ABSTRACT
OBJECTIVES: this study describes the occurrence of cesarean sections according to the Robson Classification in a public hospital in southern Brazil.
METHODS: a cross-sectional and retrospective study was conducted. Women who underwent vaginal delivery or cesarean section at the study location (gestational age >20 weeks and/or fetuses weighing > 500 g) were included. Stillbirths were excluded. Sociodemographic and obstetric data from July to November 2018 were retrospectively collected from medical records. Chi-square and linear trend tests were used for data analysis. The Robson Classification was analyzed according to World Health Organization recommendations, and the reasons for cesarean section were described.
RESULTS: the sample consisted of 1,531 women. The cesarean section rate was 39.1% (n=598). A greater incidence of cesarean sections was identified among women with no previous vaginal births, older women, those with higher educational levels, and those with more previous cesarean sections. Groups 1, 2 and 5 of the Robson Classification stood out for presenting cesarean section rates of 16%, 56.9% and 66.2%, respectively, and for totaling 60.3% of births by cesarean section in the studied institution.
CONCLUSIONS: the percentage of cesarean sections found was greater than that reported in studies conducted in other countries. Groups 1 to 5 of the Robson Classification presented rates lower than values found in national literature. Groups 1, 2 and 5 should be prioritized for management and care interventions aiming to reduce cesarean rates.
Keywords:
Cesarean section, Obstetrics, Parturition, Natural childbirth, Pregnancy
RESUMO
OBJETIVOS: descrever a ocorrência de cesáreas conforme a Classificação de Robson em hospital público no sul do Brasil.
MÉTODOS: estudo transversal retrospectivo. Foram incluídas mulheres com parto vaginal ou cesárea assistidos na instituição (idade gestacional >20 semanas e/ou fetos com peso >500g) e excluídos nascimentos de feto morto. Dados sociodemográficos e obstétricos de julho a novembro de 2018 foram coletados retrospectivamente dos prontuários. Para análise utilizou-se o teste qui-quadrado e teste de tendência linear. A Classificação de Robson foi analisada conforme recomendações da Organização Mundial da Saúde, e foram descritas as justificativas de cesárea.
RESULTADOS: amostra de 1.531 mulheres, com percentual de cesárea de 39,1% (n=598). Identificou-se maior ocorrência de cesarianas entre mulheres com maior faixa etária, nível de escolaridade e número de cesarianas prévias, e sem partos vaginais prévios. Os Grupos 1, 2 e 5 da Classificação de Robson destacaram-se por apresentar, respectivamente, os percentuais de cesárea de 16%, 56,9% e 66,2%, e por totalizar 60,3% dos nascimentos por via cirúrgica.
CONCLUSÕES: neste estudo, os percentuais de cesárea dos grupos da Classificação de Robson foram maiores quando comparados a estudos internacionais. Os Grupos 1 a 5 apresentaram valores menores em relação ao panorama nacional. Os Grupos 1, 2 e 5 destacaram-se como prioritários para intervenções assistenciais e de gestão.
Palavras-chave:
Cesárea, Obstetrícia, Parto, Parto normal, Gravidez
IntroductionOne of the Sustainable Development Goals is to reduce maternal and neonatal morbidity and mortality. Among the strategies to achieve this goal are the implementation of good practices in labor, childbirth and birth and the reduction of cesarean sections.
1According to the World Health Organization (WHO), a cesarean section rate greater than 15% does not help reduce morbidity or mortality.
2 The estimated occurrence of cesarean sections worldwide is 21.1%, 27.2% in high-income countries, 24.2% in middle-income countries and 8.2% in low-income countries. On the other hand, Latin America presents an estimate of 42.8%
3, and Brazil stands out in the world ranking of cesarean sections with a percentage of 57.0%
4-6, varying from 53.5 to 63.8% in the different Brazilian regions in 2021.
4 In Rio Grande do Sul, the percentage of cesarean sections was 64.2% in 2021.
4Cesarean sections are often inadequately justified and not based on current scientific evidence, in which case they become iatrogenic.
2,7 Possible indications include cephalopelvic disproportion, non-reassuring fetal status, previous cesarean section, unfavorable cervix for induction, pelvic or transverse fetus, genital herpes, placental problems, HIV (according to viral load), multiple pregnancies, cord prolapse and fetal macrosomia.
