ABSTRACT
OBJECTIVES: to identify whether the presence of a partner is a protective factor for a longer duration of exclusive breastfeeding (EBF) of women living in João Pessoa and assisted by the Public Health System.
METHODS: cohort with pregnant women recruited from health services and followed up at their homes. Socioeconomic and demographic information, information on prenatal care, childbirth, puerperium care and baby nutrition were collected. Median EBF was calculated by survival analysis, Kaplan-Meyer, with log-rank test for group comparison. The independent EBF factors were estimated with multiple Cox regression. A 5% significance level was considered.
RESULTS: 162 women and their children were assessed. The median EBF was 120 days. Until the first four months of postpartum, women with a partner had longer EBF (p=0.002). In the final model, "having received prenatal guidance" (HR= 1.67; 95%CI= 1.05 - 2.65), "not having difficulty in breastfeeding after hospital discharge" (HR= 1. 58; 95%CI= 1.03 - 2.42) and "not using a pacifier" (HR= 1.64; 95%CI= 1.07 - 2.53) favored longer EBF duration.
CONCLUSION: encouraging partner's support for longer periods may be a viable strategy for improving EBF. Promotional actions and not offering pacifiers are important for a longer duration of EBF, and support and management in the puerperium period needs to be strengthened.
Keywords:
Breastfeeding, Maternal and child health, Cohort studies
RESUMO
OBJETIVOS: identificar se a presença do companheiro favorece maior duração do aleitamento materno exclusivo (AME) de mulheres residentes em João Pessoa assistidas pelo Sistema Único de Saúde.
MÉTODOS: coorte com gestantes recrutadas nos serviços de saúde e acompanhadas nos seus domicílios. Coletou-se informações socioeconômicas, demográficas, sobre pré-natal, parto, cuidados no puerpério e alimentação do bebê. Mediana do AME foi calculada por análise de sobrevivência, Kaplan-Meyer, com teste log-rank para comparar grupos. Estimou-se os efeitos independentes dos fatores relacionados com AME com regressão múltipla de Cox. Considerou-se 5% de nível de significância.
RESULTADOS: foram acompanhadas 162 mulheres e seus filhos. Mediana do AME foi 120 dias. Até os primeiros quatro meses pós-parto, mulheres com companheiro tiveram maior duração do AME (p=0,002). No modelo final, "ter recebido orientações no pré-natal" (HR= 1,67; IC95%= 1,05 – 2,65), "não ter tido dificuldade para amamentar após a alta hospitalar" (HR: 1,58; IC95%= 1,03 – 2,42) e "não usar chupeta" (HR= 1,64; IC95%= 1,07 – 2,53) favoreceram maior duração do AME.
CONCLUSÃO: o apoio prolongado do companheiro pode ser uma estratégia viável para a melhora do AME. Ações de promoção e não oferecer chupeta são importantes para uma maior duração do AME e o apoio e manejo no puerpério precisam ser fortalecidos.
Palavras-chave:
Aleitamento materno, Saúde materno-infantil, Estudos de coorte
IntroductionIn the 1970s, the median duration of breastfeeding was only 75 days and exclusive breastfeeding was practically not practiced.
1 Faced with this situation, Brazil has implemented various policies that have formed a successful history of improving breastfeeding practices over the last 40 years, with a multitude of simultaneous actions carried out in a multisectoral way, described as a gear model
2: The national promotion campaigns, the
Iniciativa Hospital Amigo da Criança (Friendly Hospital Initiative), the protection law that prohibits undue marketing of products that compete with breast milk (
Norma Brasileira de Comercialização de Alimentos pata Lactentes e Crianças de Primeira Infância, Mamadeiras, Bicos e Chupetas - NBCAL
3 Brazilian Standard for the Marketing of Food for Infants and Young Children, Bottles, Nipples and Pacifiers), the increase in prenatal care actions, the formation of the human milk bank network, among other actions,
4-6 are important examples that currently constitute the national policy to promote, protect and support breastfeeding.
According to the latest national survey conducted in the country in 2019, 45.7% of the children under six months of age were exclusively breastfeeding, which means that, despite significant progress, this practice is still falling short of national and international recommendations that mothers breastfeed their children, without introducing water or any other food, until they are six months old.
