ABSTRACT
OBJECTIVES: verify the factors associated with parental stress in Neonatal Intensive Care Unit (Neonatal ICU) of small municipalities.
METHODS: cross-sectional quantitative study, with parents of newborns admitted in the neonatal ICU in two philanthropic hospitals. The instruments used were the Parental Stress Scale: Neonatal ICU and Perceptions of Family-Centered Care – Parents. The analysis was performed according to the nature of the distribution of the variables.
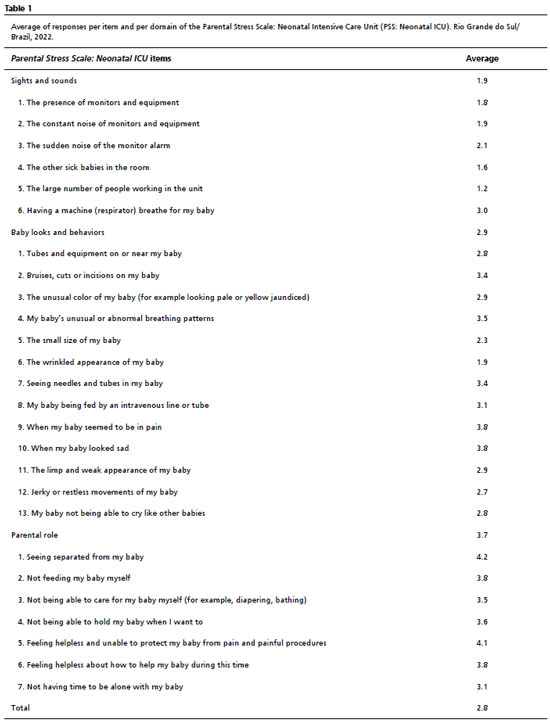
RESULTS: of the 129 volunteers, 79.8% showed parental stress. The averages of stress in the domains “sights and sounds”, “baby looks and behaviors” and “alteration in the mother/father role” was observed, respectively, 1.9, 2.9 and 3.7 in Parental Stress Scale: Neonatal ICU. There was a significant association between the gender of the participants (p=0.0182) and clinical complications during the period of hospitalization (p= 0.0443) with parental stress. A difference was observed in the groups of the variable “hospitalization time to the moment of the data collection” (p= 0.0112), in the domains “respect” (p=0.0266), “collaboration” (p=0.0060) and in the total sum (p= 0.0112) of the Perceptions of Family-Centered Care – Parents scale.
CONCLUSION: parental stress was associated with changes in the role of the mother/father; with the mothers and the occurrence of clinical complications with the baby during its hospitalization.
Keywords:
Neonatal ICU, Newborn, Parenting, Psychological stress, Professional-family relations, Integrative health care
RESUMO
OBJETIVOS: verificar fatores associados ao estresse parental em Unidade de Terapia Intensiva Neonatal (UTI Neonatal) de pequenos municípios.
MÉTODOS: estudo quantitativo transversal, com pais de recém-nascidos internados em UTI Neonatal de dois hospitais filantrópicos. Os instrumentos utilizados foram Parental Stress Scale: Neonatal ICU e Percepção do Cuidado Centrado na Família - Pais. A análise foi realizada de acordo com a natureza de distribuição das variáveis.
RESULTADOS: de 129 voluntários, 79,8% apresentaram estresse parental. As médias de estresse nos domínios “sons e imagens”, “aparência e comportamento do bebê” e “alteração no papel da mãe/pai” observadas foram, respectivamente, 1,9, 2,9 e 3,7 na Parental Stress Scale: Neonatal ICU. Houve associação significativa entre gênero dos participantes (p=0,018) e intercorrências clínicas durante a hospitalização (p=0,044) com estresse parental. Observou-se diferença nos grupos na variável “tempo de internação até o momento da coleta de dados” (p=0,011), nos domínios “respeito” (p=0,026), “colaboração” (p=0,006) e na soma total (p= 0,011) da escala Percepção do Cuidado Centrado na Família - Pais.
