ABSTRACT
OBJECTIVES: to evaluate the prevalence, clinical presentation, and surgical management outcomes of ectopic pregnancies in a tertiary hospital in Paraguay over a three-year period.
METHODS: this descriptive, cross-sectional observational study analyzed 389 clinical records of women aged 12-45 years who underwent surgical procedures for ectopic pregnancy at Hospital San Pablo from 2021 to 2023. Data on sociodemographic characteristics, symptoms, gestational age, implantation site, and surgical management were collected. Statistical analyses included frequencies, percentages, and measures of central tendency.
RESULTS: the prevalence of ectopic pregnancy requiring surgical intervention was 4.4% (17/389). The mean age of affected women was 32.4 years (SD±7.2). The most common presenting symptom was vaginal bleeding (58.8%), followed by lower abdominal pain (29.4%). Ultrasound confirmed 88.2% of cases, with right tubal implantation (58.8%) being the most frequent location. Salpingectomy was performed in 88.2% of cases, making it the predominant surgical treatment. Complicated ectopic pregnancies accounted for 76.5% of cases.
CONCLUSION: ectopic pregnancies requiring surgery remain an important clinical challenge, necessitating early diagnosis and prompt intervention to prevent severe maternal morbidity. Salpingectomy remains the standard surgical approach. Further research on non-surgical management strategies and long-term reproductive outcomes is warranted.
Keywords:
Ectopic pregnancy, Paraguay, Maternal mortality, Prevalence
IntroductionEctopic pregnancy refers to the implantation of a gestational sac outside the uterine cavity, with more than 90% of cases occurring in the fallopian tubes.
1 In the United States, the prevalence of ectopic pregnancy is approximately 1% to 2%,
2 while a study conducted in the Department of Obstetrics and Gynecology at the Faculty of Medicine, National University of Asunción, reported a prevalence of 1.47% in 2011.
3Diagnosis is based on clinical evaluation, which may include symptoms such as missed periods, light vaginal bleeding, and lower abdominal pain. Physical examination may reveal a tender adnexal mass, unilateral lower abdominal pain, cervical motion tenderness, a soft or slightly enlarged uterus inconsistent with the gestational age, signs of hemoperitoneum, or hypovolemic shock. These findings are supported by laboratory tests, including complete blood count, prothrombin time (PT), activated partial thromboplastin time (aPTT), platelet count, blood type, and positive qualitative or quantitative β-hCG levels, as well as abdominal or transvaginal ultrasound.⁴
Risk factors for ectopic pregnancy include a history of ectopic pregnancy, pelvic inflammatory disease, in vitro fertilization, tubal surgery, certain contraceptive methods, and smoking.⁵ Management options include expectant, medical, and surgical treatment.⁶ Methotrexate is the drug of choice for medical management, whereas surgical approaches include salpingostomy or salpingectomy. Expectant management—although the least invasive—is rarely the preferred option due to the risk of tubal rupture.⁷ It is recommended only for asymptomatic or mildly symptomatic, hemodynamically stable patients with a gestational age under five weeks, a tubal ectopic pregnancy smaller than 35 mm without cardiac activity on transvaginal ultrasound, no signs of intra-abdominal bleeding, and serum β-hCG levels below 1,000–1,500 IU/L.
7Over the past three decades, mortality due to ruptured ectopic pregnancies, one of the leading causes of maternal morbidity and mortality, has decreased significantly, currently accounting for approximately 2.7% of pregnancy-related deaths.
8Recent studies estimate that 10–30% of ectopic pregnancies may be eligible for medical or expectant management, depending on the clinical context, diagnostic timing, and patient stability.
9⁻11 Nonetheless, surgical treatment remains the most frequent approach in many low and middle-income settings, where late presentation and limited access to early diagnosis restrict the use of conservative strategies.
The objective of this study is to determine the prevalence of ectopic pregnancies recorded at
Hospital San Pablo between 2021 and 2023, and to provide a sociodemographic profile of the affected women.
MethodsA retrospective, descriptive, cross-sectional observational study was conducted at
Hospital San Pablo, Paraguay. A probabilistic random sampling method was used, with a minimum sample size of 378 patients, calculated based on an expected prevalence of 8%
9 in an infinite population, a 5% margin of error, and a 95% confidence level. Clinical records of patients aged 12 to 45 years who underwent surgical procedures between January 2021 and December 2023 were analyzed, collecting sociodemographic data such as age and origin. Inclusion criteria comprised clinical records of patients aged 12–45 years who underwent surgical procedures at
Hospital San Pablo during the study period and were residents of Paraguay. Exclusion criteria included incomplete or duplicate clinical records and only surgical ectopic pregnancies were considered. The study variables included age, origin, reason for admission and consultation, gestational age at diagnosis, implantation site, ultrasound diagnosis, medical or surgical management, maternal diseases associated with pregnancy, and pre-existing maternal conditions. "Complicated ectopic pregnancy" was defined a priori as any ectopic pregnancy presenting with one or more of the following: evidence of tubal rupture at presentation, hemoperitoneum documented intraoperatively or suspected clinically (signs of peritonitis with free intraperitoneal fluid on ultrasound), hemodynamic instability requiring resuscitation or blood transfusion, or clinical signs of acute abdomen necessitating urgent surgical intervention.
