ABSTRACT
OBJECTIVE: to estimate the prevalence of HIV and syphilis, and their association with gestational complications and newborn outcomes in women admitted for delivery at a mother and child center in the South of Brazil.
METHODS: cross-sectional study based on the review of electronic medical records of parturients (March/2016 to June/2018). Sociodemographic and clinical data were analyzed. HIV and syphilis were considered outcomes, then exposures to assess associations with pregnancy and neonatal variables. Prevalence Ratio (PR) were calculated using Poisson Regression with robust variance and 95% Confidence Interval (CI).
RESULTS: data from 6,527 women were evaluated. HIV prevalence was 0.6% and syphilis 1.5%. Women assisted by the public health system [PR=2.28 95%CI=1.07-4.82 for syphilis; PR=3.52 95%CI=1.06-11.72 for HIV] and drug users [PR=5.47 95%CI=2.49-12.04 for syphilis; PR=4.76 95%CI=1.12-20.19 for HIV] were more affected. Syphilis was more prevalent among younger and non-white women (p=0.001). Adequate prenatal care reduced syphilis by 38% (PR= 0.62 95%CI=0.39-0.97; p=0.006). Neonatal complications occurred in 32.3% of syphilis cases and 17.1% of HIV cases. Of the 98 syphilis cases, 29.6% led to congenital syphilis.
CONCLUSION: women in socially vulnerable conditions, such as drug users, were more affected. Congenital syphilis exceeded the national average, reinforcing the need for timely and comprehensive prenatal care.
Keywords:
Syphilis, HIV seropositive, Congenital syphilis, Sexually transmitted diseases, High-risk pregnancy
IntroductionIn view of the advances in world health in recent years, care for Syphilis and HIV has also evolved and reached a greater proportion of the population. However, Sexually Transmitted Infections (STIs) continue to rise in alarming levels.
1Among the affected populations, pregnant women stand out. In 2020, 800 women died daily from preventable causes related to pregnancy and childbirth, with emphasis on infectious diseases that during the gestational period play an important role in increasing the risk of maternal and fetal mortality.
2,3Congenital syphilis and HIV are communicable and preventable conditions with potential for vertical transmission. Both can be effectively controlled through timely diagnosis and appropriate treatment during the pre-gestational and gestational periods. However, failures in prenatal care—such as limited access, late initiation, or inadequate follow-up—may hinder prevention.
4,5 In the case of HIV, additional factors such as poor adherence to antiretroviral therapy, breastfeeding, and premature birth further increase the risk of fetal transmission.
6The correlation between Syphilis and HIV permeates the characterization of both STIs with vertical transmission and they are together with the scenario that facilitates infections and vulnerability that this population presents, with emphasis on pregnant women, who become twice as susceptible to contagion as the population in general.
7,8The identification of women exposed to risk factors is one of the main components for seeking prevention strategies. Nevertheless, sociodemographic, economic, and behavioral factors guide the characterization of female social vulnerability to STIs, and understanding the factors related to these infections is essential for their prevention.
1In addition, the implications of the occurrence of STIs such as HIV and Syphilis in the gestational period are still poorly explored in the national literature.
7 Understanding that many risk factors for maternal-fetal health are related to barriers encountered in prenatal care, it is important to characterize the complications encountered in the postpartum period.
In this sense, the objective of this study was to estimate the prevalence of HIV infection and/or syphilis and their association with gestational complications and newborn characteristics of the parturient women admitted to a mother and child center in the South of Brazil.
MethodsThe present study has an observational, cross-sectional design. The studied population consisted of parturients admitted for pregnancy resolution at the
Nossa Senhora da Conceição Mother and Child Center (HNSC), in the city of Tubarão/SC, from March 2016 to June 2018. On average, three thousand births occur annually in this maternity hospital, which is a reference for high-risk pregnancies for the entire region of South Santa Catarina State, Brazil. The maternal and child center encompasses an obstetric center, human milk bank, rooming-in space, and neonatal intensive care unit. It is a philanthropic hospital that provides services to the
Sistema Único de Saúde (SUS) (Brazilian Public Health System).
Based on a database belonging to the integrated project "Cesarean section rates according to Robson's classification: Evaluation of the implementation of the adequate childbirth project in a hospital in the South of Brazil"
9, parturient women admitted to the maternity hospital during the study period, in order to identify pregnant women diagnosed with HIV or syphilis were included. Hospitalized patients who did not have information regarding the diagnosis of HIV or syphilis were excluded.
