ABSTRACT
OBJECTIVES: to assess factors associated with the use of long-acting reversible methods (LARC) and women's concerns about them.
METHODS: this is a cross-sectional study conducted in a digital environment from April to June 2021, with the use of a structured instrument disseminated through social networks. The study included women of reproductive age (18 to 49 years old), who were not pregnant, not hysterectomized, not sterilized and whose partners were not vasectomized. Data were analyzed using logistic and multinomial regression.
RESULTS: the study population consisted of 1596 women aged 18 to 49 living in all regions of the country, 22% of whom were using LARC. Aspects associated with LARC use were younger age, having health insurance, being in a relationship and not wanting to get pregnant. Half of LARC users reported having some kind of concern about the method, the most frequent being the risk of becoming pregnant (36.2%). The aspects associated with having concerns about using LARC were the type of method, not being in a relationship and not wanting to get pregnant.
CONCLUSIONS: LARC users are not a homogeneous group. Current experience of using LARC is lived with concerns, including some about its efficacy.
Keywords:
Sexual and reproductive health, Long-term reversible contraception, Intrauterine devices
RESUMO
OBJETIVOS: determinar os fatores associados ao uso de métodos reversíveis de longa ação (LARC) e às preocupações das usuárias.
MÉTODOS: estudo transversal conduzido em ambiente digital de abril a junho de 2021, por meio de instrumento estruturado disseminado por redes sociais. Foram incluídas mulheres em idade reprodutiva (18 a 49 anos de idade), não grávidas, não histerectomizadas, não esterilizadas e cujos parceiros não eram vasectomizados. Os dados foram analisados por meio de regressão logística e multinominal.
RESULTADOS: a população do estudo foi constituída por 1596 mulheres de 18 a 49 anos de idade residentes em todas as regiões do país, das quais 22% usavam LARC. Os aspectos associados ao uso de LARC foram a idade mais jovem, ter plano de saúde, estar em um relacionamento e não querer engravidar. Metade das usuárias de LARC relatou ter algum tipo de preocupação com o método, sendo a mais frequente o risco de engravidar (36,2%). Os aspectos associados a ter preocupação com o uso de LARC foram o tipo de método, não estar em um relacionamento e não querer engravidar.
CONCLUSÕES: observou-se que as usuárias de LARC não são homogêneas entre si e que a experiência com o uso de LARC está permeada por preocupações, inclusive em relação a sua eficácia.
Palavras-chave:
Saúde sexual e reprodutiva, Contracepção reversível de longo prazo, Dispositivos intrauterinos
IntroductionThe use of contraceptive methods in Brazil has been concentrated in two short-acting methods, which are the oral contraceptive pill and male condom, besides female sterilization.
1 Although national surveys had demonstrated a relative dynamicity in the Brazilian contraceptive mix, with the decrease of tubal ligation and increase of the proportion of women that report the use of injectable methods,
2,3 the use of long-acting reversible contraception (LARC) methods is still low in the Brazilian scenario.
1The LARC are a category of contraceptive methods that do not demand monthly management, offer protection for at least three years in a single intervention, are highly effective and depend on qualified health professionals for their insertion and handling.
4 Both subdermal implants and copper and hormonal intrauterine devices (IUD) are part of the LARC group. Although the copper IUD is available in primary healthcare facilities of the Unified Health System (SUS – Portuguese acronym), hormonal IUDs and implants are available on SUS only occasionally. The implant, for example, is acquired by health secretariats of some municipalities and available only when certain criteria are met, such as being on social vulnerability or being user of illicit drugs.
5 These restrictions lead many women to purchase these methods, and, consequently, to count on professionals of the supplemental health system or of the private network to insert them, which increases even more their cost and diminish their availability for most Brazilian women.
6LARC users, in general, are the most satisfied within the users of contraceptive methods.
7,8 Nevertheless, the fact of being satisfied does not suppress concerns with the method. Surveys that assess concerns regarding LARC use are mostly carried out with women that are not current users. In addition, many of them consider only IUD, which leads the knowledge about the experience with the use of implants to be incipient in the country. At any rate, such studies demonstrate the increase of bleeding, the increase of cramps, infertility, painful removal of the method and side effects as the main concerns of women with regard to LARC.