7Different factors influence exclusive breastfeeding and knowing them helps to prepare more efficient programs to have a positive impact on increasing the duration of breastfeeding. However, these factors can vary according to the region, both in their presence and importance. The city of João Pessoa is the capital of a state in the Northeast region, a region with great social inequality and the worst social and health indicators.
8 Exclusive breastfeeding (EBF) carried out for the recommended time, complies with the principles of human right to a healthy and nutritionally adequate diet. In places like João Pessoa, it can also have an economic and social impact due to the savings generated by not having to buy expensive breast milk substitutes and by protecting the newborns' health against diarrhea, respiratory infections, a reduction in infant deaths and an important protective effect against obesity and other non-transmissible diseases.
9-11A study on women in the South region of Brazil found that the presence of a partner reduced 40% of the mother's chance in continuing to breastfeed for two years or more, as is recommended.
12 However, regarding the period of breastfeeding, a cross-sectional study carried out in Rio de Janeiro in 2013 showed that mothers who did not live with their partners had a 24% lower prevalence of breastfeeding when compared to those with a partner.
13 Similarly, another cross-sectional study carried out in Campinas, in the state of São Paulo in 2010, showed that the presence of a partner helps lead to more assertive feeding practices in a timely manner and, therefore, more adequate EBF.
14 As these studies are from the Southeast of Brazil and are cross-sectional in design, little is known about the influence of the partner in the first six months of the baby's life in theNortheast region, from a follow-up study, where we can observe what happens over time.
Therefore this study sought to analyze the factors that favor a longer duration of exclusive breastfeeding among women living in João Pessoa - Paraíba, users of the
Sistema Único de Saúde (SUS) (Public Health System) and to identify whether the presence of a partner favors a longer duration of breastfeeding.
MethodsThis is a prospective cohort study of pregnant women using SUS in the city of João Pessoa, which according to data from the Atlas of Human Development in Brazil, had a population of 811,598 inhabitants (2,017) and a
Índice de Desenvolvimento Humano Municipal (IDHM) (City Human Development Index) of 0.763 (2,010). The pregnant women were recruited from 14
Saúde da Família (UBS) (Family Health Units) selected for convenience in the South neighbourhoods of Sanitary District III, which is not only the largest of the five districts, but is also characterized by middle- and low-income families. According to data from the
Sistema de Informações sobre Nascidos Vivos do Ministério da Saúde (Ministry of Health Live Birth Information System), there were around 12,000 births in 2018 in the city, which would correspond to the target population of the study. All the women who showed up for their prenatal routine appointments during the data collection period, from Monday to Friday, and who met the inclusion criteria of the study, were invited to take part in the study, until the desired sample size was completed. The selection of the women in the study was not intended to be representative of the population, but rather to obtain groups that could be compared without any selection of bias.
The inclusion criteria were 18 years of age or older, pregnant during any gestational period and with normal development of the pregnancy and without any limitations in terms of breastfeeding or caring for their child. Women who had a communication problem or declared a health problem that prevented them from breastfeeding their children were excluded.
The sample size for this study was estimated in order to be able to observe different factors with a Relative Risk equal to or greater than 1.5 for the early interruption of EBF. Considering a 95% confidence interval and a test power of 80%, dividing the exposed and unexposed into groups of similar size and with a percentage of positive exposed of 50%, a minimum sample size of 132 participants would be required.
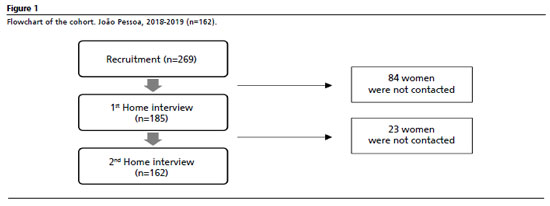
15Recruitment began in October 2018 when a first questionnaire was administered to identify the pregnant woman. To compensate for loss to follow-up, 269 pregnant women were initially recruited. Loss to follow-up was considered pregnant women who were unsuccessfully interviewed at home more than three times, on different days and at different times. 185 women were located in their homes for the first home interview and 162 for the second home interview, making up the sample size for this cohort (Figure 1). The visits to each mother were about three months apart. As this was an open cohort, pregnant women were included continuously and at different gestational ages (GA), so their children/babies were also different ages at the time of the interview. To carry out the survival analysis, it was sufficient to classify the children according to whether they were exclusively breastfed, yes or no, and to record their age at the time.