The data required for the study were collected from the electronic medical record (Tasy
®), a standard tool used to record medical care at the service. Sociodemographic data such as age, marital status, schooling, skin color, and clinical data were obtained, such as gestational history, prenatal care, HIV diagnosis, syphilis diagnosis, type of delivery, adverse event or unfavorable outcome (maternal death, maternal Intensive Care Unit (ICU) admission, intrapartum fetal death and neonatal ICU admission), abortion, birth status, prematurity (gestational age <37 weeks), breastfeeding within the first hour, skin-to-skin contact, newborn (NB) weight, being considered low weight when below 2,500g, and complications after birth (use of oxygen by the NB, perinatal asphyxia, Toc-traumatism, use of mechanical ventilation, hospitalization and performance of the hypothermia protocol for the NB). In cases of twin pregnancy or corresponding to more than one pregnancy during the research period, they were considered only once, with no duplication of information. Data were collected via hospital records, and it was not possible to identify when the diagnosis was made, whether it was made during hospital admission or previously.
The database was structured in a Microsoft Excel spreadsheet. Data were analyzed using SPSS version 26.0. Descriptive statistics were initially used, using measures of absolute and relative frequency (%) and measures of central tendency and data dispersion. Comparisons between groups were tested using the Chi-Square test and Student's t test, or non-parametric correspondents, according to the adequacy of data normality. Initially, the prevalence of HIV and syphilis diseases were the outcome variables of the study, with maternal factors associated with their occurrence being verified. Subsequently, the presence of diseases was considered as an exposure factor to assess the relationship with other pregnancy and newborn outcomes. The association measure used was the Prevalence Ratio (PR), adjusted by Poisson regression with robust variance, with a confidence interval (CI) of 95% and a level of statistical significance of 5%. The adjustment models were carried out considering variables of epidemiological importance, such as age and schooling, besides the statistical criteria of
p<0.20 in bivariate analysis, according to the outcome of interest. To test the association between maternal and gestational variables and the outcomes of HIV and syphilis, PR was adjusted for the mother's age, schooling, race/skin color and marital status. To verify the association of HIV and syphilis with other pregnancy and newborn outcomes, first model considered age and schooling, and the second considered: age, schooling
, race/skin color, marital status, SUS delivery and drug use.
The main project for which data from medical records were collected was approved by the Research Ethics Committee (CEP) of the
Universidade do Sul de Santa Catarina (UNISUL) with opinion no. 3.215.923, of March 2019. This research was approved with opinion no. 4.875.730, of July 2021.
ResultsOf the 6,670 births evaluated at the
Nossa Senhora da Conceição Maternity Hospital, from March 2016 to June 2018
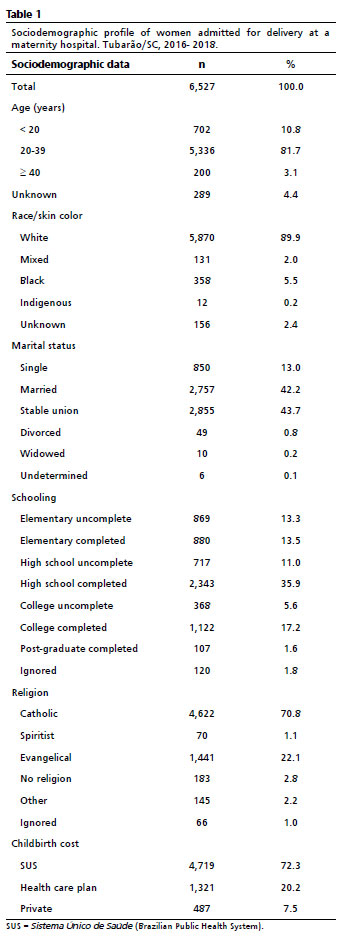
, there were 143 multiple pregnancies (2 triplets and 141 twins), resulting in 6,527 women evaluated. Regarding epidemiological data, 89.9% of the patients were white, 43.7% were in a stable relationship and 35.9% had completed high school; 72.3% of births were performed via SUS. The mean age was 27.5 years (SD + 6.4) years, ranging from 13 to 48 years, median 27 years, and the most prevalent age group was 20-39 years, with 81.7% (Table 1).