7,8 However, it should be noted that most of these indications should be individualized, considering that there are still differences between current recommendations.
To reduce the number of cesarean sections without clinical or obstetric indications, some measures are recommended. These include the integration of obstetric nurses in labor and childbirth care
9, the use of clinical guidelines and case discussions to indicate cesarean sections, the involvement of local specialists in continuing education for health professionals, and the monitoring and feedback of cesarean section practices to care teams.
10In 2015, the WHO recommended that all health institutions should implement the Robson Classification as a strategy for monitoring cesarean sections.
2 The Robson Classification is a tool that groups pregnant women into ten groups based on five criteria: parity, onset of labor, gestational age, fetal presentation and number of fetuses.
2,11-14 Its application considers epidemiological risk factors for surgical birth without considering clinical or obstetric indications, and it makes it possible to optimize cesarean sections through the following actions: identifying interventions in specific groups according to location; evaluating the effectiveness of strategies in reducing cesarean sections; evaluating the quality of care; and evaluating the outcomes by group.
2,11,12Regarding to the percentage of cesarean sections per group according to the Robson Classification, based on international studies,
13,15 the WHO has constructed the following parameters that can be used as guidelines when analyzing this indicator
12: Group 1) <10%; Group 2) 20% to 35%; Group 3) <3%; Group 4) <15%; Group 5) 50% to 60%; Group 8) 60%; Group 9) 100%; and Group 10) 30%. Although Groups 6 and 7 do not have standardized parameters established by WHO, their values are between 78.5% and 93.2% and between 73.8% and 85.0%, respectively.
13,15 In the national context, the percentages for eight of the ten groups are much greater than those reported internationally.
6This study is an initiative to monitor the occurrence of cesarean sections using the Robson Classification, which is encouraged by national public health policies and international guidelines. Therefore, this study aimed to describe the occurrence of cesarean sections according to the Robson Classification in a public hospital in southern Brazil.
MethodsThis was a cross-sectional study. Data from July 1, 2018 to November 21, 2018 were collected retrospectively between June 2019 and March 2020, at the Obstetric Center of a large federal public hospital located in Porto Alegre/RS, Brazil. This hospital provides 100% of its care through the
Sistema Único de Saúde (SUS) (Public Health System), attends an average of 300 births per month and is a regional reference for high-risk pregnancies. In addition, it seeks to follow current recommendations to apply good obstetric practices, including the implementation of the collaborative care model with the inclusion of obstetric nurses in labor and childbirth care.
The population consisted of women attended at the study scenario. All women who had a vaginal or cesarean delivery assisted at the institution with a gestational age greater than 20 weeks and with fetuses weighing 500 grams or more were included, and those with stillborn fetuses were excluded.
The sample size was calculated according to prevalence of cesarean sections studies. It took into consideration that 39% of births at the study location were by surgical means, according to data from the hospital Health Information System, with a 95% confidence level. The minimum number of births per Robson group was calculated according to the outcome studied (occurrence of cesarean sections) and to the characteristics of the study location, where it is estimated by local data that 24% of the women assisted are classified in the largest group (Group 3). Therefore, to ensure that the minimum composition of the group was present in the largest group, a minimum sample size of 1,525 births was stipulated. The sample selected was by convenience, considering the initial date of implementation of the Robson Classification at the institution and according to the period in months needed to reach the calculated sample size of births.
Data collection was carried out by the researchers themselves after training. Data were obtained from the sample's paper-based and electronic medical records using a standardized, pre-coded instrument developed by the researchers. The data were also collected from record books used by the hospital's obstetric team.
Regarding the variables, the following sociodemographic profile data were collected: age in complete years and categorized (<20/20-24/25-29/30-34/>35); race/color (white/black/mixed); schooling (elementary school/high school/higher education); and marital status (married/unmarried). Obstetric variables included: number of pregnancies (1/≥2); number of previous vaginal deliveries (0/1/≥2); number of previous cesarean sections (0 / 1 / ≥2); gestational age (in completed weeks); and “occurrence of cesarean section” (yes/no). The following information was considered as justification for the cesarean section, according to the terms registered in the medical records: anomalous fetal presentation (pelvic and transverse), multiple pregnancies, two or more previous cesarean sections, cephalopelvic disproportion, non-reassuring fetal status, failure to induce labor, no conditions for inducing labor, maternal conditions (HIV with viral load >1000 copies or unknown, eclampsia, placenta previa or occlusive placenta, placental abruption, active genital herpes, cord prolapse), fetal conditions (congenital malformations, macrosomia, intrauterine growth restriction) or maternal request.