Data was extracted from clinical records and transferred to an Excel database. Statistical analysis was conducted using Microsoft Excel 2019 and Epi Info™ version 7.2 Quantitative variables were summarized using means and standard deviations, while qualitative variables were expressed as absolute frequencies and percentages.
Quality control involved reviewing a random sample of ten clinical records to ensure the presence of required data; these records were excluded from the final draft.
The study was approved by the Ethics Committee of
Universidad del Pacífico and
Hospital San Pablo (Approval dated 06/07/2025). Because this was a retrospective review of anonymized medical records, the requirement for individual informed consent was waived, in accordance with national regulations and the Declaration of Helsinki.
ResultsA total of 389 patient records were reviewed, with a mean age of 34.5 years (SD ±8.1). Of these, 20 records were excluded due to incomplete information, leaving 369 valid records for analysis. Among these, 17 cases of ectopic pregnancy requiring surgical intervention were identified and included in the final study sample (Figure 1). The prevalence of ectopic pregnancy that required surgical intervention in the sample was 4.4% (17/389). Of the number of ectopic pregnancies, the mean age was 32.4 (SD ±7.2).
The most frequent reason for consultation of patients with confirmed ectopic pregnancy was vaginal bleeding in 58.8% (10/17), followed by pain in the lower quadrants 29.4% (5/17) and a combination of both 11.8% (2/17)
Regarding the severity of the condition, 76.5% (13/17) have been diagnosed with complicated ectopic pregnancies and the rest were uncomplicated.
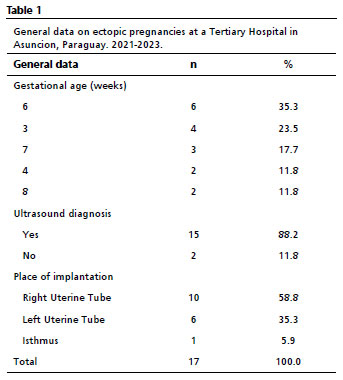
The mean number of weeks of gestation at the time of diagnosis of ectopic pregnancy was 5.5 (SD±1.8) and the most frequent was 6 weeks, which is equivalent to 35.3% (6/17) of cases. Most of them, 88.2% (15/17) were confirmed by ultrasound, and with regard to the implantation site, 58.82% (10/17) of these pregnancies took place in the right uterine tube (Table 1).
Regarding the treatment performed, all of these were resolved surgically, where decision was made based on the extent of tubal damage, hemodynamically stability, presence of rupture; Salpingectomy was the most frequent intervention in 88.2% (15/17) of the cases (Table 2).
DiscussionAccording to our findings, ectopic pregnancies (EP) requiring surgical treatment had a prevalence of 4.4% over a span of three years. This contrasts with the 7.7% prevalence reported by Berhe
et al.
11 The discrepancy may be attributed to differences in the population size analyzed: Berhe's study included approximately 1,000 patients, whereas our study reviewed 389 patients, of whom only 17 required surgical intervention. However, when compared to the findings of Mokhtari
et al.
12 our prevalence aligns within the expected range, with 44 EPs per 1,000 pregnancies, compared to the reported range of 2.9 to 53 EPs per 1,000 pregnancies.
Regarding the age of patients presenting with EP, our findings corroborate previous studies.
13-15 This consistency may be explained by the fact that women in their 30s are at their peak reproductive age.
16 Additionally, societal shifts in childbearing trends, where women prioritize personal and professional aspirations before pursuing motherhood, may contribute to the age-related patterns observed.
17,18 Other contributing factors include the accumulation of risk factors in these women, such as pelvic inflammatory disease, smoking, and pre-existing health conditions, all of which are established risk factors for EP.
18-22When it comes to the clinical presentation of EP, immediate action is crucial due to the rapid deterioration that can occur in these patients. In our cohort, the most common presenting complaint was per vaginal bleeding, consistent with findings by Stabile
et al.
21 In terms of severity, 76% of our cases required additional measures to stabilize the patients before surgical intervention, a finding comparable to other studies.