Of the total number of pregnant women, 41.4% were primiparous and 22.2% had a history of previous abortion, with up to six episodes recorded. The median gestational age at birth was 38.5 weeks, ranging from 20 to 44 weeks of gestation. Prenatal care was performed by 96% of the participants, however, in 70% of the assessed records, the place where it was performed did not appear. It was found that 79% of pregnant women had at least six prenatal consultations as recommended by the Brazilian Ministry of Health (data not shown).
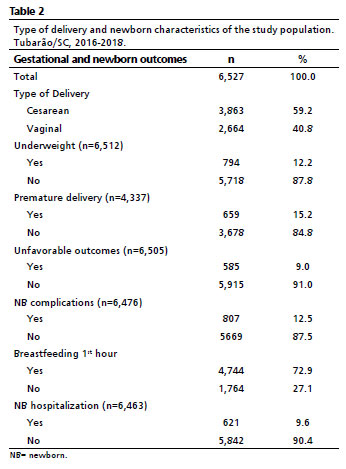
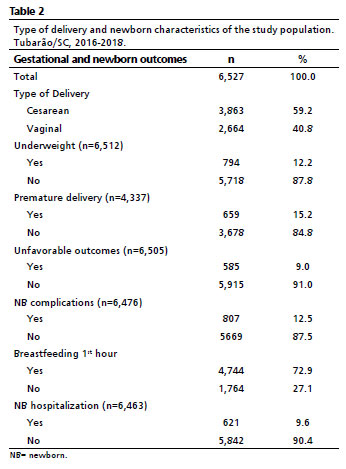
Regarding childbirth and newborn characteristics (Table 2), 59.2% of the deliveries were by cesarean section. Low birth weight was observed in 12.2% of the newborns. Among deliveries with gestational age (GA) estimated by the date of the last menstrual period (n = 4,338), 659 preterm births were recorded, representing 15.2%. Nine (9) percent of the births had some unfavorable outcome. There were two intrapartum fetal deaths and 140 admissions to the neonatal ICU (2.1%).
Eight women had no information about HIV occurrence, this disease was recorded in 41 of 6,519 women (0.6%). A higher prevalence was verified among with less schooling, non-primiparous women who reported drug use, had no association between the prevalence of the disease and the variables of age and ethnicity. Women with higher schooling constitute a 50% smaller proportion in relation to the other participants (Table 3). Married women had a 60% lower prevalence of the disease. Furthermore, HIV prevalence was 3.5 times higher among pregnant women assisted by SUS (
p=0.01), and over 4 times higher among those who reported drug use.
Syphilis represented a prevalence of 1.5%, being registered in 98 of 6,524 women with a valid data for this variable. The prevalence of syphilis was higher in younger women, less than 20 years old (
p=0.001). Ethnicity had a significant relationship with positive syphilis cases, being 45% lower in white women (
p=0.001). Married women with high schooling had a lower prevalence of the disease, as well as patients who underwent prenatal care as recommended, demonstrating that having at least six prenatal consultations reduced the occurrence of syphilis during pregnancy by 38% (
p=0.006). The prevalence of syphilis was higher among women assisted by SUS (PR=2.28; 95%CI=1.07–4.82) and among those who reported drug use (PR=5.74; 95%CI=2.49–12.04).
It was found that the diagnosis of HIV and syphilis was concomitant in 12 of the pregnant women, corresponding to 0.18% of the total number of women. Among HIV cases, 29.3% also had positive syphilis, compared to 1.3% of syphilis among women who do not have HIV (
p<0.001).
Tables 4 and 5 demonstrate the analysis of other gestational outcomes that could be related to the presence of diseases. Among women with HIV, 75.6% underwent cesarean delivery, in contrast to 59.1% of those without the disease. Yet, among women with syphilis, the highest frequency was vaginal delivery (51%) than cesarean section.
The analysis shows that patients with HIV had a history of previous abortion of 35.5%, compared to 27.5% in those without this condition, however without significant differences (PR=1.29 and 95%CI=0.80-2.08). On the other hand, syphilis cases had a higher frequency of previous miscarriages (44.3% versus 27.4%;
p=0.003). Of the 98 registered syphilis cases, 29.6% led to congenital syphilis cases.
In an adjusted analysis, cesarean delivery was positively associated with HIV during pregnancy, while the presence of the disease was a limiting factor for breastfeeding in the 1
st hour of life and exclusively during hospitalization. In contrast, syphilis, was positively associated with complications with the NB, and negatively associated with exclusive breastfeeding.
