ABSTRACT
OBJECTIVES: to synthesize preventive measures against listeriosis during pregnancy as presented in the scientific literature.
METHODS: a scoping review was conducted following the PRISMA-ScR guidelines. Articles were systematically searched in the PubMed/MEDLINE, SciELO, Web of Science, LILACS, and Scopus databases. Screening and data extraction were performed manually, with the support of the Rayyan® software.
RESULTS: of 449 articles initially identified, seven were included. The main preventive measures identified were educational interventions on risks and food safety practices, consistent with health authority recommendations. However, the literature also highlights significant challenges in effectively applying these measures, particularly in adapting them to specific social and cultural contexts.
CONCLUSIONS: health education remains the primary strategy for preventing listeriosis during pregnancy. Nevertheless, its effectiveness depends on integrated actions that address sociocultural barriers, regulatory frameworks, and systematic surveillance.
Keywords:
Listeriosis, Pregnancy, Prevention, Health education, Public health surveillance
IntroductionThe genus Listeria comprises five species of Gram-positive bacteria that primarily infect sheep, goats, and cattle.
1 However,
Listeria monocytogenes – and, in rare cases,
Listeria ivanovii – can also infect humans, primarily through the ingestion of contaminated food.
1Listeriosis usually presents with mild and self-limiting symptoms; however, this rule does not apply to pregnant women.
2 Indeed, pregnant women have up to a 100-fold higher risk of infection, with clinical manifestations that can even include severe complications such as septicemia and encephalitis.
3 Furthermore, the fetus is particularly vulnerable, with potential outcomes including miscarriage, growth restriction, and neonatal infection.
2,3Globally, listeriosis presents alarming epidemiological estimates.
4 Specifically, its fatality rate is estimated to range from 12% to 50% of cases, with many survivors experiencing sequelae such as ataxia and cranial nerve palsy, generating more than 150 disability-adjusted life years (DALYs).
4,5 However, in Brazil, epidemiological assessments of this condition remain scarce and superficial. Notably, most studies in the area stem from reports of local epidemics, which estimate the occurrence of more than 200,000 cases in specific contexts, but do not provide a real estimate of listeriosis incidence and prevalence.
6 This is likely attributable the fact that listeriosis is not a notifiable disease in Brazil, and there is no standardized surveillance protocol to evaluate it, even in pregnancy.
6Notwithstanding this scientific gap, prevention is considered the most effective strategy to control listeriosis.
4-6 This scoping review therefore aims to synthesize preventive measures against listeriosis in pregnancy as described in the scientific literature.
MethodsThis scoping review adheres to the PRISMA Extension for Scoping Reviews (PRISMA-ScR) guidelines.
7 The study objective was developed using the PICOS strategy, where "P" represents listeriosis in pregnancy; "I" denotes the prevention of this condition; "C" refers to the comparison of different preventive methods; "O" focuses on avoiding the development of listeriosis during pregnancy; and "S" includes literature reviews and protocol guidelines.
8 Accordingly, the following guiding question was formulated: "Which methods are presented by the scientific literature to prevent listeriosis in pregnancy?"
The search strategy employed Boolean operators with descriptors such as "Listeriosis AND Pregnancy AND Prevention" and "Listeriosis AND Pregnancy AND Preventive Measures." The search was conducted on March 27, 2025, across the PubMed/MEDLINE, SciELO, Web of Science, Latin American and Caribbean Health Sciences Literature (LILACS), and Scopus databases.
In addition, reference lists of relevant studies and guideline protocols were manually screened. Screening of titles, abstracts, and full texts was performed sequentially to include only articles that addressed the guiding research question. Rayyan
® software was utilized to facilitate and organize the review process.
9 Article selection was based on the inclusion and exclusion criteria outlined in Table 1.
Data extracted included information on the country of study, study design, journal, impact factor, study type, population assessed, proposed preventive measures, main results, and conclusions. Finally, no prior registration of this review protocol was made in PROSPERO.