21,22One patient in our series had previously received methotrexate prior to definitive management. Medical treatment with systemic methotrexate is an effective option in carefully selected, hemodynamically stable patients and is associated with success rates commonly reported between ~70% and 90% in appropriately selected cases. However, failure rates (and thus the need for subsequent surgical intervention) increase with higher initial serum β-hCG concentrations, larger ectopic size, the presence of embryonic cardiac activity, and if the patient presents late. Reported failure rates in the literature vary but may approach 10–30% depending on selection criteria and β-hCG thresholds. In our patient, incomplete clinical response to methotrexate prompted surgical resolution; this underscores the importance of close biochemical and sonographic follow-up when medical management is chosen and highlights that in settings where late presentation is common, surgical treatment will still comprise a substantial portion of cases.
9-11Salpingectomy is the preferred surgical approach for the management of EP, primarily because most EPs occur in the fallopian tubes, necessitating the removal of the affected tube to prevent complications such as rupture, severe hemorrhage, and recurrence.
22 This procedure involves the complete removal of the damaged fallopian tube, effectively resolving the ectopic gestation and minimizing the risk of persistent trophoblastic tissue. Salpingectomy is particularly advantageous when the contralateral tube is healthy, as it preserves overall fertility potential. Current evidence supports the advantages of laparoscopy over laparotomy for most tubal ectopic pregnancies in stable patients. Laparoscopic management is associated with reduced intraoperative blood loss, shorter operative times in experienced hands, decreased postoperative pain, shorter hospital stay and faster recovery, lower rates of adhesion formation, and potentially better subsequent reproductive outcomes compared with open surgery. These benefits have been demonstrated across observational studies and systematic reviews and explain why laparoscopy is considered the preferred approach in centers with adequate resources and trained personnel. Nevertheless, laparotomy remains indicated for patients presenting with massive hemoperitoneum, hemodynamic instability, or when advanced adhesions or extensive tubal damage preclude a safe minimally invasive approach.
9-11It is important to consider that this study has some limitations. As a single-center, retrospective study, the findings may not be generalizable to other healthcare settings or populations. Additionally, the lack of long-term follow-up data prevents an assessment of future fertility outcomes in patients who underwent surgical management. The study also focused exclusively on surgically managed ectopic pregnancies, limiting comparisons with cases treated medically or expectantly. Also, due to limitation in the available records it was not possible to determine whether the procedures were performed by laparoscopy or laparotomy. Further research, including multi-center prospective studies, is needed to provide a more comprehensive understanding of ectopic pregnancy management and its long-term implications.
This study has several limitations. As a single-center, retrospective study, the findings may not be generalizable to other healthcare settings or populations. The reliance on medical records introduces the potential for missing or incomplete data, which could impact the accuracy of reported clinical characteristics. Additionally, the study exclusively analyzed surgically managed ectopic pregnancies, limiting comparisons with cases treated medically or expectantly. The lack of long-term follow-up data prevents an assessment of reproductive outcomes or the recurrence of ectopic pregnancies. Lastly, while statistical analyses were conducted, the study design does not allow for causal inferences regarding risk factors or treatment efficacy.
This study determined a 4.4% prevalence of ectopic pregnancies requiring surgical intervention at
Hospital San Pablo from 2021 to 2023, with most cases involving women in their early thirties. Vaginal bleeding was the most common symptom, and right tubal implantation was the predominant site. Salpingectomy was the preferred treatment, highlighting its effectiveness in managing these cases. Early diagnosis and intervention remain crucial in reducing complications and improving outcomes. Further research is needed to explore alternative management strategies and their impact on reproductive health, contributing to a broader understanding of ectopic pregnancy care.
References1. Ilany K, Minneci M, Monjazeb R, Coiado OC. Overview of diagnosis, treatment, and innovation in ectopic pregnancy. Women's Health. 2023; 19: 17455057231160349.
2. Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020; 101 (10): 599-606.
3. Espínola Castiglioni GR. Ectopic pregnancy [Embarazo ectópico]. Rev Nac (Itauguá). 2012 Dec; 4 (2): 23-9. [access in 2024 Jul 14]. Available from: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2072-81742012000200004
4. Ministério da Saúde Pública e Bem-Estar Social (PY). National Manual of Standards of Care for Major Obstetric Pathologies [Manual Nacional de Normas de Atención de las Principales Patologías Obstétricas]. 1
st ed. Asunción: Ministério de Salud Pública y Bienestar Social; 2018. [access in 2024 Jul 14]. Available from: https://www.mspbs.gov.py/dependencias/progsalud/adjunto/b155f3-PatologiasObstetricascorregido.pdf
5. Andola S, Ramesh Kumar R, Desai RM, Krutika SA. Study of risk factors and treatment modalities of ectopic pregnancy. J Family Med Prim Care. 2021;10 (2): 724-9.