9-12 Still, the side effects are broadly reported by LARC users and are related to its discontinuation in the first year of use.
13,14Since they are underutilized in the country, not reaching 2% of women,
1 little is known about the factors associated with their use, and principally, about the concerns that users have when using such methods, mainly the subdermal implant. Due to these reasons, this study aimed to determine factors associated with the use of long-acting reversible contraception (LARC) methods and with the concerns of users.
MethodsCross-sectional quantitative study, part of a broader survey that aimed to validate a measurement scale of the prospective intention of becoming pregnant. The methodological procedures of the validation study are based on a study with the same objective carried out in the United Kingdom, including the sample size calculation.
15 Both in United Kingdom and in Brazil, it was attempted to obtain the participation of 1000 women, in order to reach a minimum of 20 women per item of the scale, and perform specific statistics for the evaluation of their psychometric properties.
A broader study was carried out in a virtual environment with women from 18 to 49 years of age, non-pregnant, non-hysterectomized, non-sterilized and whose partners were not vasectomized. The survey was published between April and June 2021 in social networks (WhatsApp, Facebook, Instagram), in a website created by the researchers, in a university journal and via email, considering the list of contacts of the institution that houses the survey. In the propagation of the survey, besides the general information on the objective and procedures of the study, we also provided a link with access to the tool.
The structured tool was built in the REDCap platform and it was pre-tested in person and remotely with women of the same profile as those eligible.The first part of the tool contained questions concerning sociodemographic profile and reproductive history; the second, contained questions about reproductive intention and contraceptive behavior. The time spent for fulfilling the tool was around 15 minutes. In order to avoid multiple participation by the same woman, we also obtained their full names, email and phone number, which were checked to assure the internal validity of data. Information on identification was suppressed from the database for the statistical analyses.
Data were analyzed with Stata 17.0 software. Firstly, we performed a comparison between the sociodemographic profile and reproductive history between women that did not use any method, those who used LARC (subdermal implant, hormonal IUD and copper IUD) and those who used other methods (pills, injection, condoms and behavioral methods) by means of the chi-square test for difference of proportions. In case of a given category having less than five answers, we used the Fisher’s Exact Test.
Since part of the analysis considered only women that were LARC users, the post-hoc statistical power testwas calculated,
16 which was 93.6%. Aspects associated with LARC use were analyzed by multiple logistic regression in two models: the first one compared LARC users with users of other methods, and the second one compared LARC users with women that did not use contraceptive methods. The independent variables were: age, race/color, macro-region of residence, economic group,
17 complete high school, religion, current job, access to private health insurance, intention of becoming pregnant (defined with the question “Would you like to become pregnant next year?”), relationship (defined with the question “Are you currently in a [romantic] relationship with someone?”) and previous pregnancy. Adjusted odds ratio (OR) are presented, observing that the variables were inserted simultaneously in the models.
Posteriorly, women who reported using LARC were compared with regard to their sociodemographic and reproductive profile according to the method used (subdermal implant, hormonal IUD and copper IUD) by means of the chi-square test for difference of proportions. Due to the small number of women who reported using LARC, we opted not to perform any multiple logistic regression.
The concern with the use of contraceptive methods was assessed by means of the question “Do you have any concern with your contraceptive method?”, with answer options “no” and “yes”. For women that responded affirmatively, we asked “What are your concerns about your contraceptive method?”. The answer options had 14 items of multiple choice: no worry at all; risk of becoming pregnant; pain during menstruation; if I am using correctly; weight gain; irregular/escape bleeding; effects on my humor; abundant bleeding; acne; taking hormones; interference on the level of pleasure with sex; and headache. The average number of concerns and type of concern were described according to the type of LARC and compared by the chi-square test for difference of proportions. Aspects associated with being concerned with the contraceptive method used among LARC users were analyzed by means of multiple binomial logistic regression. The main independent variable was the type of LARC used. The other independent variables were the same considered in the previous models. Crude and adjusted OR are presented; the variables were simultaneously inserted in the model.