ResultsThe initial search strategy yielded a total of 449 citations (Figure 1). After applying the predefined inclusion and exclusion criteria, seven articles met the eligibility criteria and were included in the final review.
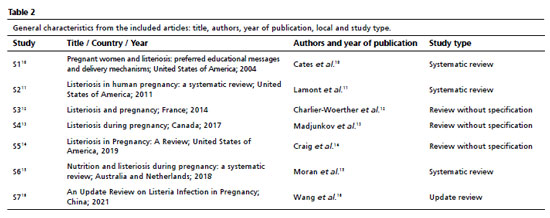
The characteristics of the selected studies are summarized in Tables 2 and 3. The majority of studies originated from the United States (S1, S2, S5), followed by contributions from Canada (S4), France (S3), Australia (S6), the Netherlands (S6), and China (S7). Most of the included articles were systematic reviews (S1, S2, S6), with publication dates ranging from 2004 to 2021.
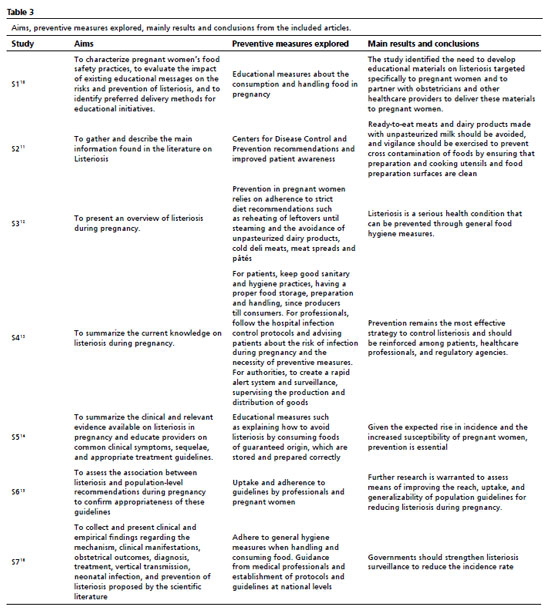
The preventive measures explored in the included studies predominantly emphasized educational interventions, particularly regarding food safety recommendations tailored to different cultural and regional contexts (S1 - S7). These measures focused on improving adherence to formal guidelines issued by health authorities, such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), which recommend avoiding high-risk foods, including unpasteurized dairy products, deli meats, smoked seafood, and refrigerated pâtés (S2,S4). Furthermore, several studies highlighted the importance of professional training for healthcare providers – including obstetricians, midwives, and dietitians – to effectively educate pregnant women about listeriosis risks, proper food storage, and safe food handling practices (S1, S3-S5, S7).
In addition to individual education, studies emphasized the role of public policies in enforcing preventive strategies that reflect local food consumption patterns and socio-economic realities (S1, S3, S4, S7). In some regions where traditional diets include unpasteurized dairy or fermented foods, public health campaigns need to be adapted to ensure cultural acceptability without compromising safety (S3, S6, S7). Moreover, the studies underscored the necessity of targeted interventions in vulnerable populations, such as women with limited access to healthcare or lower health literacy, who may require alternative communication strategies, including community-based outreach, multilingual materials, and digital health platforms (S2, S3, S6, S7).
Furthermore, enhanced surveillance systems were also identified as a crucial component of listeriosis prevention (S1, S2, S3, S4, S5). Studies called for more rigorous monitoring of food production chains, improved tracking of outbreaks, and stricter enforcement of food safety regulations to minimize contamination risks (S1, S2, S3, S4, S5). Specifically, strengthening rapid alert systems and ensuring timely responses to contamination events were highlighted as essential measures to reduce incidence rates (S1, S2, S3, S4, S5).
Finally, a multidisciplinary approach was deemed fundamental for effective prevention (S1 - S7). This includes collaboration between patients, healthcare professionals, food safety regulators, policymakers, and the food industry (S1 - S7). Obstetricians and nutritionists should work together to reinforce preventive behaviors among pregnant women, while regulatory agencies should partner with food producers to ensure compliance with safety standards (S1 - S7). Public health authorities must also engage with the media and educational institutions to develop campaigns that effectively communicate listeriosis risks and preventive actions to the general public (S1 - S7).
