025), Emotional (
p=0.002), Information (
p=0.003), Affective (
p=0.003) and Positive Social Interaction (
p=0.015) with Perceived Maternal Self-efficacy.
Discussion The results of the study showed a positive association between self-efficacy and schooling. Women with up to eight years of schooling, coming from the countryside, and with lower income show a slightly higher mean self-efficacy. Although these are unexpected findings and contradict other studies,
16 this profile contributes to the permanence of women in the NICU, including greater access to information and, consequently, influence permanence in the service and greater confidence in their parenting practices.
Schooling showed a similar result to another trial with mothers of hospitalized babies in intermediate care units.
6 Maternals' schooling level can positively influence the comprehension on the socialized information with the health professionals and, consequently, the safety of the care offered.
16 Another point to be added is that most of them counted on their partners' support, a relevant information in terms of social support, becoming a differential for the baby'scare.
17Women who received from
Bolsa Família (Family Welfare) program and had no financial income of their own had higher self-efficacy. It is known that greater material support can have a significant impact on parental efficacy.
15 Since they do not have a paid job, the mothers' availability to strengthen ties within the hospital may have increased social support from the health professionals at the service.
A positive mean association was found between parity and maternal self-efficacy, corroborating the
Teoria Social Cognitiva (Social Cognitive Theory), since women who have already had children feel more confident in parenting than primiparous women. In addition, multiparous women have higher perceptions of the social support received. This finding may be influenced by the mothers' age and by the fact that the hospital allows preterm to be visited by their siblings. The presence of the another child in the hospital environment reduces stress and worries of the mothers, increasing parental confidence and social support.
18 These and other findings strengthen the differential that the
Iniciativa Hospital Amigo da Criança(Child's Friend Hospital Initiative) can contribute to strengthening the mother, child and family's triad.
Mothers with babies less than seven daysof hospitalization and moderately premature, presented lower self-efficacy, but obtained the highest average on social support. These data are justified by the child's clinical status, since it is known that mothers with children in stable clinical condition feel more confident, unlike those who require more monitoring and need help from others.
5 New studies should be carried out taking into account child's health status, in order to know how these factors can affect the parenting process and the social support received.
Women who had more than six prenatal consultations, received guidance on breastfeeding and baby care, participated in groups for pregnant women, and those receive support to perform baby's care, had higher levels of self-efficacy and perceived social support. These findings show that health professionals, when conducting educational group activities, possible social connectionscan be made, since there are more activities outdoors than at home, reconnecting with friends and family, and new relationships through activities related to babies and parents.
19In addition, mothers who refere in having family members as their main source of information, had higher maternal self-efficacy and social support. A study that examined the association of grandmothers' adequate knowledge about breastfeeding and complementary feeding in young children showed that their involvement with mothers positively influences maternal knowledge. In other words, the support of grandmothers, by improving the mothers'self-efficacy contributing to a child's healthier development and growth.
20Possibly, this process, both on learning educational activities in group and in the family context, occurs through modeling. That is, women perceive their mothers and fellow pregnant women as more experienced in motherhood and, when they receive practical/material support, they feel more confident to perform the baby'scare.
3 Thus, support groups formed by other pregnant women and family members could be useful for new mothers to improve self-efficacy through social models.
Mothers who search for information about baby's care on the Internet/social network showed a lower parental efficacy than mothers who use family members or health professionals to clarify their doubts. This fact is possibly justified by the access to information without scientific evidence available online.
21 This aspect is important because the general population has increasingly relied on virtual social networks to learn about health, so it is the health professionals'role to inform these mothers how to accessreliable sources of information, avoiding even fake news, so widespread nowadays.
In this study, social support proven to be a predictor of perceived maternal self-efficacy, in other words, the greater the social support received, the better preterm NB mothers adapt to the parenting process. Furthermore, all dimensions of social support - material, affective, emotional, information, and positive social interaction - seem to influence self-efficacy. A study indicates that material support has been shown to be as important as other dimensions for parental satisfaction, possibly due to the social context experienced by these mothers.