To check for any selection bias due to losses, the pregnant women who were followed up were compared with those recruited and not located for follow-up. The chi-square test showed that there were no differences between these two groups with regard to living with a partner, maternal schooling, skin color, maternal occupation outside the home and whether she was entitled to social benefits.
All the information was collected through face-to-face interviews using smart phones to record the data, with the help of the KoboCollect application, a free open source platform developed by the Harvard Humanitarian Initiative.
16During recruitment, information was collected on address and telephone contact, socioeconomic data, the characteristics of the pregnant woman's family, information about the pregnancy and the care received during prenatal care. At home, after the birth of the baby, questions were asked about puerperal care, health and infant feeding.
The event of EBF duration, was estimated by the number of days between the birth of the baby and the introduction of the first food or water into the child's diet. Mothers who were still breastfeeding were asked: "In addition to breastfeeding, have you offered water or any other food?" If so, they were asked: "What was your child's age at the time of this food introduction?" For mothers who had already weaned completely, they were asked: "Until what age did your child suckle only at the breast, without the introduction of water or other food?". The last complete piece of information from each mother was taken into account, either at the first home interview, if they had already interrupted EBF, or at the second home visit. At the end of the follow-up, if the mother had not yet introduced any food, the baby's age was taken as the EBF time and this data was analyzed as censoring in the survival analysis.
All the variables of interest were categorized and the relationship between each of them and EBF time was tested through survival analysis, using the Kaplan-Meyer technique and the Log-Rank test, with a significance level of 5%, to compare the survival curves of EBF time for each comparison group. To investigate the independent effect of the variables that were related to the EBF duration, a Cox multiple regression model was constructed, including all the variables that had a p-value of less than or equal to 0.20 in the Kaplan-Meyer analyses and progressively removing those that did not have a
p-value of less than 5%, according to the Wald statistic, progressively removing the variables from the initial model.
The research protocol was submitted to and approved by the Research Ethics Committee /
Plataforma Brasil of the State of Paraíba, opinion number 2.413.361 of December 4, 2017 (CAAE: 78557717.6.0000.5188).
ResultsA total of 162 women were recruited at different gestational ages, 16.4% in the first, 32.7% in the second and 50.9% in the third trimester. 53.1% of the women were between 25 and 35 years old; the vast majority lived in households with up to three residents (58.4%); 70.4% lived with a partner (married or in a stable union); 1/3 of the women were assisted by some kind of social cash transfer program and 44.5% had a low income (up to ½ monthly minimum wage per capita = R$ 500.00); 57.4% self-reported being mixed colored skin. 74.1% of the participants had up to high school education and 79.0% worked outside the home; 63% of the women reported not being primiparous and 68.8% said they had received guidance on breastfeeding, but only 24.1% said they had had at least one consultation with a nutritionist (Table 1).
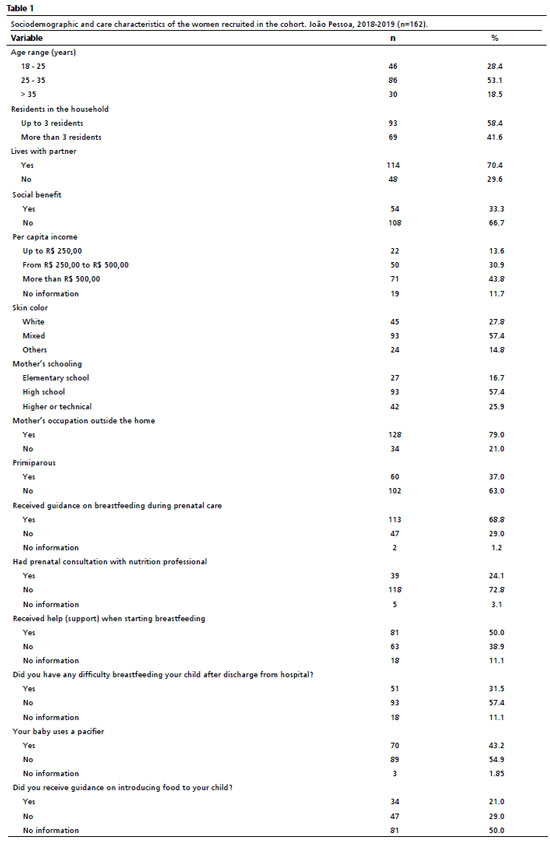
After the baby's birth, half of the mothers reported having received some support to breastfeed, the vast majority of which (78.5%) was offered while still at the maternity ward, by nurses, pediatricians, milk bank staff or some other unspecified health professional. After being discharged from hospital, 17 women received support mainly from relatives and friends, which corresponds to 21.5% of the mothers who received support or 10.7% of all mothers, but 31.5% of the women reported having had some difficulty breastfeeding after being discharged from hospital.
