ABSTRACT
OBJECTIVES: this study aimed to assess the quality of life and the relationship between the sleep of parents and primary caregivers of children under two years old.
METHODS: a cross-sectional study was conducted with parents, mothers, or caregivers of infants aged one to 23 months, using online administration of the Pittsburgh Sleep Quality Index (PSQI) to assess sleep quality and the WHOQOL-BREF to assess quality of life.
RESULTS: the vast majority of the 456 respondents were mothers (97.6%)and primary caregivers of the child (97.6%). Among the participants, 76.5% reported having a good or very good quality of life, which was not influenced by the age of the child. The vast majority (83.4%) of respondents had a PSQI score above 5, indicating poor sleep quality. Sleep quality showed a significant negative correlation with most domains of the WHOQOL-BREF.
CONCLUSIONS: mothers of children under two years old experience poor sleep quality, which negatively impacts their quality of life. Healthcare professionals should pay special attention to the physical and mental health of caregivers of young children, and public policies related to parental leave rights and labor rights should take such results into account.
Keywords:
Sleep quality, Quality of life; Maternal health
RESUMO
OBJETIVOS: avaliar a qualidade de vida e a relação existente entre o sono de pais e principais cuidadores de crianças menores de dois anos.
MÉTODOS: estudo transversal realizado com pais, mães ou cuidadores de lactentes de um a 23 meses de vida, com aplicação online dos questionários Pittsburgh Sleep Quality Index, para avaliação da qualidade do sono, e WHOQOL-BREF, para qualidade de vida.
RESULTADOS: a maior parte dos 456 respondedores eram mães (97,4%) e principais cuidadores da criança (97,6%). Dentre os participantes, 76,5% referiram ter uma qualidade de vida boa ou muito boa, o que não teve impacto com a idade da criança. A grande maioria (83,4%) dos respondedores teve uma pontuação no PSQI >5, indicando qualidade do sono ruim. A qualidade do sono teve correlação negativa e significativa com a maioria dos domínios do WHOQOL-BREF.
CONCLUSÕES: mães de crianças com menos de dois anos apresentam baixa qualidade do sono, o que impacta negativamente em sua qualidade de vida. Profissionais da saúde devem ficar especialmente atentos à saúde física e mental dos cuidadores de crianças pequenas, e as políticas públicas relacionadas aos direitos de licença maternidade e paternidade e direitos trabalhistas devem levar tais resultados em consideração.
Palavras-chave:
Qualidade do sono, Qualidade de vida, Saúde materna
IntroductionSleep is a crucial part of the mechanism of restoration of body balance and the preservation of psychological health. As the human being growths and develops, the characteristics of adequate sleep modify, varying in relation to duration, distribution of stages and circadian rhythm.
1 In this context, the quantity of hours of sleep in adult life is lower and depends on the cycle of sleep, which is related to age and external factors. Therefore, sleep may be a challenge for parents of small children, since the manner of raising a child may be a prejudicial external factor, affecting health and well-being by means of physiological alterations, such as weariness, memory lapse, absenteeism from work and drowsy driving.
1 There are surveys that aims to assess the quality of sleep in parents of children with specific statuses, such as the experience of a disease,
2 prematurity,
3,4 or low birth weight.
5 It is known that sleeping is essential to maintain the adequate physiological functioning of the body and that the deprivation of this organic function, which occurs with parents of neonates with behavioral problems of sleep, for example, is associated with depression, fatigue and cognitive disorders.
6 Furthermore, the increase of stressing factors for caregivers in the early years of children’s life, such as the hospitalization of a newborn, contributes to higher indexes of psychological disorders, such as anxiety and higher probability of developing postpartum depression.
7However, it is important to assess whether the birth of a healthy child is capable of affecting the quality of life and sleep of families, since the existing studies aim to screen for the impact of the health of children on the lives of parents only in specific situations in which there is any damage in children’s health.
2-5 In spite of this, the literature is still scarce with regard to surveys that assess, mainly, the relationship between quality of life and sleep in caregivers of children, even those healthy.
The literature shows a direct relationship between low quality of maternal sleep and the presence of negative indicators of physical and mental health,
5 which justifies the indispensabilityof broader surveys. Moreover, a study indicates that the well-being of a child, generally prioritized by parents, lead the latter to experience lack of sleeping and consequently, of energy for activities and social events, affecting their way of life.
2 Also, the quality of maternal sleep was described as a significant predictor for stress, fatigue and humor alterations.