CONCLUSÃO: estresse parental esteve associado à alteração no papel de mãe/pai; às mães e à ocorrência de intercorrências clínicas com o bebê durante sua hospitalização.
Palavras-chave:
UTI neonatal, Recém-nascido, Parentalidade, Estresse psicológico, Relações profissional-família, Assistência integral à saúde
IntroductionEvery year, around 64 to 80 of 1000 live newborns (NB) in the world require intensive care in a neonatal intensive care unit (Neonatal ICU).
1 The hospitalization of NBs in the neonatal ICU may cause emotional and health changes also in their parents.
2 Some stress factors present at the neonatal ICU, according to the parents' conception, are the noise, the alternation of light and shade, the presence of tubes and equipment, the babies' fragile appearance,
3 the functions and empathy of the multi-professional team, the need for communication and information, the fear of death of the NB, the feelings of guilt and shame, and the separation from their child.
4-6 In addition to this, the baby care is performed by the health team, making parents feel like spectators, compromising the recognition of the mother and father roles, which, added to the stress caused by the environment, can negatively interfere in bonding with the baby and in its development.
7,8The parents' participation in the neonatal ICU is very important since their stay is associated with improvement in the baby's neurodevelopment, besides optimizing the parental relationship and improving the perception of stress in the Neonatal ICU.
9 Despite the existence of Law Nº 13,257 of 2016, in Brazil, which addresses public policies for early childhood and regulates that neonatal ICU should provide conditions for the father, mother or another responsible person to remain full-time during the baby's hospitalization, there are still many obstacles in fulfilling this right.
10The care of newborns should include the family and their needs, as recommended by the Family Centered Care (FCC).
5,11 Some measures that optimize the assistance are the guarantee of free access of parents at the neonatal ICU, respect for their values and beliefs, active listening and provision of complete and unbiased information about their baby and encouragement to participate in decision-making and to care for the baby.
11 These and other actions reflect the decrease of hospital stay, greater parental autonomy, qualification of the parents' perception regarding hospitalization and reduction of parental stress.
12 FCC, in recent years, has faced challenges in its incorporation due to the COVID-19 epidemiological situation, which brings numerous repercussions for both the inclusion of the family in care contexts and the parental stress experienced by parents and other family members.
13Although admission to a neonatal ICU is necessary in several cases and ensures the survival of the NB at risk, it is an environment with numerous stressful factors for both the baby and its family. The aim of this study was to verify the factors associated with parental stress in the neonatal ICU considering the context of FCC in two small to medium-sized municipalities.
MethodsThis is an observational, cross-sectional study with a quantitative approach. The participants of the study were fathers and mothers of newborns admitted to a neonatal ICU who had attended the unit at least three times before the data collection. The chosen participation interval was between 5 and 15 days of the baby's hospitalization. The lower limit of hospitalization days was considered so that parents could have experiences within the neonatal ICU context to respond to the proposed instruments, and the upper limit was set to give homogeneity to the participants.
Parents of newborns admitted directly to a conventional or kangaroo intermediate care unit were excluded, as were those under 18 years of age at the time of the invitation to participate in the study or those who did not have cognitive conditions to answer the data collection instrument, as considered by the health team. The population comprised all eligible fathers and mothers of newborns admitted to the neonatal ICU of two institutions during the survey period.
Data collection occurred from May to October 2021, in two hospitals in the South of Brazil, both philanthropic, with ten neonatal ICU beds each. The institutions were chosen based on the geographical availability of the researchers. Hospital A serves patients from 22 municipalities in the Northwest region of the state. It has 155 inpatient beds and three intensive care units (adult, pediatric, and neonatal). Hospital B is part of one of the largest hospital complexes in the Northern region of the state. It is a reference center for the Northern macro-region of the state for the SUS (Portuguese acronym for Unified Health System), covering 158 municipalities and serving a population of approximately 1,600,000 inhabitants. At hospital A, fathers and mothers were allowed to remain in the neonatal ICU full-time, except for the change of shifts of the staff and in some procedures. Meanwhile, at hospital B, the parents' stay took place in a visitation system, twice per shift, one hour each. The visiting routines at both hospitals were not changed during the pandemic. First, the eligible participants were selected by telephone, through the contacts listed in the institutions' registration system, and invited to participate in the research. Subsequently, the collection instruments were sent, via WhatsApp application, to the fathers and mothers who agreed to participate, in a digital version. In this electronic form, which was answered online, the first section contained the informed consent (IC). The rest of the form could only be accessed if the participant agreed to the IC. After filling out the instruments, the answers were automatically sent to the email of the researchers. The data collection occurred entirely virtually, justified by the intensification of infections by COVID-19, and it was carried out by a team of trained academics and residents.