6. Buhur U, Unal O. Management of ectopic pregnancy in a tertiary hospital: a retrospective cohort study. Eur Rev Med Pharmacol Sci. 2023;27 (8): 3500-7.
7. Estrella P, Bustillos Solórzano ME. Update on ectopic pregnancy for primary health care [Actualización del embarazo ectópico para atención primaria de salud]. Arch Med. 2022; 24 (2). [access in 2024 Jul 14]. Available from: https://www.colegiomedicosazuay.ec/ojs/index.php/ateneo/article/view/232
8. Espinoza-Garita S, Garnier-Fernández JC, Pizarro-Alvarado G. Overview of ectopic pregnancy [Generalidades sobre embarazo ectópico]. Rev Med Sinerg. 2021; 6 (5). e670.
9. Hao HJ, Feng L, Dong LF, Zhang W, Zhao XL. Reproductive outcomes of ectopic pregnancy with conservative and surgical treatment: a systematic review and meta-analysis. Medicine (Baltimore). 2023; 102 (17): e33621.
10. Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009; 361 (4): 379-87.
11. Berhe ET, Kiros K, Hagos MG, Gesesew HA, Ward PR, Gebremeskel TG. Ectopic pregnancy in Tigray, Ethiopia: a cross-sectional survey of prevalence, management outcomes, and associated factors. J Pregnancy. 2021; 2021: 4443117.
12. Mokhtari Zanjani P, Ahmadnia E, Kharaghani R. Ectopic pregnancy rate in Iranian midwifery clients and infertile patients treated by assisted reproductive technologies. J Evid Based Med. 2019; 12 (1): 56-62.
13. Ntafam CN, Sanusi-Musa I, Harris RD. Intramural ectopic pregnancy: an individual patient data systematic review. Eur J Obstet Gynecol Reprod Biol X. 2023; 21: 100272.
14. Brim ACS, Barretto VRD, Reis-Oliveira JG, Silveira de Araújo RB, Romeo AC. Risk factors for ectopic pregnancy occurrence: systematic review and meta-analysis. Int J Gynaecol Obstet. 2025; 168 (3): 919-32.
15. Jensen RE, Martins N, Parks MM. Public perception of female fertility: initial fertility, peak fertility, and age-related infertility among U.S. adults. Arch Sex Behav. 2018; 47 (5): 1507-16.
16. Rahman MM, Tasnim J. Exploring the factors behind the shift in unwanted childbearing rate in Bangladesh between 2007 and 2017/2018: a cross-sectional study. BMJ Open. 2023; 13 (5): e069265.
17. Li H, Nawsherwan, Fan C, Nabi G, Ping YX. The trend in delayed childbearing and its potential consequences on pregnancy outcomes: a single-center 9-year retrospective cohort study in Hubei, China. BMC Pregnancy Childbirth. 2022;22: 514.
18. Jenabi E, Ayubi E, Khazaei S, Soltanian AR, Salehi AM. Environmental risk factors associated with ectopic pregnancy: an umbrella review. J Gynecol Obstet Hum Reprod. 2023; 52 (2): 102532.
19. Singh JK, Dangal G. Profile of ectopic pregnancy cases in a tertiary hospital. J Nepal Health Res Counc. 2021;19 (2): 327-30.
20. Talavera JIR, Parrill AM, Elsayad C, Fogel J, Riggs JC, Peng B. Association between ectopic pregnancy and inflammatory bowel disease, irritable bowel syndrome, and celiac disease: a systematic review. J Obstet Gynaecol Res. 2021; 47 (5): 1601-9.
21. Stabile G, Mangino FP, Romano F, Zinicola G, Ricci G. Ectopic cervical pregnancy: treatment route. Medicina (Kaunas). 2020; 56 (6): 293.
22. Morin A, Sideris M, Platts S, Palamarchuk T, Odejinmi F. A systematic review of ectopic pregnancy management and complications during the COVID-19 pandemic. In Vivo. 2022; 36 (4): 1570-9.
Authors' contributionInsfran G: conceptualization, methodology, formal analysis, writing—original draft, writing—review & editing, supervision.
Benítez B, Solaeche A and Nahomi Solís: Conceptualization, Methodology, Data curation, Investigation, Writing—original draft.
All authors approved the final version of the article and declare no conflicts of interest.
Data availabilityThe entire data set supporting the results of this study has been published in the article itself.
Received on June 17, 2024
Final version presented on September 23, 2025
Approved on September 24, 2025
Associated Editor: Alex Sandro Souza
 ; Bárbara Benítez2
; Bárbara Benítez2 ; Alejandra Solaeche3
; Alejandra Solaeche3 ; Nahomi Solís4
; Nahomi Solís4