DiscussionChallengesThe studies included in this review highlighted several challenges in the practical implementation of listeriosis prevention strategies, particularly among pregnant women.
11,13,15,16Among the challenges mentioned, the lack of knowledge among pregnant women about the mode of transmission, risks, and preventive measures for listeriosis stands out.
10-12,17 Consequently, the studies highlight the need for effective educational campaigns, aimed at both pregnant women and healthcare professionals, so that they can act as agents of knowledge dissemination about this condition.
10-15,18Another relevant issue raised by the studies is the lack of standardization of preventive measures associated with listeriosis.
19,20 Namely, differences in infrastructure, resources, and methodological rigor adopted by different countries and industries lead to inconsistencies in recommendations and hinder practical and effective public health interventions.
19,20 Therefore, the authors argue for the creation of common supranational and interinstitutional protocols, whose guidelines must allow for adaptation to local and specific contexts.
20,21Educational InterventionsRather than merely recommending educational measures, the discussion focuses on how such measures can be implemented.
13,14,21 Consequently, many authors recommend using the guidelines and booklets created by the CDC and WHO as means of disseminating reliable information on the subject.
12-15,21 Accordingly, public campaigns involving the distribution of printed and digital materials to individuals, especially pregnant women, are recommended.
12.15 Despite existing obstacles to these actions – such as limited internet access in certain communities, low literacy levels, and language barriers – the development of multilingual educational resources, culturally adapted food safety campaigns, and the integration of listeriosis education into existing prenatal care protocols offer potential solutions to overcome them.
10,11,13,22Role of Healthcare ProfessionalsHealthcare professionals play a critical role in listeriosis prevention, as they serve as a trusted source of information for pregnant women.
10,13,23 Prenatal care visits provide an ideal setting for educating patients on food safety practices, the risks of listeriosis, and the importance of adhering to preventive guidelines.
11,13,23 Nevertheless, inconsistent access to prenatal care and the lack of sufficient training on foodborne disease prevention for healthcare providers may hinder these efforts.
14,16,24 In light of this, investing in continuing education for healthcare professionals, developing standardized counseling protocols, and incorporating food safety education into routine prenatal care are potential strategies to overcome these difficulties.
14,16,25Surveillance and RegulationEffective prevention is also contingent upon robust food safety regulations and surveillance systems.
13,17,26 Governments must enforce stricter control of high-risk foods, improve traceability, and ensure transparent communication with the public.
12-15,27 Enhanced surveillance, through mandatory case reporting, improved diagnostics, and real-time data sharing, is paramount to detect outbreaks and assess preventive measures.
13,15,27,28 International collaboration is essential to standardize surveillance and harmonize regulatory practices.
11,14,28Strengths and limitationsThe study's adherence to the PRISMA-ScR guidelines ensures a structured and transparent methodological approach. The use of the PICOS framework to define the research question enhances the clarity and precision of the study objectives. Furthermore, the comprehensive search strategy, which incorporated multiple databases and manual reference screening, increases the likelihood of capturing a broad range of relevant literature.
Conversely, the lack of prior registration in PROSPERO could impact the reproducibility of the study. Manual data extraction, while thorough, poses a risk of human error. Lastly, restricting the inclusion criteria to specific languages may have led to the exclusion of relevant studies published in other languages.
Future perspectivesFuture research should focus on rigorously evaluating the effectiveness of current preventive measures, exploring novel strategies for foodborne disease mitigation, and identifying socioeconomic determinants that influence adherence to guidelines.
10,13,29 By reinforcing preventive strategies and fostering international cooperation, public health authorities can mitigate the risks associated with listeriosis in pregnancy, thereby reducing maternal and neonatal morbidity and mortality.
11,29,30 Efforts should remain dynamic and adaptive to emerging evidence, to ensure that listeriosis prevention remains a priority in maternal health initiatives worldwide.