The questionnaires used were Parental Stress Scale: Neonatal Intensive Care Unit (PSS: Neonatal ICU) and Perception of Family-Centered Care - Parents Brazilian version (PCCF-P Brazilian version), both of them validated and translated into Brazilian Portuguese,
14,15 as well as an instrument for characterisation of the participants, obstetric and newborn data, produced by the authors. The PSS: Neonatal ICU
16 aims to assess the perception of parents regarding the stressful factors present in the physical and psychosocial environments of the neonatal ICU. The instrument is of the Likert type, with scores from 1 to 5, where 1 refers to “not stressful” and 5 to “extremely stressful”. There is still the option “not applicable”. The metric “1” and the cut-off point “2” were considered to divide the groups into “With stress” (score equal to or higher than 2) and “Without stress” (score lower than 2).
5The PCCF-P is a scale of perception of FCC for parents and aims to measure and compare parents' perspectives on FCC in different paediatric contexts.
17 This measurement scale is also of the Likert type, with four alternative answers for each question: 1 - never, 2 - sometimes, 3 - generally and 4 – always.
15 The quantification of the answers varies from 20 and 80, and the higher the sum value, the more positive the parents' perception.
18Qualitative variables were presented by absolute and relative frequencies. Simple crossings of qualitative variables were performed and, to verify the association between them, the measure “Odds Ratio” (OR) and its confidence interval were used. The analysis was performed using the Statistica 9.1 software, and the significance level was considered to be
p≤0.05. Quantitative variables were presented by mean (± standard deviation), median, minimum and maximum. This study was approved by the Research Ethics Committee of a Public Higher Education Institution, CAAE 43938621.8.0000.5346, in April 2021, and by the institutions where the collections took place.
ResultsThe study included 129 volunteers, 62.8% of whom were mothers, with an average age of 29 (± 6.1) years and an age range between 20 and 46 years. The predominance was of parents who had completed high school (43.4%) as maximum education and who did not reside in the city where their newborn was hospitalized (62.8%). Regarding the daily parental stay at the neonatal ICU, the period ranged from 30 minutes to 16 hours, with an average of 3.7 (±3.3) hours. Regarding the parents' perception of this time at the neonatal ICU, 48.8% of the participants said they considered it “little”.
Considering the obstetric data, 53.4% were high-risk pregnancies, 65.1% had obstetric complications and 97.6% of women had prenatal care. Complications include pre-eclampsia, thrombophilia, diabetes, placental abruption, fetal centralisation and hypothyroidism.
Regarding the neonates, the average length of stay in neonatal ICU up to the time of data collection was 8 days, predominantly male newborns (68.9%), moderate and late premature (68.9%), the average weight of 2.1 kg and birth by caesarean section (80.0%). The main causes of admission to the neonatal ICU were prematurity and respiratory distress (60.0%), 75.5% had clinical complications during the period they stayed in the unit and 95.5% used some type of device. Furthermore, 78.9% were not using ventilatory support at the time of data collection, but 65.5% of them had already used it during hospitalization.