At the study location, the Robson Classification is defined and registered by the care team in the women's medical records, using the criteria presented in Table 1. This study used the group designed in the medical records by the service team to analyze this variable.
The data were entered into an Excel
® spreadsheet. The data were then analyzed using SPSS
® version 22 statistical software. Categorical variables are presented as absolute and relative values, and the numerical variable “age” is also expressed as mean and standard deviation (SD). To compare the proportions of cesarean sections and vaginal deliveries, the women in the sample were grouped according to their sociodemographic and obstetric characteristics, and the chi-square test and linear trend test (for variables with a linear increase in the percentage value) were used for analysis; a significance value of 5% (α = 0.05) was considered. The analysis of the distribution of the sample in the Robson Classification groups was carried out in accordance with WHO recommendations.
12 The analysis of the distribution of cesarean section justifications by Robson Classification group is presented descriptively using percentages. The study was approved by the Ethics and Research Committee at the institution, according to document no. 3.252.730 on April 9, 2019 and CAAE no. 05684919.1.0000.5530.
ResultsA total of 1,550 births were selected for the sample, with 19 participants excluded according to the exclusion criteria; 1,531 medical records were analyzed in this study. The demographic and obstetric characteristics of the sample are described in Table 2. The average age was 28.4 (SD= 6.6) years. The women were predominantly white (68.0%), unmarried (88.0%), and had completed elementary school (50.4%). Regarding obstetric characteristics, 66.2% of the sample had two pregnancies or more, 56.4% had no previous vaginal births and 75.6% had no previous cesarean section. In the sample, 60.7% were not nulliparous: 71.7% of these women had one or more previous vaginal births, and 40.2% had one or more previous cesarean sections.
The occurrence of cesarean sections was 39.1% (n=598) in the sample. Of the women with a previous cesarean section, 54.0% underwent a new cesarean section. The greater the age group (
p<0.001) and schooling level (
p<0.001) were, the greater the frequency of cesarean section. A greater occurrence of cesarean section was observed among women with a greater number of previous cesarean sections (
p<0.001), while a lower percentage of cesarean sections was identified among those with a greater number of previous vaginal deliveries (
p<0.001).
Table 3 shows the distribution of the sample according to the Robson Classification, as well as the percentage of cesarean sections in each group and the absolute and relative contribution of each group to the total proportion of cesarean sections in the sample. The group with the highest representation in the sample was Group 3 (22.1%), and the groups with the highest relative contribution to the cesarean rate at the institution were Group 5 (32.4%) and Group 2 (20.7%).
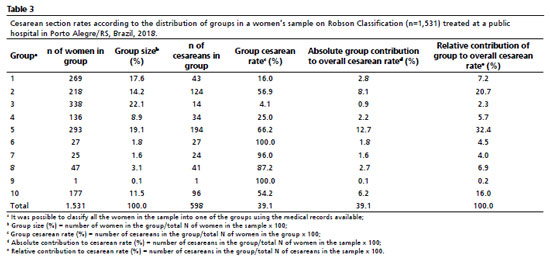
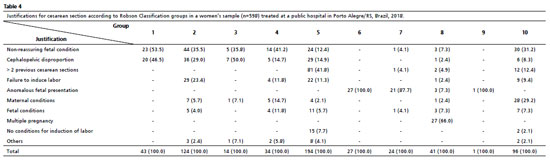
In a complementary examination, the justification registered by the team for performing the cesarean sections was analyzed. It was found that in the sample the most frequent were non-reassuring fetal status (24.1%), cephalopelvic disproportion (17.6%) and two or more previous cesarean sections (16.1%). When the justifications were analyzed within the Robson Classification groups, it was found that Groups 1, 2 and 3 had greater percentages of cephalopelvic disproportion than did the other groups (Table 4) in the sample. Failure to induce labor emerged as a justification for performing a cesarean section in 10.9% of the sample, with a greater percentage in Group 2 than in the other groups (Table 4). Other justifications given in the sample were: anomalous fetal presentation (8.5%), maternal condition (7.7%), fetal condition (5.2%), multiple gestation (4.5%) and no conditions for inducing labor (2.8%). Groups 6, 7 and 9 of the Robson Classification were justified by anomalous fetal presentation.