6 Thus, understanding the impact of raising children on quality of parent’s lives is essential to approach health in a multidimensional manner.
This study aims to assess the potential relationship between quality of life and the sleep of parents and main caregivers of children under two years of age.
MethodsCross-sectional study carried out with the application of an online questionnaire with parents of nurslings aged between one and 23 months of life. The survey was conducted in the Federal University of Juiz de Fora, however it was publicized in social networks in a profile created for such, allowing the participation of Brazilian families. Data collection occurred between September 1
st and October 31
th, 2023.
The inclusion criterion was being father, mother or main caregiver of a nursling of up to two years of life. The sample size was calculated considering a 95% confidence interval, with sampling error of 5%, and an additional of 10% of participants for the compensation of potential sample losses. We used as a basis an estimated population of live births in Brazil in the last two years that preceded the survey (2,677,101 live births in 2021 and 2,561,922 live births in 2022, according to data from the Ministry of Health).
8 This resulted in a sample size of 423 participants.
We excluded participants that did not fulfill the tool for data collection within the deadline of the survey and those from other countries of Portuguese language that eventually fulfilled the tool.
Sociodemographic data collected were the age of the caregiver, gender, age of the nursling, schooling, income in minimum wages (at the time of the survey, the national minimum wage was R$1320,00) and the exercise of paid employment by the caregiver.
For the assessment of quality of life, we used the WHOQOL-BREF a self-administered instrument composed of 26 questions that generates a profile of quality of life in four domains, validated in Brazil by Fleck
et al.
9 In this validation, the internal consistency of the domains, according to the Cronbach’s alpha reliability coefficient, varied from 0.69 to 0.84 between the domains, and scored 0.91 for the entire questionnaire; the coefficients of test and retest varied between 0.69 and 0.81 (
p<0.0001).
9 The domains that compose the scale are physical health (score from 7 to 35 points), which assesses subjects such as pain, discomfort, fatigue and use of medications, psychological health (score from 6 to 30 points), which assesses positive feelings, self-esteem, memory, spirituality; social relationships (score from 3 to 15 points), which asks about relationships, social support and sexual activity; and environmental health (score from 8 to 40 points), which assesses subjects such as security, financial resources, home environment, leisure and transport.
For the assessment of sleep quality, we used the Pittsburgh Sleep Quality Index (PSQI), a self-administered tool, validated in Brazil, for adult population, by Bertolazi
et al.
10 The internal consistency of the Brazilian version by Cronbach’s alpha reliability coefficient is 0.73, and the test and retest coefficient was 0.82.
10 The PSQI is composed of 24 questions that assess seven components of sleep: subjective quality, sleep latency (calculated by means of questions that evaluate the time elapsed to fall asleep), duration of sleep; habitual efficiency (calculated from the number of hours spent sleeping and the number of hours spent on bed); presence of sleep disorders; use of sleeping medications and daytime sleepiness. The sum of scoring of the seven components results in a total score, for which scoring above 5 indicates bad sleep quality.
11Data obtained from the online questionnaire were extracted for Microsoft Excel software and the Statistical Package for the Social Sciences (SPSS) version 22.0 software, used for the statistical analyses. The descriptive analysis was performed with mean calculation, standard deviation, absolute and relative frequency.
The relationship between the result of WHOQOL-BREF and PSQI scales within each other and the sociodemographic variables was verified applying Pearson correlation and Student’s
t test for independent samples (in case of normality of data) or by the Mann-Whitney
U test (in the absence of normality of data), considering the level of statistical significance of 5% for all tests. Shapiro-Wilk test was used to assess the normality of data. For the interpretation of the magnitude of coefficients in Pearson correlation, we used the Cohen reference (1988), according to which coefficients varying from 0.10 to 0.29 indicate weak correlation, scores between 0.30 and 0.49 suggest moderate correlation, and values between 0.50 and 1.00 are interpreted as strong correlation.
12The research was approved by the Research Ethics Committee of the Federal University of Juiz de Fora, under CAAE number 69944923.3.0000.5147, opinion number 6.259.629, August 24, 2023.