DiscussionIn this study, which analyzed medical records of over 6,000 women during childbirth care in a maternity hospital in the South of Brazil, the prevalence of syphilis was estimated at 1.5% and HIV infection at 0.6%. An association was found between social vulnerability factors and a higher risk of infection, such as being assisted by SUS and those who reported drug use. The presence of these infections during pregnancy was associated with cesarean deliveries and lower occurrence of breastfeeding in HIV cases, and with neonatal complications and hospitalization in cases of syphilis.
In a systematic review, the global pooled prevalence of syphilis was 0.8% (95%CI=0.7–0.9) and of HIV, 2.9% (95%CI=2.4–3.4), with both infections showing higher prevalence in low-income and lower-middle-income countries compared to the global average.
8 An analysis of the national
Sistema de Informação de Agravos de Notificação (Sinan) (Notifiable Diseases Information System) for syphilis, with data specific to pregnant women, indicated an incidence of 22.3 cases per 1,000 live births (2.23%) in 2020. Regarding HIV notifications among women of reproductive age, an incidence of 12.3 cases per 1,000 women (approximately 1.23%) was identified in the same year.
10 In an analysis of more than 15 million births in Brazil, linking data from two national information systems, Sinan and
Sistema de Informação sobre Nascidos Vivos (Sinasc) (Brazilian Live Births Information System), the proportion of maternal syphilis was 0.91%.
11Variations in frequency rates may be related to differences in disease detection methods and case reporting practices, as well as to sociodemographic factors, particularly those affecting access to prenatal care and diagnostic testing.
11,12 This study was conducted in a city located in the state of Santa Catarina, in the South region of Brazil, which is nationally recognized as an HIV ‘hot spot' and also reports syphilis detection rates above the national average.
13 An analysis of the
Pesquisa Nacional de Saúde (PNS) (Brazilian National Health Survey) (2013 and 2019) showed an increase in the number of syphilis (21%) and HIV (4%) tests performed during prenatal care over the period. The South region recorded the highest prevalence of testing.
12 It is also important to highlight that, while annual HIV detection rates in Brazil have remained relatively stable over the past ten years, maternal syphilis rates have increased exponentially.
13The pattern of co-infection between HIV and syphilis is a common finding, also verified in this study. The analysed groups present a predominance of social vulnerability factors, such as low educational level, delivery through SUS, and drug use. Sometimes, the low educational level is associated with economic characteristics and limitations of access to health, being considered a predictor of the use of SUS, as it indicates the women's lack of conditions to afford private services.
4,11,12,14-16The fact that women who use drugs have a higher prevalence of syphilis and HIV is in line with other studies.
4,17-19 The increase in STIs in this group is attributed to the risks that this lifestyle offers, due to the loss of the power of judgment and consequently, the increase in unprotected sexual activities and multiple partners.
16,20 In addition, drug use is also responsible for an increase in vertical transmission, a reduction in prenatal care and prevention failures.
6Among the epidemiological aspects evaluated, women with syphilis represented mostly a group of non-white women, with low schooling and single, a pattern similar to other studies.
4,11,12,17,21 As for the most affected age group among pregnant women with syphilis, those under 20 years of age stand out, with a prevalence of up to four times greater of the disease. In a Brazilian study, women aged 20 to 29 years were the most affected age group for both infections during the study period.
10 This discrepancy between the findings can be explained by the rising of a new risk group for syphilis, more evident from the year 2011, when an inversion of the age profile began.
22,23 A study carried out in the city of São Paulo showed that the increase in cases of gestational syphilis is directly influenced by cases of teenage pregnancy.
15 The group in question is evidently fragile, having mostly an unplanned pregnancy and unprotected sexual practice, it is necessary to promote approaches whenever this public has access to health services.
4,22The predominant pattern among HIV-positive pregnant women is of less educated and non-primigravid women. For Cambou
et al.,
13 education was also an important factor, with only 21.3% of pregnant women with HIV having a high schooling level. Regarding age and ethnic classification, the Ministry of Health shows a predominance among young women (20 - 24 years old) and mixed race.
23 However, this statistical analysis did not find an association of HIV prevalence with age and ethnicity.
In Brazil, prenatal care is free and universally accessible to all women, by SUS.