In the sample studied, there was a greater occurrence of cesarean sections among women without previous vaginal births, those in a higher age group, those with a higher level of schooling and those with a greater number of previous cesarean sections. In addition, Groups 1, 2 and 5 of the Robson Classification stood out for representing the majority of the surgical births in the sample.
In this study, the greater the maternal age was, the greater the occurrence of cesarean section. This finding is in line with other studies
11,16 and may be related to the fact that older women are more susceptible to developing complications during pregnancy which can influence the number of cesarean sections performed.
17The percentage of cesarean sections was also greater among women with a higher level of schooling. However, a more robust analysis would be necessary to assess whether this effect would be maintained in association with other socioeconomic variables, since the literature shows divergences on the impact of these factors on this indicator.
5,18 A Brazilian study carried out in public and private hospitals revealed no difference between schooling and the proportion of cesarean sections. However, it was found that other socioeconomic factors were associated with a greater probability of cesarean section compared to the rest of the sample.
5 On the other hand, a study of women treated only in public hospitals with established obstetric protocols concluded that socioeconomic indicators had no influence on cesarean section rates, which were probably only determined by clinical and obstetric indications.
19The higher proportion of cesarean sections among women with no previous vaginal delivery and among women with previous cesarean sections reinforces the importance of measures to avoid the first cesarean section
6 and the use of tools such as the Robson Classification to analyze the occurrence of births by surgery in health services.
The overall percentage of cesarean sections in this sample was greater than that in developed countries.
20,21 However, the rates are lower than the national average and those found in different Brazilian regions
4. The occurrence of cesarean sections in the Robson Classification groups was also higher than that reported in international studies.
13,15 However, the percentages for Groups 1, 2, 3, 4 and 5 are lower than those found at the national and regional levels.
6 An example of this is the data on surgical births according to the Robson Classification groups in the southern region of Brazil in 2021
4: Group 1, 46.2%; Group 2, 74.4%; Group 3, 16.9%; Group 4, 49.5%; and Group 5, 86.5%. This scenario illustrates the current cesarean epidemic in the country.
Considering the occurrence of cesarean sections within each group, a percentage of more than 50% was observed in Groups 2, 5 and 10. Groups 6, 7, 8 and 9 represent situations that usually make it difficult or prevent vaginal delivery.
22 The discussion about the high percentage of cesarean sections in Group 10 must include the fact that the service studied is a reference for high-risk pregnancies, which can result in a greater number of premature births by surgery.
22The sum of the percentages of Groups 1, 2 and 5 represents 60.3% of cesarean sections performed at the institution (relative contribution); these data are similar to those described by an international multicenter study
15. The findings suggest that these are the priority groups for interventions to reduce cesarean section risk, and actions should be based in reviewing the obstetric practices of healthcare teams.
6,12,17,22 Thus, national studies propose the implementation of health policies to prevent unnecessary cesarean sections, especially elective ones performed in women of Groups 1 and 2 – when these women undergo cesarean sections, they become part of Group 5.
23,24 Likewise, public policies are also aimed at encouraging vaginal delivery after cesarean section to prevent repeated cesarean sections,
24 since this population is at greater risk of obstetric complications that increase maternal and neonatal morbidity and mortality compared to women who have vaginal deliveries.
7To change this scenario, the WHO
1 encourages the inclusion of obstetric nurses in labor and childbirth care since women who are assisted by teams with obstetric nurses receive fewer interventions and have a greater chance for spontaneous vaginal delivery.
9,25 The adoption of this care model by the studied institution may have contributed to a lower occurrence of cesarean sections in the sample and a lower relative contribution of cesarean sections in groups 1 to 4 compared to national and regional data.
6,23In this study, there was a high contribution (relative and absolute) of cesarean sections in Group 2, in line with the literature that characterizes this group as having the highest proportion of cesarean sections among nulliparous women, with a percentage ranging from 24.0 to 69.0%.