13,29,30ConclusionThis scoping review demonstrates that listeriosis prevention in pregnancy requires integrated and context-sensitive strategies. Health education remains essential, but its success is contingent upon culturally adapted approaches, qualified healthcare professionals, rigorous regulatory enforcement, and robust surveillance systems. Crucially, beyond synthesizing existing evidence, this review emphasizes the need for coordinated actions between clinical practice and public health policies to ensure effective prevention. Strengthening these strategies is crucial to reduce maternal and neonatal risks and to elevate listeriosis prevention as a priority in maternal health agendas
References1. Koopmans MM, Brouwer MC, Vázquez-Boland JA, van de Beek D. Human Listeriosis. Clin Microbiol Rev. 2023 Mar; 361: e0006019.
2. Khsim IEF, Mohanaraj-Anton A, Horte IB, Lamont RF, Khan KS, Jørgensen JS,
et al. Listeriosis in pregnancy: An umbrella review of maternal exposure, treatment and neonatal complications. BJOG. 2022; 129 (9): 1427-33.
3. Charlier C, Disson O, Lecuit M. Maternal-neonatal listeriosis. Virulence. 2020 Dec; 11 (1): 391-7.
4. de Noordhout CM, Devleesschauwer B, Angulo FJ, Verbeke G, Haagsma J, Kirk M, Havelaar A, Speybroeck N. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014 Nov; 1411: 1073-82.
5. Freitag IGR, Castro Lisbôa Pereira R, Machado ES, Hofer E, Vallim DC, Hofer CB. (2021). Prevalence of Listeria monocytogenes fecal carriers in HIV-infected and -uninfected pregnant women from Brazil. Braz J Microbiol. 2021; 52 (4): 2081–4.
6. Camargo AC, Moura A, Avillan J, Herman N, McFarland AP, Sreevatsan S,
et al. Whole-genome sequencing reveals Listeria monocytogenes diversity and allows identification of long-term persistent strains in Brazil. Environ Microbiol. 2019 Dec; 21 (12): 4478–87.
7. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D,
et al. PRISMA Extension for Scoping Reviews PRISMA-ScR: Checklist and Explanation. Ann Intern Med. 2018 Oct; 1697: 467-73.
8. Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study PICOS design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020 Jun; 376: 387.
9. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec; 51: 210.
10. Cates SC, Carter-Young HL, Conley S, O'Brien B. Pregnant women and listeriosis: preferred educational messages and delivery mechanisms. J Nutr Educ Behav. 2004; 363: 121-7.
11. Lamont RF, Sobel J, Mazaki-Tovi S, Kusanovic JP, Vaisbuch E, Kim SK,
et al. Listeriosis in human pregnancy: a systematic review. J Perinat Med. 2011 May; 393: 227-36.
12. Charlier-Woerther C, Lecuit M. Listériose et grossesse [Listeriosis and pregnancy]. Presse Med. 2014 Jun; 436 Pt 1: 676-82. [French]
13. Madjunkov M, Chaudhry S, Ito S. Listeriosis during pregnancy. Arch Gynecol Obstet. 2017; 296 (2): 143-52.
14. Craig AM, Dotters-Katz S, Kuller JA, Thompson JL. Listeriosis in Pregnancy: A Review. Obstet Gynecol Surv. 2019 Jun; 746: 362-8.
15. Moran LJ, Verwiel Y, Bahri Khomami M, Roseboom TJ, Painter RC. Nutrition and listeriosis during pregnancy: a systematic review. J Nutr Sci. 2018 Sep;7: e25.
16. Wang Z, Tao X, Liu S, Zhao Y, Yang X. An Update Review on Listeria Infection in Pregnancy. Infect Drug Resist. 2021 May; 14: 1967-78.
17. Chen L, Lu T, Yang D, Qin X, Huang L, Xu B,
et al. Clinical Outcome and Factors with Dietary Behaviors in Pregnant Women with Listeria monocytogenes: A Hospital-Based Case-Control Study in Shanghai. Foodborne Pathog Dis. 2024; 21 (7): 431-9.