Among the participants, 79.8% showed stress. A descriptive analysis of the PSS: Neonatal ICU was performed. The results are shown in Table 1. In the domain “sights and sounds”, the most stressful situations, in the perception of parents, were “Having a machine (respirator) breathe for my baby” (average 3.0) and “The sudden noise of the monitor alarm” (average 2.1). In the domain “baby looks and behaviors”, the items that received the highest scores in this category were “When my baby seemed to be in pain” (mean 3.8) and “When my baby looked sad” (mean 3.8). As for the domain “Alteration in the role of mother/father”, the factors indicated as the most stressful were “Being separated from my baby” (average 4.2) and “Feeling helpless and unable to protect my baby from pain and painful procedures” (average 4.1).
Associations were made between variables of characterisation of the participants, and obstetric and neonatal data with the PSS: Neonatal ICU instrument. The results are shown in Table 2. It was observed that only two variables showed a significant association with parental stress: the gender of participants and clinical complications of newborns during the period of stay at the neonatal ICU. Parental stress is significantly (
p=0.0182) higher, with a chance of almost 3 times, in mothers, compared to fathers. Moreover, the presence of clinical complications affecting the baby during the stay at the neonatal ICU led to a 2.6 times greater chance of occurrence of parental stress in participants (
p= 0.0443).
The quantitative variables were also analyzed. Their averages (±standard deviation) and medians are shown in Table 3. Figure 1 shows the sum obtained by each participant in the scale PCCF-P Brazilian version for each group of the PSS: Neonatal ICU. It is observed that there was a difference between the groups in the PCCF-P domains “respect” (
p=0.0266) and “collaboration” (
p=0.0060), as well as in the total sum (
p=0.0112) of the instrument, in which a concentration of answers in the highest scores was observed in the “without stress” group. Furthermore, “time of hospitalization until the moment of data collection” (
p=0.0112) also revealed a difference between the groups.
DiscussionParental stress in the neonatal ICU was associated with changes in the role of the mother/father; the gender of the participants and the occurrence of clinical complications with the baby during hospitalization. A difference was observed in the groups of the variable “hospitalization time to the moment of the data collection”, in the domains “respect”, “collaboration” and in the total sum of the Perceptions of Family-Centered Care – Parents scale.
As shown in the analysis of the PSS: Neonatal ICU, the domain with the highest average was “Alteration in the role of mother/father”, whose factors indicated as the most stressful were “Being separated from my baby” and “Feeling helpless and unable to protect my baby from pain and painful procedures”, similarly to studies that point to the same results.
19,20The separation between parents and babies imposed by the neonatal ICU environment is considered one of the main sources of stress, because parents feel overwhelmed and powerless, besides the fact that babies receive little support and parental interaction.
21 During hospitalization, parents transfer the care of their children to health professionals, evidencing the separation from the baby and the difficulty of being part of the service and living their parental functions.
4,19,22 During the baby's hospitalization, the opportunities for parents' involvement in childcare are limited. This restricted access of parents to their role as caregivers directly interferes with their affective and psychological well-being, in addition to affecting the establishment of affective bonds.
3 The high level of stress can be minimized with the support of the healthcare team, incorporating FCC methodologies and optimizing the parents' participation in the care process.
11Child hospitalization, regardless of the child's age, is directly related to parental presence. However, in the scenario of intensive care, this situation is challenging due to the high complexity of the procedures performed and due to the reduced visiting hours still existing in some units,
23 as well as in one of the institutions analyzed in this study. A study conducted in Finland in 2015 found an average stay of 9.7 hours, mainly during the day. It also showed that the units that allowed parents to stay overnight, the length of stay was higher.
24 According to the legislation, one of the units surveyed in this study allows parents to attend the neonatal ICU 24 hours a day, but the physical structure does not favor the overnight stay, due to limited space, insufficient comfort, among other obstacles.
Another conditioning factor that hindered the presence of parents during pediatric hospitalizations was the context of the COVID-19 pandemic. The FCC stands out as a care philosophy that promotes family participation in decisions and care for their loved ones. However, during the COVID-19 pandemic, there is a risk of regressing in the implementation of this approach due to concerns about the potential spread of the virus, which might distance the family from this context. It is crucial to reflect on each situation individually, as applying a one-size-fits-all rule would disrespect the uniqueness of each person and his or her family.