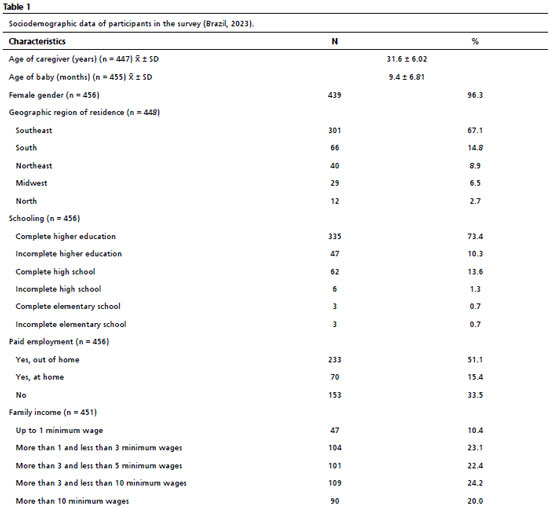
ResultsA total of 456 respondents completed the survey, with predominance of female participants (96.3%) and that identified themselves as mothers (97.4%) of a child under two years of age. Most respondents (97.6%) were the main caregivers of the children. The age of participants varied from 16 to 50 years, with a mean of 31.6 years (standard deviation: 6.02). The age of the children of respondents varied from one to 23 months of life, with 43.1% of babies between one and six months; 24.4% between seven and 12 months and 32.5% between 13 and 23 months of life. Most participants were from the Southeast region of Brazil (67.1%), but with representation of all geographic regions. Sociodemographic data of participants on the survey are detailed in Table 1.
In the self-referred evaluation of quality of life, 76.5% participants referred to having a good or very good quality of life, whilst only 6.8% referred to a bad or very bad quality of life. In the question about satisfaction with oneself health, 51.1% revealed being satisfied or very satisfied, whilst 26.5% was dissatisfied or very dissatisfied with their health.
The median scores for the four domains of the WHOQOL-BREF questionnaire (physical health, psychological health, social relationships and environmental health) were compared in relation to sociodemographic variables (age of the participant, age of his/her children, schooling and income), and these results are presented in Table 2.
We observed that the child’s age did not correlate with any of the domains of quality of life. The age of the respondent correlated weakly with the environment domain (
p<0.01). Schooling and income presented weak correlation, however statistically significant (
p<0.001), with the domains physical and psychological health. For the environmental health domain, there was moderate correlation with schooling and strong with income (
p<0.01 for both). There was no correlation between schooling and income with the domain of social relationships. (Table 2).
When questioned about how they classified sleep quality in the last month, 65.1% of participants answered having bad or very bad quality. Most (83.4%) respondents had a PSQI score above 5, which indicates bad sleep quality. The PSQI scoring presented weak positive correlation, however statistically significant, with the schooling of participants, and weak negative with income. There was no correlation with the age of the respondent and with the age of the child (Table 2).
The scoring of the seven PSQI components had negative correlations and was statistically significant with most domains of WHOQOL-BREF, as detailed in Table 3. The scoring of the global PSQI score had negative correlation and was statistically significant with all domains of WHOQOL-BREF (Table 3). This correlation was strong for the physical health domain (r= -0.548), and moderate for the psychological domain (r= -0.368), social relationship domain (r= -0.362) and environmental health domain (r= -0.316).
In the motivations mentioned related to difficulty for sleeping in the PSQI questionnaire, 77.5% of respondents that indicated “other reasons” besides those enlisted in the questionnaire, evidenced a motivation related to the baby, such as waking up for breastfeeding or providing another type of care (non-tabular data).
The Shapiro-Wilk test was used to assess the normality of data of variables that represented the four WOQOL-BREF domains and the seven PSQI components, as well as the PSQI final score, (all with
p<0.01), evidencing an asymmetrical distribution of data (non-tabular data).
The means of scores of the four WHOQOL-BREF domains were higher within respondents with paid employment, in a statistically significant manner, indicating that having a job was protective in relation to a better quality of life (Table 4). However, the PSQI score was higher for those who did not have paid employment, suggesting worse sleep quality for this subgroup. The means of scores of the WHOQOL-BREF domains and PSQI did not diverge in a statistically significant manner within caregivers with children with less or more of one year of life.
DiscussionIn the present study, most caregivers of children under two years of age from the sample revealed to have impairments in sleep quality, which in turn was correlated to the domains of quality of life. Nevertheless, most participants demonstrated to be satisfied with their own quality of life.
Sleep is essential to maintain the balance of human functions, being responsible by the physical and psychological restructuration. The results of this research corroborates this conceptualization when demonstrating that all assessed domains for quality of life – social, psychological, physical and environmental – had negative impacts for low sleep quality. Physiological factors related to the care of the child, such as breastfeeding, were among the reasons for low sleep quality, suggesting that the care provided to a child under two years of age, yet healthy, may lead to impacts for mothers. Moreover, it is important to consider that the birth of a child leads to physiological modifications related to diuresis, menstruation and hemoglobin levels, which seem to impact maternal sleep at least at the first 12 months of a baby’s life.