18. Hu G, Yan W, Dong F, Li G, Zhang X, Li Q,
et al. Maternal-Fetal Listeriosis in China: Clinical and Genomic Characteristics From an ST8 Listeria monocytogenes Case. Infect Drug Resist. 2025; 18: 1313–24.
19. Camargo AC, Woodward JJ, Call DR, Nero LA. Listeria monocytogenes in Food-Processing Facilities, Food Contamination, and Human Listeriosis: The Brazilian Scenario. Foodborne Pathog Dis. 2017; 14 (11): 623–36.
20. Rizk J, Andreou E, Hileti D, Ghaddar A, Zampelas A. Nutrition knowledge among pregnant women in Lebanon: A cross-sectional study. Women's Health (Lond). 2024; 20: 17455057241272216.
21. Vallim DC, Barroso Hofer C, Lisbôa RC, Barbosa AV, Alves Rusak L, Reis CM,
et al. Twenty Years of Listeria in Brazil: Occurrence of Listeria Species and Listeria monocytogenes Serovars in Food Samples in Brazil between 1990 and 2012. Biomed Res Int. 2015; 2015: 540204.
22. Zhang Y, Zhang J, Chen J, Qi X, Zhang Z, Chen H,
et al. Sporadic Listeriosis Cases, Genotypic Characteristics, and Antibiotic Resistance of Associated Listeria monocytogenes Isolates in Zhejiang Province, China (2016-2022). Foodborne Pathog Dis. 2025; [
Online ahead of print].
23. Ooi KJ, Fenton S, Taylor R, Hutchesson MJ, Hinwood M, Collins C. The Relationship Between Potential Listeria monocytogenes Exposure and Diet Quality and Dietary Intake During Pregnancy: A Cross-Sectional Analysis in Australian Women. J Hum Nutr Diet. 2025; 38 (2): e70032.
24. Cavalcanti AAC, Limeira CH, Siqueira IN, Lima AC, Medeiros FJP, Souza JG,
et al. The prevalence of Listeria monocytogenes in meat products in Brazil: A systematic literature review and meta-analysis. Res Vet Sci. 2022; 145: 169–76.
25. Braga V, Vázquez S, Vico V, Pastorino V, Mota MI, Legnani M,
et al. Prevalence and serotype distribution of Listeria monocytogenes isolated from foods in Montevideo-Uruguay. Braz J Microbiol. 2017; 48 (4): 689–94.
26. Księżak E, Sadkowska-Todys M. Listeriosis in Poland in 2012-2021. Listerioza w Polsce w latach 2012-2021. Przegl Epidemiol. 2024; 77 (4): 531–43.
27. Niu Y, Li W, Xu B, Chen W, Qi X, Zhou Y,
et al. Risk factors associated with food consumption and food-handling habits for sporadic listeriosis: a case-control study in China from 2013 to 2022. Emerg Microbes Infect. 2024; 13 (1): 2307520.
28. Gianecini RA, Cipolla L, Rocca F, Campos J, Poklepovich T, Prieto M. (2024). Caracterización molecular de aislamientos de Listeria monocytogenes de origen humano y alimentario en Argentina, 2018-2023. Rev Argentina Microbiol. 2024; 56 (3): 329–35.
29. Vázquez E, Gregorio Ó, Soriano V, Álvarez C, Ortega-de la Puente A., de la Cruz-Echeandía M,
et al. (). Pregnancy-related listeriosis in Spain. J Infect Public Health. 2025; 18 (5): 102706.
30. Figueroa Y, Gentiluomo J, Grisaro A, Buffoni M, Zipenco N, Sucari A,
et al. Estudio epidemiológico y serotipificación por PCR múltiple de Listeria monocytogenes aislada de matrices alimentarias en Argentina. Rev Argentina Microbiol. 2023; 55 (4): 387–94.
Author's contributionThe author conceived the article and declared no conflicts of interest.
Data AvailabilityAll datasets supporting this study are present in the article.
Received April 29, 2024
Final version presented on October 1, 2025
Approved on October 2, 2025
Associated Editor: Priscila Onofre