The study was approved by the Research Ethics Committee on 09/01/2020 (4.252.351). The Free and Informed Consent Form was made available on the website of the study and only women who clicked the “accept” icon were able to answer the questions. All procedures that ensure the confidentiality of data and women were performed. We also provided an email address for contact in case of doubt, and a website with every information on the research, in addition to links for information on contraception and reproductive health.
ResultsAltogether, 2070 women accessed the questionnaire, but only data from 1596 were considered, since some of them did not meet the inclusion criteria, for not having had sexual relationship (n=102), for being hysterectomized (n=29), for being pregnant (n=41), for being out of the age range (n=10) or having tubal ligation/vasectomized partner (n=4). The others did not fill thequestionnaire (n=288) and were then not considered in the study.
Of the 1596 women who participated in the study, most had completed high school (65.5%), reported being white (64.7%), to be on the socioeconomic group B (58.1%), to have health insurance (68.1%) and not wanting to become pregnant in the future (72.8%). There were respondents from all macro-regions of the country (Table 1).
A little more than one fifth of women used LARC (22.0%), whilst 27.9% did not use any method and the rest (50.1%) used other methods (26.8% used contraceptive pills, 18.5% male condom, 1.6% injectable contraceptives and 4.8% behavioral methods). There was a statistically significant difference between LARC users, users of other methods or no method concerning age (
p<0.001), religion (
p=0.023), having health insurance (
p=0.002), region of residence (
p=0.013), being in a relationship (
p<0.001), previous pregnancy (
p<0.001), number of children (
p=0.020) and future intention of becoming pregnant (
p<0.001) (Table 1).
Compared to women who used other contraceptive methods, LARC users were more likely to have health insurance, to be in a relationship and to have become pregnant previously; and less likely to be 35-49 years of age and to want to have children or not being sure about this. Compared to women who did not use contraceptive methods, LARC users were more likely to have health insurance and to be in a relationship. In turn, they were less likely to be 35-49 years-old and to want to have children or not being sure about this (Table 2).
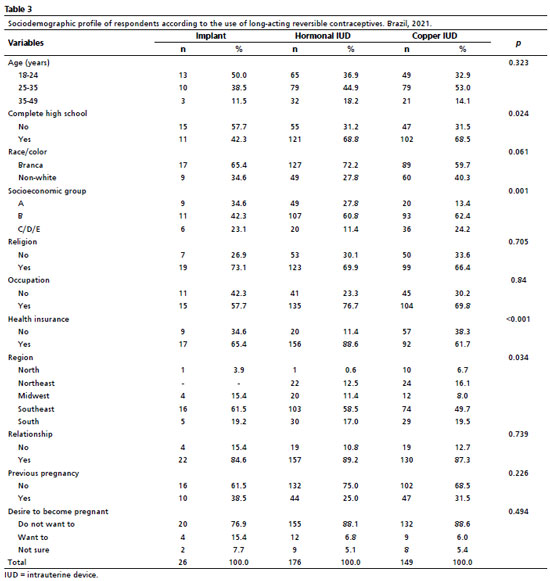
Considering only LARC users (n=351), we observed a statistically significant difference in their sociodemographic and reproductive profiles in relation to have complete high school (
p=0.024), to the socioeconomic group (
p=0.001), to have health insurance (
p<0.001) and to the macro-region of residence (Table 3).
Almost half of LARC users reported some kind of concern with the method (48.7%; n=171).Hormonal IUD users were those who most reported some kind of concern (54.0%), whilst subdermal implant users were those who reported less concerns (23.1%). Among copper IUD users, almost half of them reported having concerns when using the method (47.0%). Among the ten categories that composed the question about concern, implant users reported, on average, 0.7 concerns (SD= 1.7); hormonal IUD users reported 1.7 (SD= 2.2) and copper IUD users, 1.1 (SD= 1.5) (data not shown in Table). Among implant users, the most frequent concern was related to weight gain. Among hormonal and copper IUD users, the most frequent concern was related to the risk of becoming pregnant; however, within hormonal IUD users, irregular bleeding and acne were the most reported subsequent concerns, whilst heavy menstrual bleeding and menstrual cramps were the most reported subsequent concerns within copper IUD users (Table 4).