25Families should be seen not only in terms of restrictions on their entry and stay in the hospital, viewed as potential infection spreaders, but as partners in developing strategies and actions during this crisis, as well as planning future steps, including for potential future pandemics. These results also highlight the importance of FCC in reducing parental stress in the neonatal ICU.
26Parental stress is significantly higher in mothers, compared to fathers. A meta-analysis corroborates the present finding of the study, highlighting that admission to the neonatal ICU is more stressful for mothers than for fathers and can impact mental health and quality of life.
27 Mothers reported a higher combined prevalence of stress, anxiety, and depression than fathers, possibly attributable to their feelings about the birth of a sick child.
28This can be explained due to the several transformations experienced by women during pregnancy and puerperium, the role of primary caregivers that mothers have, besides usually spending more time at the neonatal ICU than fathers spend. In addition, fathers may have easier access to babies soon after birth due to returning to work earlier and mothers presenting higher perinatal risks. Another important factor is the limitation to breastfeeding, the most distressing situation for mothers.
3There is a 2.6 times more chance of stress occurring when there are clinical complications with the baby during the stay at the neonatal ICU. This situation is directly related to a higher risk of death, clinical instability, separation of parents and baby, parents' feelings of helplessness and insecurity, and increased NB hospitalization time, among other problems, which may explain the association with parental stress. The baby's clinical instability is related to less parental presence, lap and skin-to-skin contact in the neonatal ICU. When their child is on a mechanical ventilator or is clinically fragile, parents may feel less confident in their ability to provide care. On the other hand, there is greater participation of parents in the care of babies with fewer medical interventions.
9The “without stress” group showed a slightly longer average time, which may indicate that, as the days went by, the parents created a bond with the health team and developed greater confidence concerning the care. In addition, babies tend to become more clinically stable over time during their treatment, which leads to greater parental reassurance. It is related to the decrease in intensive care needs of the baby, making the parents feel increasingly like their child's primary caregivers, assuming their parental role. This occurs as they can participate more actively in breastfeeding, bathing, and holding their baby.
29Analyzing the quantitative variables, there was a concentration of answers in the highest scores in the “without stress” group in the domains “respect”, “collaboration” and in the total sum of the PCCF-P scale, which indicates that the better the parents' perception of FCC, the lower their levels of stress at the neonatal ICU. During the period of hospitalization of the NB at the neonatal ICU, parents need assistance, support, encouragement and guidance from the team.
9,21,25Studies show that the assistance aimed at the practice of FCC is strictly related to the mitigation of anxiety and parental stress and the enhancement of self-confidence and sense of assurance and control of parents, optimisation in the adherence to the kangaroo method, breastfeeding rates and the parent-baby bond, reduction in the time of hospitalization of the newborn and subsequent readmissions, in addition to integration with the health team.
24 Moreover, the newborn experiences a better adaptation to the extrauterine life, with better weight gain and regulation of vital signs.
A systematic review indicates that stress stemming from neonatal ICU environments has been correlated with Post-Traumatic Stress Disorder (PTSD) and anxiety. It also highlights that there is limited evidence suggesting that parental involvement and effective communication between parents and the healthcare team, adequate social support, and positive coping mechanisms can serve as protective factors for both PTSD and anxiety.
30This study presented as a limitation the fact that data collection occurred entirely virtually, justified by the intensification of infections by COVID-19. This situation may have excluded eligible participants who did not have a smartphone or WhatsApp application. Another limitation is the lack of formal data on the contamination of the studied population during this period in these institutions.
A potential strength of the study is the opportunity to raise awareness among professionals about the factors associated with parental stress in the neonatal ICU and to train them in FCC. Promoting actions that encourage parents to participate in the care of their babies and teaching them in a way that makes them feel confident in assuming their parental role is essential. Additionally, allowing and encouraging their full-time presence is crucial. This will generate greater bonding between parents and the team, between parents and babies, strengthening parental autonomy and assurance and having a positive impact on the reduction of parental stress and on child development in both medium and long term.