The use of pacifiers by babies was reported by 43.3% of mothers before stopping breastfeeding and with regard to guidance on introducing food to their children, half of the mothers were unable to answer and of those who did, less than half (42%) said they had received some guidance (Table 1).
The median duration of EBF, estimated by survival analysis, was 120 days (95%CI = 96.6-143.4; 95 events and 67 censorships). When comparing different groups of women, divided according to the independent variables of the study, three characteristics showed a significant difference between the groups: guidance on breastfeeding in the prenatal period (
p<0.013); difficulty on breastfeeding (
p<0.004); and pacifier use (
p<0.005), according to the log-rank test. Receiving guidance on breastfeeding in the prenatal period or not having difficulty to breastfeed, the duration of breastfeeding increased by 55 days (an increase of 38%). Not using a pacifier, the median duration of EBF increased by 60 days (41% increase) (Table 2).
The variables that were statistically significant and those with a
p-value of less than 0.20 ("received help" and "Lives with partner") were included in a multiple Cox regression model. The independent factors associated (Hazard Ratio) with stopping exclusive breastfeeding much earlier were: receiving guidance on breastfeeding during prenatal care (67%), not using a pacifier (64%) and not having had difficulties breastfeeding (Table 3).
When observing the behavior of women's breastfeeding duration according to the presence of a partner, it was possible to see a difference in the first four months (Figure 2A). The comparison test for this period proved to be significant and the median breastfeeding period was 33.3% longer among mothers who lived with a partner (median 50 days
vs 75 days,
p=0.002 log-rank test) (Figure 2B). This difference disappears after this period, as can be seen in Figure 2A.
DiscussionThe results of this study showed that the estimated median duration of EBF observed among the women in João Pessoa, around four months, was better than that observed for Brazil in the national study carried out in 2019, where a median of three months was observed.
8 These results are positive and were also better than those observed in previous studies carried out in different cities in the State of Paraíba, in 2002 among 70 cities, which showed that only 16.6% of children under six months were on EBF
17 and in 2005, with data from 14 cities where 30.5% of the children under six months were on EBF.
18In the analysis of the actions that had a positive effect on the longer duration of EBF, there is the guidance given during prenatal care. It was observed that two out of three pregnant women reported having received this guidance and considering the importance of this activity, its low cost and its great effectiveness, it could be expanded to strengthen the national breastfeeding promotion policy.
19 A meta-analysis analyzed the effect of breastfeeding promotion and confirmed that mothers who received guidance on breastfeeding during prenatal care were 41% more likely to start and continue breastfeeding compared to mothers who did not receive this guidance.
20On the other hand, having had a consultation with a nutritional professional had a low reported frequency, only one in four women, and was not found to be effective in improving the duration of their EBF time. So the low number of women who had access to this service, as well as the low presence of nutritionists in the units, may explain this result.
Half of the women reported having received help with breastfeeding after the birth of their baby while still in the maternity ward, but this did not have an impact on the duration of EBF. However, after hospital discharge, a third of the mothers reported having had difficulties on breastfeeding and this was a factor that had an impact on them breastfeeding exclusively for less time. The difficulties, which are frequent and well described in the literature, are related to factors such as: the baby's inadequate position during breastfeeding, difficulty latching onto the breast, nipple wounds, maternal pain and discomfort, breast engorgement, nipple cracks and wounds, and can even lead to more serious problems such as mastitis, all of which influence the interruption of breastfeeding.
19-21 Only one tenth of the mothers reported having received some support at this time, and almost always from relatives or friends, which shows the possible weakness of the follow-up actions during the puerperium carried out by the local primary health care services.