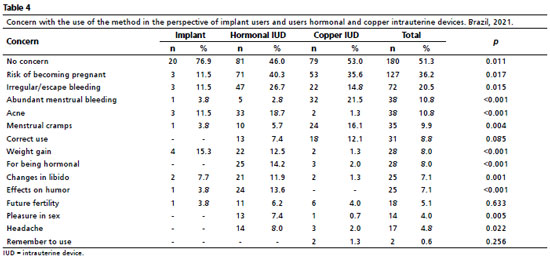
The aspects associated with being concerned about the use of the method within LARC users were type of method, being in a relationship and wanting to become pregnant (Table 5).
DiscussionThis study was fully conducted in a digital environment with women of reproductive age residing in all macro-regions of the country. We observed that a fifth of them used LARC. The age, access to private health insurance, relationship and desire of becoming pregnant were determinants for women to use such methods. The concerns with the use of these methods was broadly reported, but less frequently by users of subdermal implants. The type of method was a crucial element for the report of concerns with the use, as well asthe relationship and the desire of becoming pregnant.
In Brazil, LARC users still access the implant and hormonal IUD almost only from private services or at the supplementary health system. This condition certainly has similarities to the profile of users described in the study: white women with better schooling, residing mainly in the South and Southeast regions of the country, mostly belonging to socioeconomic groups A and B and who have health insurance. However, another part of the LARC users is composed of women who accessed the method for being in extreme social vulnerability and probably underrepresented in our study population.
The lack of availability of these devices in a broad and universal way at SUS is one of the elements that produce the differentiated profile of women with access to these birth control technologies. This phenomenon is being described by some authors as a form of “contraceptive coercion”,
18 since it reproduces a “selective offer” of LARC devices to certain women and fragments the universality and integrality paradigm, principles that guided for decades the public health policies for women inthe country.
6 The methodological strategy adopted allowed us to reach, mostly, LARC users that are on the top of the social pyramid, which reinforces the fact that our results should not be generalized.
It is important mentioning that the copper IUD is part of the contraceptive mix offered by SUS since before the promulgation of the Familiar Planning Law, in 1996.
19 However, the prevalence of its use have always appeared timidly on the national surveys: in the National Demographic Health Survey, of 2006, for example, 4.5% of women had already used copper IUD once, a very low percentage compared to contraceptive pill or tubal ligation.
20 In the same study, implants reached 0.4%. The National Health Survey of 2013, in turn, did not differentiate copper IUD from hormonal IUD.
1The absence of such data does not allow us to affirm changes in the prevalence of the use of this method, although it is part of the contraceptive mix available in SUS for decades. It is worth noting, however, subtle differences of profile in relation to implant users and hormone IUD users, mainly concerning the condition of “having health insurance”, observing the restrictions on its availability on public health services.
Documents, protocols and clinical guidelines emphasize with great enthusiasm the high effectiveness and reliability of LARCs as elements that make them first choice methods.
21 However, a variety of questions/situations experienced by women that use LARC has been poorly represented in studies on contraceptive practices. This study evidences that the real experience of many users is actually permeated by concerns, including with regard to the effectiveness and reliability of the method, also in relation to its countless side effects. Thus, the proportion of women that discontinue the use of the method right in the first year do not seem occasional for us, mainly due to discomforts and side effects that it can cause.
13,14,22The present study did not ask explicitly about possible side effects caused by the method in use; alternatively, we opted to ask about the main concerns of users with regard to the method they were using, which provide evidence on the reasons that may eventually contribute to its discontinuation. The results show, for example, that the concerns with irregular bleeding are more frequent among hormonal IUD users, whilst abundant menstrual bleeding concerns copper IUD users. Assuredly, the changes on menstrual standards that LARC users experience are a frequent source of concern and need to be considered in the contraceptive counseling and management.