5 Access to at least six prenatal consultations—a minimum recommended by the Brazilian Ministry of Health—has been consistently associated with improved syphilis detection and management during pregnancy.
5,13,22,23 In this study, among women who had six or more consultations there was a 38% reduction in the occurrence of Syphilis. In the Federal District in Brazil, a real-time monitoring plan for prenatal visits led to a 37% reduction in congenital syphilis incidence within two years, following the implementation of improved care strategies.
24 It is important to note that the quality of care offered is sometimes not what was expected, especially for women with low socioeconomic status.
11 In addition, the late beginning of prenatal care occurs in about 40% of women and less than 30% perform the second test requested, which puts the woman and the fetus at risk, increasing the possibility of unfavorable neonatal outcomes.
22,23More unfavorable outcomes and complications after birth were seen in patients with gestational syphilis. Women with syphilis are prone to a greater number of gestational complications than women in general.
4,14 This is due to the high vertical contamination of
Treponema pallidum, which not only causes congenital syphilis but also compromises fetal growth and can cause prematurity, low birth weight, and stillbirths.
5,22,25,26 Usually, such events are seen in those pregnant women who are victims of the process of misdiagnosis, non-treatment, or incorrect treatment of themselves and their partners, which is a major impediment found in the process of reducing vertical transmission of syphilis.
23 Due to these characteristics, the diagnosis of syphilis is considered a predictor of the quality of prenatal care.
4,16,17,22The diagnosis of congenital syphilis was performed in 29.6% of newborns born to mothers with gestational syphilis, however, it is not known how the diagnosis was established, if all newborns were correctly tested or if they came to present late syphilis cases. The results found are above the national average, which was 0.9% in 2023 (i.e. 9.0 cases per 1,000 live births).
23 This finding suggests possible ineffectiveness in syphilis treatment during pregnancy in the present study, since congenital infection occurs in less 2% of adequately treated women during pregnancy.
5,27The number of complications and unfavorable outcomes related to mothers with HIV was lower when compared to the impact of syphilis. However, regarding prematurity, the prevalence was higher among children born to mothers with HIV (16.7%), compared to those born to mothers with syphilis (10.3%), despite the fact that, according to the literature, syphilis is directly linked to prematurity.
17,26 The number of previous abortions was higher among women with syphilis than among those with HIV. However, it is not possible to establish a direct causal relationship, as there are no data on the timing of infection or diagnosis, Still, the fact that syphilis increases the number of cases of spontaneous abortions is known, and the history of abortion is also associated with pregnant women with the disease.
4,5,17,26In Brazil, vaginal delivery is not contraindicated for women with HIV if their viral load is within recommended limits.
5 In this study, 24.4% of women with HIV had vaginal deliveries, but it was not possible to verify whether their viral loads were within the recommended range.
The Ministry of Health advises that women with HIV should not breastfeed, as HIV transmission can still occur via breastmilk, even when the viral load is undetectable.
5 In this study, breastfeeding was 70% less frequent among women with HIV compared to those without, yet it still occurred, suggesting that suppression strategies may be insufficient and placing newborns at risk.
Therefore, breastfeeding guidance should begin during prenatal care, preparing women for safe alternatives and reducing the risk of vertical transmission to below 2% when appropriate interventions are implemented.
5,6 Conversely, offering such guidance only in the postpartum period may reduce adherence and lead to less satisfactory outcomes.
5Among the limitations of the study, the use of secondary data may have introduced inconsistencies or missing information, particularly regarding timing of diagnosis, treatment details, and disease stage. Additionally, abortion data reflect maternal history without enabling causal attribution to HIV or syphilis. As a cross-sectional study, causal relationships cannot be established.
In conclusion, HIV prevalence was 0.6%, higher in single women, drug users, and who gave birth at SUS. HIV was associated with higher rates of cesarean delivery and lower breastfeeding frequency. Syphilis prevalence reached 1.5%, being lower in women with higher schooling, white, married, and with ≥6 prenatal visits, and with a higher occurrence in drug users and being SUS patients. The presence of the disease increased the frequency of complications in NBs, reduced exclusive breastfeeding during hospitalization, higher miscarriages rates and a frequency of congenital syphilis above the national average, reinforcing the need for timely and comprehensive prenatal care.
References1. Davis R, Xiong X, Althabe F, Lefante J, Cafferata ML, Mwenechanya M,
et al. Factors associated with HIV and syphilis screenings among pregnant women at first antenatal visit in Lusaka, Zambia. BMC Res Notes. 2020 Sep; 13 (1): 423.