22 Emotional support has been shown to be significant in relation to self-efficacy, being a predictor of parental satisfaction. In addition, informational support can also affect self-efficacy, confirming what was previously discussed about adequate and reliable information from the media.
Educational interventions such as educational materials, home visits, brochures, cell phone apps, and phone calls, enable the exchange of information and experiences, improving skills and consequently increasing parents' self-efficacy.
12An unexpected finding was the positive mean associated between the self-efficacy of women up to eight years of schooling, from the countryside, and in a greater socioeconomic vulnerability. Although these results contradict other studies, in which they reveal the importance of health services that facilitate the access and permanence of these mothers in support homes provided by the institution. The
Iniciativa Hospital Amigo da Criança (Child's Friend Hospital Initiative) and
Rede Cegonha (Stork Network) are public policies that focus in care beyond the NICU favoring the reception, access to evidence-based information, and, consequently, greater confidence in their parenting practices in this critical period of life.
23In the study, multiparous women showed higher levels of parental efficacy. Thus, health professionals must value the mastery and vicarious experiences which, according to Bandura
et al. 5 must contemplate the support network of more experienced mothers, favoring in educational activities in which they can share their experiences with primiparous women and their support network.
Among the limitations of the study is the fact that it was a single-center research in a single reference hospital, which may have made it difficult to generalize the data. Finally, we conclude that social support proven to be a predictor of maternal self-efficacy, as well as all its dimensions: material, affective, emotional, information and social, reinforcing the importance of a comprehensive care for families who experience prematurity. In view of the above, future research should be conducted in larger populations in order to corroborate the findings and expand the evidence in the area of care for premature infants.
References1. Reymundo MG, Suazo JAH, Aguilar MJC, Faura FJS, Galiana GG, Peinador YM,
et al. Recomendaciones de seguimiento del prematuro tardío. An Pediatr (Barc). 2019; 90 (5): 318.e1-318.e8.
2. Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D,
et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019 Jan; 7 (1): e37-46.
3. Cavalcante ANM, Araújo MAL, Lopes SVS, Almeida TIF, Almeida RLF. Epidemiology of neonatal mortality in Ceará in the period from 2005-2015. Rev Bras Promoç Saúde. 2018; 31 (4): 1-8.
4. Skupien SV, Souza SRRK, Wall ML, Trigueiro TH, Prandini NR, Ferreira CB. Rede social de apoio à mulher no aleitamento materno: revisão integrativa. Rev Enferm Cent O Min. 2022; 12 (1): 43-8.
5. Bandura A, Azzi RG, Polydoro S. Teoria social cognitiva: conceitos básicos. Porto Alegre: Artmed; 2008.
6. Sousa Cotrim DM, Costa Neto SB. Estudios sobre la percepción de la autoeficacia de los padres: una revisión de la literatura. Rev Subjetividad Procesos Cognitivos. 2021; 25 (1): 23-46.
7. Lima TJS, Souza LEC. O suporte social como fator de proteção para as mães de crianças com Síndrome da Zika Congênita. Ciênc Saúde Colet. 2021; 26 (8): 3031-40.
8. Alinejad-naeini M, Razavi N, Sohrabi S, Heidari-beni F. The association between health literacy, social support and self-efficacy in mothers of preterm neonates. J Matern Fetal Neonatal Med. 2019; 34 (11): 1703-10.
9. Zanini DS, Peixoto EM, Nakato TC. Escala de Apoio Social (MOS-SSS): Proposta de Normatização com Referência nos Itens. Trends Psychol. 2018, 26 (1): 387-99.
10. Baldini PR, Lima BJ, Pina JC, Okido ACC. Mães de crianças que necessitam de cuidados contínuos e complexos: fatores associados ao apoio social. Esc Anna Nery. 2021; 25 (3): e20200254.
11. Konstantyne T, Pereira BB, Caetano C. Benefícios e desafios do método canguru como estratégia de humanização e saúde. Rev Bras Saúde Mater Infant. 2022; (1): 7-9.