13Studies that assess sleep quality in parents of healthy children are still scarce. An integrative literature review revealed that the sleep of women in the postpartum period is more fragmented, short and less restorative.
3 Most participants in the research presented altered PSQI scores, demonstrating impaired sleep quality, which did not modify significantly to the extent that the child is growing. This is particularly relevant since there are researches that demonstrate that low sleep quality is associated with sleepiness and daytime impairment, reverberating also in damages to health, such as higher risk of developing cardiovascular diseases, systemic arterial hypertension, chronic stress and immunodepression.
14 Still, a systematic review and meta-analysis concerning the subject demonstrated that the birth of a child affects the total time of sleep and the efficiency of parental sleeping, mainly in the first 16 weeks of life.
13 It may be supposed, thus, that the prolonged impairment in the sleep quality of parents of small children may lead to global and longstanding repercussions in their health.
According to a previous study, which carried out a functional linear regression for the characterization of sleep-wake standards, mothers who breastfed used to be awake during nighttime and demonstrate diminished daytime activity.
15 On the other hand, in another research, breastfeeding itself did not negatively affect the maternal sleep quality, although the duration of the nighttime sleep of the nursling was significant in the prediction of short duration of maternal sleep.
16 In this study, sleep quality was assessed with the PSQI, which does not bring specific questions about sleep impairments with breastfeeding or care with the child, however these factors were frequently mentioned by the mothers as being associated with the need of waking up frequently.
Surveys about parental sleep in the postpartum period have been concentrated, mainly, in mothers of children with specific situations, such as prematurity or disease. In this perspective, the survey carried out by Edéll-Gustafsson
et al.
17 revealed that mothers of preterm newborns experienced more stress than mothers of healthy babies, which negatively influenced their sleep. The study of Marthinsen
et al.,
5 in turn, demonstrates that the sleep of mothers of preterm newborns is mentioned as bad, mainly in the earlier stage right after birth. Total time of sleep inferior to seven hours, fragmented sleep and frequent nighttime awakenings were observed in that survey, in the study population.
5In the present study, we confirmed that having paid employment is associated with better scores in three of the four domains of WHOQOL-BREF, and with better sleep quality by PSQI, in a statistically significant manner. Similarly, a previous study demonstrated that some mothers are more susceptible of presenting bad sleep in the puerperal period than others are: mothers of preterm newborns with higher depressive symptoms or with lesser amount of daily activities reported less restorative sleep than mothers of preterm newborns with lower depressive symptoms or higher amount of daily activities.
18 This may suggest that stimulating the execution of activities not directly related to childcare, such as paid employment, may have positive effects for this population.
In the present study, there was no statistically significant difference in the scores for sleep quality and quality of life within parents of children in the first and second year of life. Similarly, a research demonstrated that approximately 26% of parents are unhappy with the sleep of their children in the first year of life, a percentage that stood similar in the second year of life.
19 The unhappiness of parents with the sleep of their children already in the first year of life had future correlation with sleep problems screened in a validated questionnaire; however, the researchers did not assess the impact of these problems in the sleep of parents.
19There are studies that demonstrate that anxiety, depression, stress and lower income are related to bad sleep quality in mothers whose preterm babies were hospitalized in Neonatal Intensive Care Units.
20 Also, there are researches demonstrating a worse sleep quality of children with acute or chronic diseases, hospitalized or not. In these researches, the conclusion was that the dedication of parents to childcare leads to a sleep with shorter duration,
2 worse quality
8,21 and symptoms of daytime fatigue.
3 However, a hospitalized or sick child brings several additional factors that influence the sleep quality of parents, such as parental stress;
22 familiar issues and those related to environment of childcare;
23 concerning with the critical status of the child, being or not aside the bed, hard feelings and thoughts;
20 and even pathological anxiety and postpartum depression.
8 However, the present study suggests that even parents of children born at term and/or healthy ay present negative impacts in sleeping and quality of life.
Sleep disorders lead to several adverse impacts in the quotidian since it diminishes the daytime functioning of people, increases the predisposition to the development of psychiatric disorders, cognitive deficit, onset and aggravation of health problems, risks of traffic accidents, absenteeism in the workplace, worsening of relationships, with different reverberations in short, medium and long term.