23 These are dimensions that have been pointed as important aspects in the method discontinuation, mainly the hormonal ones, both long and short acting.
23,24We conclude that users of implant reported less concerns with the method and seemed to feelsafe with regard to its effectiveness and reliability.
Furthermore, our results confirm that LARC users differentiate from each other in relation to the concerns they have with the method, depending on the type of method used, which implies that they should not be seen as homogeneous in the contraceptive care nor in studieson contraceptive practices.
25 Neither should the LARCS be published as they were similar to each other – however they are in efficacy rates – observing that they have different mechanisms of action, different side effects and different manners of insertion.
26The advantages of online surveys are countless, such as quickness of execution, broadness and low cost, aspects that were largely discussed due to the COVID-19 pandemic.
27 However, this methodological resource brings, in the same way, several limitations concerning the data produced. For example, it is not possible to know the range, in terms of broadness and profile of the public reached by the invitation that was published in social networks. It is known that the internet coverage is highly diversified, that is, the availability and quality are inversely proportional to socioeconomic status.
28 There are both a selection bias and an impossibility of calculating the denial in participating in the study: the participants of the study may have be interested in answering the questionnaire precisely because they have some relation with the subject of the survey, an aspect that may largely affect the measures of association and distribution of the phenomenon. Even more so, questions such as representativeness and generalization of data cannot be calculated from websurveys.
The present study contributes to the advance in the field of sexual and reproductive health when incorporating users of subdermal implants, who are rarelyconsidered in studies about reproductive planning in the country. In addition, it highlights the differences among LARC users according to their sociodemographic profile and analyzes their countless concerns regarding the use of these methods. The high levels of satisfaction with LARCs cannot overshadow the fact that some women are concerned about using them, including with regard to its effectiveness and safety.
While recent national surveys on prevalence of the use of these methods in Brazil are not available, there is no doubt that an expansion in LARC offer has been occurring, either by the private or supplementary health market, or in a selective manner by public health services, focusing on specific profiles of users. There is an exacerbation of LARCs efficacy, reinforced in pharmaceutical industry advertisement and in discourses of several medical associations, with expressions like “use it or forget it” or “contraceptive without complications”.
29 Nevertheless, during the process of counseling, such euphoria cannot obfuscate the possible side effects that such methods could cause to women and how to deal with them, in order to avoid, mainly, their discontinuation; otherwise the use of another method could bring more advantages.
We concluded that women that used LARC were diverse among each other, both in sociodemographic and in reproductive history and with regard to the concerns they had about the method. While such methods are highly effective, many users reported concerns with the risk of pregnancy. Changes in the standard of menstrual bleeding induced by the use of the method also stood out as the main concerns.
We reinforce that efforts should be taken so that women and men are able to reach their rights to reproductive autonomy and self-determination, amplifying the capability and freedom to decide if, when and how many times they want to become pregnant/reproduce. The right to adequate information, as well as access to effective and safe contraceptive methods are angular dimensions for the implementation of reproductive rights, which should be offered to all citizens of reproductive age. This is an attitude that safeguards the expansion of the contraceptive mix, as well as the guarantee to its universal and free access by SUS.
AcknowledgmentsWe would like to thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 for financial support.
References1. Trindade RE, Siqueira BB, Paula TF, Felisbino-Mendes MS. Uso de contracepção e desigualdades do planejamento reprodutivo das mulheres brasileiras. Ciênc Saúde Colet. 2021; 26 (Suppl. 2): 3493-504.
2. Cavenaghi S, Diniz Alves JE. O mix contraceptivo eternamente obsoleto no Brasil e seu legado. Rev Bras Est Pop. 2019; 36: 1-29.
3. Lago TG, Kalckmann S, Alves MCGP. Diferenciais da prática contraceptiva no Município de São Paulo, Brasil: resultados do inquérito populacional Ouvindo Mulheres. Cad Saúde Pública. 2020; 36 (10): e00096919.