The importance of this type of action for establishing breastfeeding in a safe and pleasurable way for mother and child is well known. If Brazil has shown great success in promoting breastfeeding over the years, it is necessary to better implement support policies, whether through individual or group counseling, community networks, or remote means such as telephone contact or the use of social networks. Innovative initiatives such as the use of a virtual social network to provide timely support to puerperal women after hospital discharge have great potential for success.
22 An experimental study carried out with women who had their babies at the
Hospital Universitário in João Pessoa, a population similar to that of this study, found that puerperal women who took part in a virtual support group had an EBF duration of 149 days, almost the double that of those who did not take part in the same group.
23This presente study found that the presence of a partner had a positive effect on the start of breastfeeding and its continuity until the baby was four months old. Other studies recognize the importance of the partner at the beginning of the puerperium,
24 or of family support, which includes the partner, at six months.
25 However, this study draws attention to the fact that this effect disappears after this period. A cohort carried out in Viçosa, Minas Gerais, in 2011 and 2012 followed 168 women and their children for 120 days and found that the lack of help from a partner in caring for the baby increased the likelihood of interrupting EBF by 33%, compared to women who received this support.
26 This result confirms the findings of the present study showing, in another region of the country, a similar effect in relation to care and support practices for the newborn and breastfeeding women. As the Minas Gerais study did not continue after 120 days, the disappearance of this protective effect of EBF observed in our study cannot be better compared.
The reduction in the difference in the duration of breastfeeding at four months postpartum between the groups with and without a partner could be a confounding factor attributed to women returning to work, which is an important factor already described in the literature.
17 However, in the current study, the comparison of the duration of breastfeeding between women who have paid jobs, with or without maternity leave, or even the comparison of these with those who do not work was not observed, which reinforces the findings regarding the positive result of the presence of a partner during this period for a longer duration of EBF.
There is a need for studies that can identify the role of the partner, as well as their conceptions of breastfeeding and consequently direct health actions towards this public, highlighting a possible positive impact that this type of action can have on increasing the duration of EBF, directly or indirectly.
27The use of a pacifier in the first months of life is proven to be harmful to the practice and maintenance of EBF, but it is still common among young infants.
28 A meta-analysis of Brazilian epidemiological studies found that, among the characteristics related to the child, the use of a pacifier was one of the main factors associated with interrupting EBF,
29 a result that is confirmed by international studies which show that this practice causes impaired sucking and consequently reduced milk production.
30The use of a bottle was not included in the analysis because the outcome studied was on EBF, so the use of a bottle, rather than being a risk factor, already constitutes the very interruption of this practice, with the exception of a very few cases of administration of human milk extracted via a bottle.
22A limitation of this study was not following up all the women recruited from the health services, which is a challenge for cohort studies, but the analyses showed that losses were random, minimizing this problem. It is also important to consider that this is not a representative population study, but a follow-up study aimed at identifying factors related to the duration of EBF in a group of women treated at SUS, so the results observed should be analyzed with caution.
On a positive note, the interviews were all conducted at home and by trained interviewers, and an attempt was made to confirm the information between each interview, always using the most recent one to avoid memory bias. The information provided was simple and easy to understand, guaranteeing the quality of the data analyzed. Despite the existence of many studies on the same subject, cohort studies such as this one make it possible to observe cause and effect relationships and identify which experiences women have had that favor a longer-lasting EBF practice.
It can be concluded that prolonged support from the partner can be a viable strategy for improving EBF. Promotional actions and not offering pacifiers are important for a longer duration of EBF and support and management in the puerperium need to be strengthened. In addition, it is recommended that new studies with greater statistical power be carried out, including representative samples of the population, contributing to strengthening the care of the mother and child group in a comprehensive, universal, equitable and continuous way during the lactation period.
References1. Venancio SI, Saldiva SR, Monteiro CA. Tendência secular da amamentação no Brasil. Rev Saúde Pública. 2013; 47 (6): 1205-8.
2. Pérez-Escamilla R, Dykes FC, Kendall S. Gearing to success with national breastfeeding programmes: The Becoming Breastfeeding Friendly (BBF) initiative experience. Matern Child Nutr. 2023 Jan; 19 (Suppl. 1): e13339.