2. Sebastião CS, Neto Z, Jandondo D, Mirandela M, Morais J, Brito M. HIV, hepatitis B virus, hepatitis C virus, and syphilis among pregnant women attending antenatal care in Luanda, Angola: Seroprevalence and risk factors. J Med Virol. 2020 Dec; 92 (12): 3265-70.
3. United Nations. Sustainable Development Goals, Goal 3: Ensure healthy lives and promote well-being for all at all ages [
Internet]. United Nations Sustainable Development. [access in 2025 Jul 17]. Available from:
https://www.un.org/sustainabledevelopment/health/4. Benedetti KCSV, Ribeiro ADC, Queiroz JHFS, Melo ABD, Batista RB, Delgado FM,
et al. High Prevalence of Syphilis and Inadequate Prenatal Care in Brazilian Pregnant Women: A Cross-Sectional Study. Am J Trop Med Hyg. 2019 Oct;101(4):761–6.
5. Ministério da Saúde (BR). Protocolo Clínico e Diretrizes Terapêuticas para Prevenção da Transmissão Vertical do HIV, Sífilis e Hepatites Virais. Brasília (DF): Ministério da Saúde; 2022. [access in 2024 Sep 15] Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_hiv_sifilis_hepatites.pdf6. Cardenas MC, Farnan S, Hamel BL, Mejia Plazas MC, Sintim-Aboagye E, Littlefield DR,
et al. Prevention of the Vertical Transmission of HIV; A Recap of the Journey so Far. Viruses. 2023 Mar; 15 (4): 849.
7. Menegotto M, Magdaleno AM, Silva CLO, Friedrich L, Silva CH. Mother-to-Child HIV Transmission among Pregnant Women in a City with the Highest Rates of HIV in Brazil. Am J Perinatol. 2022 Oct; 39 (13): 1418–25.
8. Wu S, Wang J, Guo Q, Lan H, Sun Y, Ren M,
et al. Prevalence of human immunodeficiency virus, syphilis, and hepatitis B and C virus infections in pregnant women: a systematic review and meta-analysis. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2023 Aug; 29 (8): 1000–7.
9. D'Agostini Marin DF, Rosa Wernke A, Dannehl D, Araujo D, Koch GF, Marçal Zanoni K,
et al. The Project Appropriate Birth and a reduction in caesarean section rates: an analysis using the Robson classification system. BJOG Int J Obstet Gynaecol. 2022 Jan; 129 (1): 72–80.
10. Santos BNS, Araújo FG, Paula TF, Matozinhos FP, Felisbino-Mendes MS. Prevalence of preconception health indicators among Brazilian women of reproductive age. Ciênc Saúde Colet. 2023 Nov; 28: 3367-81.
11. Paixao ES, Ferreira AJF, Pescarini JM, Wong KLM, Goes E, Fiaccone R,
et al. Maternal and congenital syphilis attributable to ethnoracial inequalities: a national record-linkage longitudinal study of 15 million births in Brazil. Lancet Glob Health. 2023 Nov; 11 (11): e1734–42.
12. Freitas FMS, Correia RDGCF, Biazus-Dalcin C, Jorge HMF, Aquino PS, Oliveira BLCA. Prenatal tests in Brazil: prevalence and associated factors according to the Brazilian National Health Survey. Rev Esc Enferm USP. 2025; 58: e20240154.
13. Cambou MC, Saad E, McBride K, Fuller T, Swayze E, Nielsen-Saines K. Maternal HIV and syphilis are not syndemic in Brazil: Hot spot analysis of the two epidemics. PLOS ONE. 2021 Aug; 16 (8): e0255590.
14. Kengne-Nde C, Anoubissi JD, Loni-Ekali G, Nguefeu-Nkenfou C, Moussa Y, Messeh A,
et al. Highlighting a population-based re-emergence of Syphilis infection and assessing associated risk factors among pregnant women in Cameroon: Evidence from the 2009, 2012 and 2017 national sentinel surveillance surveys of HIV and syphilis. PLOS ONE. 2020 Nov 13; 15 (11): e0241999.
15. Medeiros JAR, Yamamura M, Silva ZP, Domingues CSB, Waldman EA, Chiaravalloti-Neto F. Spatiotemporal dynamics of syphilis in pregnant women and congenital syphilis in the state of São Paulo, Brazil. Sci Rep. 2022 Jan; 12 (1): 585.