In future studies, we suggest looking more closely at the inclusion of the paternal figure and the cultural representation of the maternal figure. In addition, a differentiation between maternal stress in mothers of premature and full-term babies could be approached, as well as checking for differences between the pre- and post-pandemic periods.
References1. Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D,
et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health. 2019; 7 (1): e37-e46.
2. Silva ND, Linhares MB, Gaspardo CM. Developmental care approaches for mitigating stress in preterm neonates in the neonatal intensive care unit: A systematic review. Int J Psychol Neurosci. 2018 Jun; 11 (2): 117-31.
3. Caporali C, Pisoni C, Gasparini L, Ballante E, Zecca M, Orcesi S, Provenzi L. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. J Perinatol. 2020 Sep; 40 (12): 1739-52.
4. Abuidhail J, Al-Motlaq M, Mrayan L, Salameh T. The Lived Experience of Jordanian Parents in a Neonatal Intensive Care Unit. J Nurs Res. 2017 Apr; 25 (2): 156-62.
5. Kegler JJ, Neves ET, Silva AM, Oliveira DC, Zamberlan KC. Fatores associados ao estresse de pais em Unidade de Terapia Intensiva Neonatal. Acta Paul Enferm. 2023; 36: eAPE02061.
6. Ramos FP, Enumo SR, Paula KM. Maternal Coping with Baby Hospitalization at a Neonatal Intensive Care Unit. Paidéia (Ribeirão Preto). 2017 Ago; 27 (67): 10-9.
7. Veronez M, Borghesan NA, Corrêa DA, Higarashi IH. Vivência de mães de bebês prematuros do nascimento a alta: notas de diários de campo. Rev Gaucha Enferm. 2017; 38 (2): e60911.
8. Spinelli M, Frigerio A, Montali L, Fasolo M, Spada MS, Mangili G. ‘I still have difficulties feeling like a mother': The transition to motherhood of preterm infants mothers. Psychol Health. 2015 Out; 31 (2): 184-204.
9. Pineda R, Bender J, Hall B, Shabosky L, Annecca A, Smith J. Parent participation in the neonatal intensive care unit: Predictors and relationships to neurobehavior and developmental outcomes. Early Hum Dev. 2018 Feb; 117: 32-8.
10. Amaral CER. Lei nº 13.257/2016: políticas públicas para a primeira infância. Rev Jus Navigandi [
Internet]. 2016 Jul; 21 (4803). [access in 2021 Dez 21]. Available from:
https://jus.com.br/artigos/47246/lei-n-13-257-2016-politicas-publicas-para-a-primeira-infancia.
11. Fróes GF, Mendes EN, Pedroza GD, Cunha ML. Estresse experimentado por mães de recém-nascidos pré-termo em unidade de terapia intensiva neonatal. Rev Gaúcha Enferm. 2020; 41 (spe): e20190145.
12. Balbino FS, Balieiro MM, Mandetta MA. Measurement of Family-centered care perception and parental stress in a neonatal unit. Rev Latino-Am Enferm. 2016; 24: e2753.
13. Lessa ARD, Bitercourt VN, Crestani F, Andrade GRH, Costa CAD, Garcia PCR. Impact of the COVID-19 Pandemic on Patient- and Family-Centered Care and on the Mental Health of Health Care Workers, Patients, and Families. Front Pediatr. 2022 Jul; 10: 880686.
14. Souza SR, Dupas G, Balieiro MM. Adaptação cultural e validação para a língua portuguesa da Parental Stress Scale: Neonatal Intensive Care Unit (PSS:NICU). Acta Paul Enferm. 2012; 25 (2): 171-6.
15. Silva TO, Alves LB, Balieiro MM, Mandetta MA, Tanner A, Shields L. Adaptação transcultural de instrumentos de medida do cuidado centrado na família. Acta Paul Enferm. 2015 Abr; 28 (2): 107-12.
16. Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993; 42: 148-52.
17. Shields L, Mamun AA, Flood K, Combs S. Measuring family-centred care: working with children and their parents in two second level hospitals in Australia. Eur J Pers Cent Healthc. 2014; 2 (2): 206-11.