4. World Health Organization (WHO). Medical eligibility criteria for contraceptive use [
Internet]. Geneva: WHO; 2015. [access in 2022 Out 10]. Available from:
https://apps.who.int/iris/bitstream/handle/10665/181468/9789241549158_eng.pdf5. Ministério da Saúde (BR). Secretaria de Ciência, Tecnologia, Inovação e Insumos Estratégicos em Saúde. Portaria SCTIE/MS nº 13, de 19 de abril de 2021. Torna pública a decisão de incorporar o implante subdérmico de etonogestrel, condicionada à criação de programa específico, na prevenção da gravidez não planejada para mulheres em idade fértil: em situação de rua; com HIV/AIDS em uso de dolutegravir; em uso de talidomida; privadas de liberdade; trabalhadoras do sexo; e em tratamento de tuberculose em uso de aminoglicosídeos, no âmbito do Sistema Único de Saúde – SUS [
Internet]. Brasília (DF): Ministério da Saúde; 2021. [access in 2023 Jan 10]. Available from:
https://www.in.gov.br/en/web/dou/-/portaria-sctie/ms-n-13-de-19-de-abril-de-2021-3151842196. Brandão ER, Cabral CS. Vidas precárias: tecnologias de governo e modos de gestão da fecundidade de mulheres “vulneráveis”. Horiz Antropol. 2021; 27 (61): 47-84.
7. Borges ALV, Santos AO, Araújo KS, Gonçalves RFS, Rosa PLFS, Nascimento NC. Satisfaction with the use of contraceptive methods among women from primary health care services in the city of São Paulo, Brazil. Rev Bras Saúde Mater Infant. 2017; 17 (4): 749-56.
8. Apter D, Briggs P, Tuppurainen M, Grunert J, Lukkari-Lax E, Rybowski S,
et al. A 12-month multicenter, randomized study comparing the levonorgestrel intrauterine system with the etonogestrel subdermal implant. Fertil Steril. 2016; 106 (1): 151-75.
9. Bameka A, Kakaire O, Kaye DK, Namusoke F. Early discontinuation of long-acting reversible contraceptives and associated factors among women discontinuing long-acting reversible contraceptives at national referral hospital, Kampala-Uganda; a cross-sectional study. Contracept Reprod. Med. 2023; 8 (1): 27.
10. Zimmerman L, Sarnak DO, Karp C, Association between experience of specific side-effects and contraceptive switching and discontinuation in Uganda: results from a longitudinal study. Reprod Health. 2021; 18: 239.
11. Stanton T, Cizek S, Tyson N. Adolescents and long-acting reversible contraceptives: beyond the basics. Curr Opin Obstet Gynecol. 2020; 32 (6): 416-23.
12. Svahn S, Hultstrand JN, Tydén T, Ragnar ME. Contraception use and attitudes: women’s concerns regarding hormonal contraception and copper intrauterine devices. Eur J Contracept Reprod Health Care. 2021; 26 (6): 473-78.
13. Wahab NA, Rahman NA, Mustafa KB, Awang M, Sidek AA, Ros RM. A clinical evaluation of bleeding patterns, adverse effects, and satisfaction with the subdermal etonogestrel implant among postpartum and non-postpartum users. Int J Gynaecol Obstet. 2016; 132 (2): 237-8.
14. Polis CB, Hussain R, Berry A. There might be blood: a scoping review on women’s responses to contraceptive-induced menstrual bleeding changes. Reprod Health. 2018; 15: 114.
15. Hall J, Barrett G, Rocca C. Evaluation of the Desire to Avoid Pregnancy Scale in the UK: a psychometric analysis including predictive validity. BMJ Open. 2022; 12 (7): e060287.
16. Flahault A, Cadilhac M, Thomas G. Sample size calculation should be performed for design accuracy in diagnostic test studies. J Clin Epidemiol. 2005; 58: 859-62.