16. Freitas CHSM, Forte FDS, Roncalli AG, Galvão MHR, Coelho AA, Dias SMF. Factors associated with prenatal care and HIV and syphilis testing during pregnancy in primary health care. Rev Saúde Pública. 2019 Sep; 53: 76.
17. Torres RG, Mendonça ALN, Montes GC, Manzan JJ, Ribeiro JU, Paschoini MC. Syphilis in Pregnancy: The Reality in a Public Hospital. Rev Bras Ginecol Obstet. 2019 Feb; 41 (2): 90-6.
18. Simões LA, Mendes JC, Silveira MR, Costa AMGD, Lula MD, Ceccato MDGB. Fatores associados à coinfecção HIV/sífilis no início da terapia antirretroviral. Rev Saúde Pública. 2022 Jun; 56: 59.
19. Haider MR, Kingori C, Brown MJ, Battle-Fisher M, Chertok IA. Illicit drug use and sexually transmitted infections among young adults in the US: evidence from a nationally representative survey. Int J STD AIDS. 2020 Nov; 31 (13): 1238-46.
20. Trivedi S, Williams C, Torrone E, Kidd S. National Trends and Reported Risk Factors Among Pregnant Women With Syphilis in the United States, 2012–2016. Obstet Gynecol. 2019 Jan; 133 (1): 27.
21. Neto PLF, Fonseca RRS, Avelino MES, Vilhena EM, Barbosa MAAP, Lopes CAF,
et al. Prevalence and Factors Associated With Syphilis in People Living With HIV/AIDS in the State of Pará, Northern Brazil. Front Public Health. 2021; 9: 646663.
22. Bezerra MLMB, Fernandes FECV, Nunes JPO, Baltar SLSMA, Randau KP. Congenital Syphilis as a Measure of Maternal and Child Healthcare, Brazil. Emerging Infectious Diseases. 2019; 25 (8): 1469-76.
23. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde e Ambiente. Boletim Epidemiológico Sífilis 2024. Número Especial. Brasília (DF): Ministério da Saúde [
Internet]. [access in 2025 Jul 17]. Available from:
https://www.gov.br/aids/pt-br/central-de-conteudo/boletins-epidemiologicos/2024/boletim_sifilis_2024_e.pdf24. World Health Organization (WHO). Eliminating congenital syphilis: using evidence-based management in Brazil. Geneva: WHO; 2024 [
Internet]. [access in 2025 Jul 17]. Available from:
https://www.who.int/news/item/20-12-2024-eliminating-congenital-syphilis--using-evidence-based-management-in-brazil25. Lim J, Yoon SJ, Shin JE, Han JH, Lee SM, Eun HS,
et al. Outcomes of infants born to pregnant women with syphilis: a nationwide study in Korea. BMC Pediatr. 2021 Jan; 21 (1): 47.
26. Shava E, Moyo S, Zash R, Diseko M, Dintwa EN, Mupfumi L,
et al. Brief Report: High Rates of Adverse Birth Outcomes in HIV and Syphilis Coinfected Women in Botswana. JAIDS J Acquir Immune Defic Syndr. 2019 Aug; 81 (5): E135-40.
27. Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I,
et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep. 2021 Jul; 70 (4): 1-187.
Authors' contributions: Almeida K, Silva LL, Marin DFD, Iser BPM were responsible for the conception and design of the study. Almeida K, Silva LL, Almeida BAO were responsible for the literature review and first version of writing, collection, analysis and interpretation of data. Iser BPM and Marin DFD participated in data analysis and interpretation and relevant critical review of intellectual content. All authors approved the final version of the article and declare that there is no conflict of interest.
Data Availability: The entire data set supporting the results of this study has been published in the article itself.
Received on October 14, 2024
Final version presented on July 17, 2025
Approved on July 24, 2025
Associated Editor: Aurélio Costa
 ; Luana Lima da Silva2
; Luana Lima da Silva2 ; Beatriz Aparecida Oliveira de Almeida3
; Beatriz Aparecida Oliveira de Almeida3 ; Daniela Ferreira D'Agostini Marin4
; Daniela Ferreira D'Agostini Marin4 ; Betine Pinto Moehlecke Iser5
; Betine Pinto Moehlecke Iser5