18. Petersen CB, Lima RAG, Balieiro MMFG, Mandetta MA. Parent and staff perceptions of patient and family‐centred care in a Brazilian paediatric's hospital: Quantitative study. J Eval Clin Pract. 2023; 29 (6): 765–73.
19. Kegler JJ, Neves ET, Silva AM, Jantsch LB, Bertoldo CD, Silva JH. Estresse em pais de recém-nascidos em uma Unidade de Terapia Intensiva Neonatal. Esc Anna Nery. 2019; 23 (1): e20180178.
20. Palma IE, Von Wussow KF, Morales BI, Cifuentes RJ, Ambiado TS. Estrés en padres de recién nacidos hospitalizados en una unidad de paciente crítico neonatal. Rev Chil Pediatr. 2017 Jun; 88 (3): 332-9.
21. Franck LS, Waddington C, O'Brien K. Family Integrated Care for Preterm Infants. Crit Care Nurs Clin North Am. 2020. Jun; 32 (2): 149-65.
22. Cassiano RG, Gaspardo CM, Linhares MB. Prematurity, neonatal health status, and later child behavioral/emotional problems: a systematic review. Infant J Ment Health. 2016 Abr; 37 (3): 274-88.
23. Gómez-Cantarino S, García-Valdivieso I, Moncunill-Martínez E, Yáñez-Araque B, Ugarte Gurrutxaga MI. Developing a Family-Centered Care Model in the Neonatal Intensive Care Unit (NICU): A New Vision to Manage Healthcare. Int J Environ Res Public Health. 2020 Out; 17 (19): 7197.
24. Mäkelä H, Axelin A, Feeley N, Niela-Vilén H. Clinging to closeness: The parental view on developing a close bond with their infants in a NICU. Midwifery. 2018 Jul; 62: 183-8.
25. Mandetta MA, Balieiro MM. A pandemia da COVID-19 e suas implicações para o cuidado centrado no paciente e família em unidade pediátrica hospitalar. Rev Soc Bras Enferm Ped. 2020; 20 (esp COVID-19): 77-84.
26. Institute for Patient and Family Centered Care. What is patient- and family-centered care?. Bethesda: Institute for Patient and Family Centered Care; 2020 [access in 2024 Mai 10]. Available from:
https://www.ipfcc.org/27. Shetty AP, Halemani K, Issac A, Thimmappa L, Dhiraaj S, Radha K, Mishra P,
et al. Prevalence of anxiety, depression, and stress among parents of neonates admitted to neonatal intensive care unit: a systematic review and meta-analysis. Clin Exp Pediatr. 2024 Feb; 67 (2): 104-15.
28. Bua J, Dalena P, Mariani I, Girardelli M, Ermacora M,
et al. Parental stress, depression, anxiety and participation in care in neonatal intensive care unit: a cross-sectional study in Italy comparing mothers versus fathers. BMJ Paediatr Open. 2024 Apr; 8 (Suppl. 2): e002429.
29. Sousa FP, Curado MAS. Parental stress in the neonatology unit - The influence of hospital stay length and neonatal unit differentiation. J Neonatal Nurs. 2023; 29 (3): 506-10.
30. Reem M, Sian H, Pilkington V, Opondo C, Gale C, Stein A,
et al. Factors associated with posttraumatic stress and anxiety among the parents of babies admitted to neonatal care: a systematic review. BMC Pregnancy Childbirth. 2024 May; 24 (1): 352.
Author's contributionBrondani AS, Jantsch LB e Jacobi LF: study design, data collection and analysis, interpretation of results, writing of the manuscript.
All the authors approve the final version of the article and declare no conflicts of interest.
Received on September 8, 2023
Final version presented on May 31, 2024
Approved on July 1, 2024
Associated Editor: Karla Bomfim
 ; Leonardo Bigolin Jantsch2
; Leonardo Bigolin Jantsch2 ; Luciane Flores Jacobi3
; Luciane Flores Jacobi3