3. Presidência da República. Lei nº 11.265, de 3 de janeiro de 2006. Regulamenta a comercialização de alimentos para lactentes e crianças de primeira infância e também a de produtos de puericultura correlatos. Brasília (DF): DOU de 4 de janeiro de 2006. [access in 2024 Abr 6]. Available from:
https://www.planalto.gov.br/ccivil_03/_ato2004-2006/2006/lei/l11265.htm4. Lamounier JA, Chaves RG, Rego MAS, Bouzada, MCF. Iniciativa Hospital Amigo da Criança: 25 anos de experiência no brasil. Rev Paul Pediatr. 2019; 37: 486-93.
5. Melo DS, Oliveira MH, Pereira DS. Brazil's progress in protecting, promoting and supporting breastfeeding from the perspective of the global breastfeeding collective. Rev Paul Pediatr. 2021; 39: e2019296.
6. Silva KB. Oliveira MIC, Boccolini CS, Sally EOF. Promoção comercial ilegal de produtos que competem com o aleitamento materno. Rev Saúde Pública. 2020; 54: 10.
7. Universidade Federal do Rio de Janeiro (UFRJ). Aleitamento materno: Prevalência e práticas de aleitamento materno em crianças brasileiras menores de 2 anos. 4: ENANI 2019. [
Internet] Rio de Janeiro (RJ): UFRJ; 2021. (108 p.). [access in 2024 Abr 6]. Available from:
https://enani.estudiomassa.com.br/wp-content/uploads/2023/10/Relatorio-4-ENANI-2019-Aleitamento-Materno.pdf8. Cherol CCS, Ferreira AA, Lignani JB, Salles-Costa R. Regional and social inequalities in food insecurity in Brazil, 2013-2018. Cad Saúde Pública. 2023; 38: e00083822.
9. Dib S, Fair FJ, McCann LJ, Nicholls A, Kalea AZ, Soltani H,
et al. Effects of Exclusive Breastfeeding Promotion Interventions on Child Outcomes: A Systematic Review and Meta-Analysis. Ann Nutr Metab. 2024; 80 (2): 57-73.
10. Horta BL, Rollins N, Dias MS, Garcez V, Pérez-Escamilla R. Systematic review and meta-analysis of breastfeeding and later overweight or obesity expands on previous study for World Health Organization. Acta Paediatr. 2023 Jan; 112 (1): 34-41.
11. Qiao J, Dai LJ, Zhang Q, Ouyang YQ. A Meta-Analysis of the Association Between Breastfeeding and Early Childhood Obesity. J Pediatr Nurs. 2020; 53: 57-66.
12. Martins EJ, Giugliani ERJ. Which women breastfeed for 2 years or more? J. Pediatr. 2012; 88 (1): 67-73.
13. Alves, Jessica de Souza, Oliveira, Maria Inês Couto de, e Rito, Rosane Valéria Viana Fonseca. Orientações sobre amamentação na atenção básica de saúde e associação com o aleitamento materno exclusivo. Ciênc Saúde Colet. 2018; 23 (4): 1077-88.
14. Mais LADomene SMA, Barbosa MB, Taddei JAAC. Diagnóstico das práticas de alimentação complementar para o matriciamento das ações na Atenção Básica. Ciênc Saúde Colet. 2014; 19 (1): 93-104.
15. Venancio SI, Saldiva SRDM, Monteiro CA. Tendência secular da amamentação no Brasil. Rev Saúde Pública. 2013 Dec; 47 (6): 1205-8.
16. KoboToolBox. Harvard Humanitarian Initiative. 2020. [access in 2022 Nov 12]. Available from:
https://www.kobotoolbox.org/ 17. Vianna RPT, Rea MF, Venancio SI, Escuder MM. A prática de amamentar entre mulheres que exercem trabalho remunerado na Paraíba, Brasil: um estudo transversal. Cad Saúde Pública. 2007 Oct; 23 (10): 2403-9.
18. Palmeira PA, Santos SMC, Vianna RPT. Prática alimentar entre crianças menores de dois anos de idade residentes em municípios do semiárido do Estado da Paraíba, Brasil. Rev Nutr. 2011 Jul; 24 (4): 553-63.