12. Cheng LA, Mendonca, Lucena JM, Rech CR, Farias Júnior JC. Is the association between sociodemographic variables and physical activity levels in adolescentes mediated by social support and self-efficacy? J Pediatr (Rio J). 2020; 96 (1): 46-52.
13. Santos LM, Conceição TB, Gomes AS, Silva CSG, Ramos MSX, Passos SSS,
et al. Caracterização de nascidos vivos prematuros em um município do nordeste brasileiro. Rev Soc Bras Enferm Ped. 2021; 21 (2): 85-90.
14. Barnes CR, Adamson-Macedo EN. Perceived maternal parenting self-efficacy (PMPS-E) tool: development and valuation with mothers of hospitalized preterm neonates. J Adv Nurs. 2007; 60 (5): 550-60.
15. Griep RH, Chor D, Faerstein E, Werneck GL, Lopes CS. Validade de constructo de escala de apoio social do Medical Outcomes Study adaptada para o português no Estudo Pró-Saúde. Cad Saúde Pública. 2005; 21 (3): 703-14.
16. Moraes AS, Aguiar RS. Dificuldades com a amamentação de recém-nascidos prematuros após a alta hospitalar: uma revisão integrativa. Rev JRG. 2021; 4 (8): 253-6.
17. Alves AB, Pereira TR, Aveiro MC, Cockell FF. Functioning and support networks during postpartum. Rev Bras Saúde Mater Infant. 2022; 22 (3): 667-73.
18. Martins MC, Boeckmann LMM, Melo MC, Moura AS, Morais RCM, Mazoni SR,
et al. Nursin mother`s perceotions when experiencing prematurity in the neonatal intensive care unit. Cogitare Enferm. 2022; 27: e80125.
19. O'neill P, Cycon A, Friedman L. Seeking social support and postpartum depression: A pilot retrospective study of perceived changes. Midwifery. 2019; 71: 56-62.
20. Angelo BHB, Pontes CM, Sette GCS, Leal LP. Knowledge, attitudes and practices of grandmothers related to breastfeeding: a meta-synthesis. Rev Latino-Am Enferm. 2020; 28: e3214.
21. Campana KSS, Curan GRF, Rossetto EG, Costa LLC, Silva LMF. Uso de aplicativos para smartphones visando a promoção da amamentação de prematuros: revisão de escopo. Adv Nurs Health. 2022; 4 (1): 21-39.
22. He J, Yimyam S, Namprom N. Breastfeeding self-efficacy, social support, and breastfeeding among Chinese mothers with late preterm infants. J Neonatal Nurs. 2022; 28: 21-5.
23. Ministério da Saúde (BR). Gabinete do Ministro. Portaria Nº 1.153, de 22 de Maio de 2014. Redefine os critérios de habilitação da Iniciativa Hospital Amigo da Criança (IHAC), como estratégia de promoção, proteção e apoio ao aleitamento materno e à saúde integral da criança e da mulher, no âmbito do Sistema Único de Saúde (SUS). Brasília (DF): Ministério da Saúde; 2014. [access in 2023 Abr 2]. Available from:
https://bvsms.saude.gov.br/bvs/saudelegis/gm/2014/prt1153_22_05_2014.htmlReceived on August 2, 2021
Final version presented on April 3, 2023
Approved on April 11, 2023
Associated Editor: Alex Sandro Rolland
Authors' contribution: Pinheiro SRCS, Gubert FA, Feitosa MP and Martins MC: conceptualization, data collection, formal analysis, investigation, method, project management and writing of the article; Beserra EV: collaboration in reviewing the writing; Gomes CC: collaboration in writing and reviewing the writing.
The authors approved the final version of the article and declare no conflict of interest.
 ; Fabiane do Amaral Gubert2;
; Fabiane do Amaral Gubert2; Mariana Cavalvante Martins3
Mariana Cavalvante Martins3 ; Eveline Pinheiro Beserra4
; Eveline Pinheiro Beserra4 ; Clarissa Costa Gomes5
; Clarissa Costa Gomes5 ; Marielle Ribeiro Feitosa6
; Marielle Ribeiro Feitosa6