17. Associação Brasileira de Empresas de Pesquisa (ABEP). Critério Brasil 2019 [
Internet]. São Paulo: ABEP; 2019. [access in 2023 Jan 10]. Available from:
http://www.abep.org/criterio-brasil.18. Senderowicz L. “I was obligated to accept”: A qualitative exploration of contraceptive coercion. Soc Sci Med. 2019; 239: 112531.
19. Sociedade Civil Bem-Estar Familiar no Brasil (BEMFAM). Pesquisa Nacional sobre Demografia e Saúde 1996. Rio de Janeiro: BEMFAM; 1997. [access in 2023 Jan 10]. Available from:
https://dhsprogram.com/pubs/pdf/fr77/fr77.pdf20. Ministério da Saúde (BR). Centro Brasileiro de Análise e Planejamento. Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher – PNDS 2006: dimensões do processo reprodutivo e da saúde da criança. Brasília (DF): Ministério da Saúde; 2009. [access in 2023 Jan 10]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/pnds_crianca_mulher.pdf21. Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Persp Sex Reprod Health. 2014; 46 (3): 171-5.
22. Sznajder KK, Tomaszewski KS, Burke AE, Trent M. Incidence of discontinuation of long-acting reversible contraception among adolescent and young adult women served by an urban primary care clinic. J Pediatr Adolesc Gynecol. 2017; 30 (1): 53-7.
23. Zimmerman LA, Sarnak DO, Karp C, Wood SN, Yihdego M, Shiferaw S,
et al. Measuring experiences and concerns surrounding contraceptive induced side-effects in a nationally representative sample of contraceptive users: evidence from PMA Ethiopia. Contraception X. 2022 Mar; 4: 100074.
24. Borges ALV, Chofakian CBN, Viana AO, Divino EA. Descontinuidades contraceptivas no uso do contraceptivo hormonal oral, injetável e do preservativo masculino. Cad Saúde Pública. 2021; 37 (2): e00014220.
25. Laporte M, Metelus S, Ali M, Bahamondes L. Major differences in the characteristics of users of the copper intrauterine device or levonorgestrel intrauterine system at a clinic in Campinas, Brazil. Int J Gynecol Obstet. 2022; 156: 240-6.
26. Manzer JL, Berndt VK, Bell AV. Comparing methods of long-acting reversible contraception: A qualitative study of Delaware women’s perceptions of intrauterine devices and the implant. Contraception. 2022; 113: 73-7.
27. De Boni, Raquel B. Websurveys nos tempos de COVID-19. Cad Saúde Pública. 2020; 36 (7): e00155820.
28. Centro Regional de Estudos para o Desenvolvimento da Sociedade da Informação (CETIC). Pesquisa sobre o uso das tecnologias de informação e comunicação nos domicílios brasileiros: TIC Domicílios 2021. [editor] Núcleo de Informação e Coordenação do Ponto BR. 1
st. ed. São Paulo: Comitê Gestor da Internet no Brasil; 2022. [access in 2023 Jan 10]. Available from:
https://cetic.br/media/docs/publicacoes/2/20221121125504/tic_domicilios_2021_livro_eletronico.pdf29. Coutinho do Nascimento NN, Reis Brandão E. Long-Acting Reversible Contraception (LARC): análise das controvérsias que cercam sua circulação no Sistema Único de Saúde no Brasil. Rev Encuentros Latinoamericanos. 2021; 5 (2): 17-41.
Author’s contributionBorges ALV: conceptualization of the proposal of the article, data analysis and interpretation, writing and review of the manuscript. Chofakian CBN: data analysis and interpretation, writing and review of the manuscript. Ale CCS and Cabral CS: writing and review of the manuscript. All authors approve the final version of the article and declare no conflicts of interest.
Received on February 28, 2023
Final version presented on June 28, 2024
Approved on July 3, 2024
Associated Editor: Sheyla Costa
 ; Christiane Borges do Nascimento Chofakian 2
; Christiane Borges do Nascimento Chofakian 2 ; Carolina Cavalcante da Silva Ale 3
; Carolina Cavalcante da Silva Ale 3 ; Cristiane da Silva Cabral 4
; Cristiane da Silva Cabral 4