24 In spite of this, in this research, most participants self-evaluated the quality of life positively. It is necessary to recall that quality of life is multidimensional, and influenced by several factors aside from sleep. We cannot disregard, for example, that respondents of the research are very happy with the birth of a child, which would improve their perception of quality of life. Another relevant question is that a significant part of respondents has paid employment, and that income and schooling were elevated in our sample, making it possible, thus, higher resources such as the hiring of an auxiliary caregiver, which may influence the positive self-perception of quality of life.
Researches that aim to intervene in the sleep quality of parents and small children are still lacking, and the strategies for this goal are varied, generally involving the improvement of sleep of babies. A study with a cognitive-behavioral intervention, of single branch, demonstrated the benefits of sleep for children and parental stress, however with a low number of samples and did not use a control group.
25 A recent systematic review, however, demonstrated the benefit of varied intervention for the sleep of small children, such as reduction of screen time, going to sleep earlier and maintain a quiet routine before sleep time, highlight the need of individualizing cases and guidelines provided by health professionals.
26Some limitations of this research deserve to be highlighted. First, since it is a cross-sectional study, the assessment was performed punctually, not demonstrating the progressive evolution – positive or negative – of sleep quality, associating the maintenance or modification of aspects involved; secondly, most participants were from the Southeast region, and an elevated percentage had complete higher education, which may impair the generalization of results. We did not collect information on the necessity and frequency of breastfeeding during nighttime, which may affect the sleep of respondents. Since it is a research with online data collection, the respondents had access to the internet, which brings a relative limitation to the results of the research concerning sociodemographic range, when it does not approach people without access to the internet. It is necessary to consider the possibility of answer bias, that is, the participants who agreed answering to the survey possibly were interested in it because of having complaints related to sleep quality or quality of life. Lastly, we did not collect information on previous diagnoses related to the mental health of participants.
On the other hand, it is worth highlighting that the research used validated instruments, with a significant sample size and a sample that represents a population of real life mothers.Moreover, however we mentioned several researches that assessed the sleep quality and quality of life of parents of preterm children or bearers of chronic diseases, the literature still lacks studies that assess such outcomes in the population of parents in general. Therefore, this research brings the originality of the result of an impaired sleep quality even for caregivers of healthy children born in term.
The low quality of sleep may lead to negative consequences for health, work and social relationships of parents of small children, and this may be further studied. Researches that assess physical and mental health and symptoms of fatigue in this population are still lacking, as well as the impairments for the quotidian life that may occur with sleep deprivation. Additionally, such results may influence public policies related to parental leave rights and other labor rights, which are strongly divergent in different countries. Moreover, it is necessary that health professionals are specifically aware of the physical and mental health of caregivers of small children.
References1. Müller MR, Guimarães SS. Impacto dos transtornos do sono sobre o funcionamento diário e a qualidade de vida. Estud Psicol (Campinas). 2007 Oct; 24(4): 519-28.
2. Smith S, Tallon M, Smith J, Angelhoff C, Mörelius E. Parental sleep when their child is sick: A phased principle-based concept analysis. J Sleep Res. 2022 Oct; 31(5): e13575.
3. Baumgartel K, Facco F. An Integrative Review of the Sleep Experiences of Mothers of Hospitalized Preterm Infants. Nurs Womens Health. 2018 Aug; 22 (4): 310-26.
4. Lee, Shih-Yu; kimble, Laura P. Impaired sleep and well-being in mothers with low-birth-weight infants. J Obstet Gynecol Neonatal Nurs. 2009 Nov-Dec; 38 (6): 676-85.
5. Marthinsen GN, Helseth S, Fegran L. Sleep and its relationship to health in parents of preterm infants: a scoping review. BMC Pediatr. 2018 Nov 12; 18 (1): 352.
6. Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol. 2007 Mar; 21 (1): 67-73.
7. Castro MS, Lima RFS, Christoffel, MM, Brito, AGL, Azevedo, AMC. Sleep quality of mothers of newborns admitted to the Neonatal Intensive Care Unit. Res Soc Dev. 2020; 9 (9) (Sup. 1): e697997987.
8. Ministério da Saúde (BR). Sistema de Informações sobre Nascidos Vivos. 2024. [acesso em 2024 Mai 20]. Disponível em:
http://plataforma.saude.gov.br/natalidade/nascidos-vivos/9. Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L,
et al. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida “WHOQOL-bref”. Rev Saúde Pública. 2000 Apr; 34 (2): 178-83.
10. Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, Barreto SS. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Medicine. 2011 Jan; 12 (1): 70-5.
11. Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989; 28: 193-213.
12. Cohen J. Statistical power analysis for the behavioral sciences. 2
nd ed. Hillsdale, NJ, Erlbaum; 1988.
13. Parsons L, Howes A, Jones CA, Surtees ADR. Changes in parental sleep from pregnancy to postpartum: A meta-analytic review of actigraphy studies. Sleep Med Rev. 2023 Apr; 68: 101719.
14. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D,
et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep. 2015 Aug; 38 (8): 1161-83.
15. Crittenden AN, Samson DR, Herlosky KN, Mabulla IA, Mabulla AZP, McKenna JJ. Infant co-sleeping patterns and maternal sleep quality among Hadza hunter-gatherers. Sleep Health. 2018 Dec; 4(6):527-534.
16. Demirci JR, Braxter BJ, Chasens ER. Breastfeeding and short sleep duration in mothers and 6-11-month-old infants. Infant Behav Dev. 2012 Dec; 35 (4): 884-6.
17. Edéll-Gustafsson U, Angelhoff C, Johnsson E, Karlsson J, Mörelius E. Hindering and buffering factors for parental sleep in neonatal care. A phenomenographic study. J Clin Nurs. 2015 Mar; 24 (5-6): 717-27.
18. Shelton SL, Meaney-Delman DM, Hunter M, Lee S-Y. Depressive symptoms and the relationship of stress, sleep, and well-being among NICU mothers. J Nurs Educ Pract. 2014; 4(8): 70-9.
19. Harskamp-van Ginkel MW, Imkamp NLE, van Houtum L, Vrijkotte TGM, Ben Haddi-Toutouh Y, Chinapaw MJM. Parental Discontent with Infant Sleep During the First Two Years of Life. Behav Sleep Med. 2023 Nov; 21 (6): 727-40.
20. Schaffer L. The impact of guided imagery on sleep quality in mothers of preterm infants. [dissertation]. California: University of San Diego; 2012. [access in 2024 Jan 17]. Available from:
https://digital.sandiego.edu/dissertations/424/21. Stremler R, Dhukai Z, Wong L, Parshuram C. Factors influencing sleep for parents of critically ill hospitalised children: a qualitative analysis. Intensive Crit Care Nurs. 2011; 27 (1) 37-45.
22. Haddad S, Dennis CL, Shah PS, Stremler R. Sleep in parents of preterm infants: A systematic review. Midwifery. 2019 Jun; 73: 35-48.
23. Amorim M, Silva S, Kelly-Irving M, Alves E. Quality of life among parents of preterm infants: a scoping review. Qual Life Res. 2018 May; 27 (5): 1119-31.
24. Müller MR, Guimarães SS. Impacto dos transtornos do sono sobre o funcionamento diário e a qualidade de vida. Estud psicol (Campinas). 2007 Oct; 24 (4): 519-28.
25. Schnatschmidt M, Lollies F, Schlarb AA. A single-arm pilot study: can a parental sleep intervention for sleep-disturbed young children in individual settings improve children’s sleep, crying, eating, and parental distress in mothers and fathers? BMC Pediatr. 2022 Oct; 22 (1): 578.
26. Cook G, Carter B, Wiggs L, Southam S. Parental sleep-related practices and sleep in children aged 1-3 years: a systematic review. J Sleep Res. 2024 Aug; 33 (4): e14120.
Authors’ contributionVitorino LS, Costa LH, Camargo MN, Oliveira MED, Silva RGO: data collection, writing of the manuscript. Alvim VF: coordination of the project, data analysis, writing of the manuscript.
Grunewald STF: conceptualization and writing of the research project, data analysis, writing of the manuscript. All authors approve the final version of the article and declare no conflicts of interest.
Received on February 16, 2024
Final version presented on August 15, 2024
Approved on August 28, 2024
Associated Editor: Karla Bomfim
 ; Ronald Godinho de Oliveira Silva 2
; Ronald Godinho de Oliveira Silva 2 ; Mila Nogueira Camargo 3
; Mila Nogueira Camargo 3 ; Larissa Honório Costa 4
; Larissa Honório Costa 4 ; Luiza Silva Vitorino 5
; Luiza Silva Vitorino 5 ; Vitor Fernandes Alvim 6
; Vitor Fernandes Alvim 6 ; Sabrine Teixeira Ferraz Grunewald 7
; Sabrine Teixeira Ferraz Grunewald 7