19. Venancio SI, Melo DS, Relvas GRB, Bortoli MC, Araújo BC, Oliveira CF,
et al. Effective interventions for the promotion of breastfeeding and healthy complementary feeding in the context of Primary Health Care. Rev Paul Pediatr. 2022; 41: e2021362.
20. Cohen SS, Alexander DD, Krebs NF, Yuong BE, Cabana MD, Erdmann P,
et al. Factors Associated with Breastfeeding Initiation and Continuation: A Meta-Analysis. J Pediatr. 2018; 203: 190-196.e21.
21. Rocha GP, Oliveira MDCF, Ávila LBB, Longo GZ, Cotta RMM, Araújo RMA. Condicionantes da amamentação exclusiva na perspectiva materna. Cad Saúde Pública. 2018; 34 (6): e00045217.
22. Galvão DMPG, Silva EMB, Silva DM. Use of new technologies and promotion of breastfeeding: integrative literature review. Rev Paul Pediatr. 2021; 40: e2020234.
23. Cavalcanti DS, Cabral CS, Toledo Vianna RP, Osório MM. Online participatory intervention to promote and support exclusive breastfeeding: Randomized clinical trial. Matern Child Nutr. 2019; 15 (3): e12806.
24. Freitas DAK, Pires T, Willges BS, Daudt L, Käfer KD, Martins FS,
et al. Determinantes para a interrupção do aleitamento materno exclusivo aos 30 dias de vida. Rev Paul Pediatr. 2022; 40: e2021096.
25. Brandt GP, Britto AMA, Leite CCDP, Marin LG. Factors Associated with Exclusive Breastfeeding in a Maternity Hospital Reference in Humanized Birth. Rev Bras Ginecol Obstet. 2021; 43(2): 91-6.
26. Machado MC, Assis KF, Oliveira FC, Ribeiro AQ, Araújo RM, Cury AF,
et al. Determinants of the exclusive breastfeeding abandonment: psychosocial factors. Rev Saúde Pública. 2014 Dec; 48 (6): 985-94.
27. Mitchell-Box KM, Braun KL. Impact of male-partner-focused interventions on breastfeeding initiation, exclusivity, and continuation. J Hum Lact. 2013; 29 (4): 473-9.
28. Santos EMD, Silva LS, Rodrigues BFS, Amorim TMAX, Silva CS, Borba JMC,
et al. Avaliação do aleitamento materno em crianças até dois anos assistidas na atenção básica do Recife, Pernambuco, Brasil. Ciênc Saúde Colet. 2019; 24 (3): 1211-22.
29. Pereira-Santos M, Santana MS, Oliveira DS, Nepomuceno RA, Lisboa CS, Almeida LMR,
et al. Prevalência e fatores associados à interrupção precoce do aleitamento materno exclusivo: meta-análise de estudos epidemiológicos brasileiros. Rev Bras Saúde Mater Infant. 2017; 17 (1): 59-67.
30. Buccini GDS, Pérez-Escamilla R, Paulino LM, Araújo CL; Venancio SI. Pacifier use and interruption of exclusive breastfeeding: Systematic review and meta-analysis. Matern Child Nutr. 2017; 13 (3): e12384.
Authors' contribution: Silva LKC: conceptualization of the work, analysis, data collection, definition of the methodology, project management, writing the initial version and writing the final version.
Viana MACBM: curated the data, defined the methodology and revised the final version.
Oliveira SF: data collection and writing the review and final version of the manuscript.
Lima RLFC: conceptualizing the work, defining the methodology and writing the final version and review.
Vianna RPT: conceptualization of the work, analysis, acquisition of funding, definition of the methodology, project management, writing the initial version and writing the final version.
All the authors have approved the final version of the article and declare no conflict of interest.
Received on May 16, 2024
Final version presented on December 5, 2024
Approved on December 9, 2024
Associated Editor: Ricardo Cobucci
 ; Maria Augusta Correa Barroso Magno Viana2
; Maria Augusta Correa Barroso Magno Viana2 ; Sara Ferreira de Oliveira3
; Sara Ferreira de Oliveira3 ; Rafaela Lira Formiga Cavalcanti de Lima4
; Rafaela Lira Formiga Cavalcanti de Lima4 ; Rodrigo Pinheiro de Toledo Vianna5
; Rodrigo Pinheiro de Toledo Vianna5