6,15,17,23,26 When analyzing the heterogeneous composition of Group 2, its stratification is suggested
12 into women who underwent labor induction and those who had a cesarean section before labor began, since the occurrence of cesarean sections in each of these subgroups requires different interventions such as reviewing the induction protocol used and reducing elective cesarean sections.
In this study, Group 5 had the highest relative contribution to the total number of cesarean sections in the sample, which is in line with the findings in the literature,
15,17,26 especially in southern Brazil.
6 Group 5 can be divided into women with one previous cesarean section and those with two or more to identify strategies to reduce cesarean sections for each subgroup.
12In the sample studied, the main justification used by the team for performing cesarean sections was non-reassuring fetal status, a finding that differs from that observed in international studies.
27,28 This finding points to the need to deepen the analysis, identify factors associated with the occurrence of non-reassuring fetal status during labor at the study location and train the team to improve obstetric care. The second most frequent justification for cesarean section in the sample was cephalopelvic disproportion, highlighting the need for strategies to improve the assessment of the progress of labor and this diagnosis, such as the proper use of the partograph.
29The occurrence of cesarean sections justified by previous cesarean sections in the sample was lower than that reported by other studies (35.0 to 42.0%),
27,28 which may be related to the fact that a single previous cesarean section is not an indication for surgical birth at the study location. However, changes in obstetric practices are still needed, as the literature shows that vaginal delivery in women with two previous uterine scars does not increase unfavorable maternal or neonatal outcomes.
30Regarding the possible limitations of this study, it should be noted that the data used for analysis came from the medical records (including the Robson Classification), which may have errors in completion and restrictions in the format of data presentation. In addition, it is believed that a multivariate analysis could help to better understand the findings. For positive aspects, we highlight the impact of local research on the discussion and evaluation of institutional practice, especially in a public service context, and its potential to generate changes in the current obstetric scenario. The analysis of clinical and obstetric indications for cesarean section in each group of the Robson Classification is also a distinguishing feature of this study.
In conclusion, this study described the occurrence of cesarean sections according to the Robson Classification in a public hospital in southern Brazil. Although the figures are still above those recommended by WHO, the percentage of cesarean sections found was lower than the national average, which may reflect the interdisciplinary obstetric care model adopted at the institution. The results of this study suggest that Groups 1, 2 and 5 are priority groups for care and management interventions. Actions aimed at preventing cesarean sections in nulliparous women could lead to a reduction in Group 5.
References1. World Health Organization (WHO). WHO recommendations: intrapartum care for a positive childbirth experience [
Internet]. Geneva: WHO; 2018. [access in 2022 Dec 3]. Available from:
http://apps.who.int/iris/bitstream/10665/260178/1/9789241550215-eng.pdf2. Organização Mundial da Saúde (OMS). Declaração da OMS sobre Taxas de Cesáreas [
Internet]. Geneva: WHO; 2015. [access in 2023 Out 10]. Available from:
http://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_por.pdf3. Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021; 6: e005671.
4. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde. Nascidos Vivos no Brasil [
Internet]. Brasília (DF); 2021. [access in 2023 Out 10]. Available from:
http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvuf.def5. Kluthcovsky ACGC, Amari VCS, Esperidião CR, Ciriaco EM, Freitas NB, Vernizi BT. Trends and factors associated with cesarean sections in Brazil and its States between 2001 and 2015. Mundo Saúde. 2019; 43 (4): 1044-63.
6. Knobel R, Lopes TJP, Menezes MDO, Andreucci CB, Gieburowski JT, Takemoto MLS. Cesarean-section Rates in Brazil from 2014 to 2016: cross-sectional analysis using the Robson Classification. Rev Bras Ginecol Obstet. 2020; 42 (9): 522-8.
7. American College of Obstetricians and Gynecologists (ACOG). Obstetric Care Consensus Nº 1: Safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014 Mar; 123 (3): 693-711.
8. National Institute for Health and Care Excellence (NICE). Caesarean birth: NICE guideline. [
Internet]. London: NICE; 2021 [access in 2023 Out 10]. 45p. Available from:
https://www.nice.org.uk/guidance/ng192/9. Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2016 Apr; 4 (4): CD004667.
10. Chen I, Opiyo N, Tavender E, Mortazhejri S, Rader T, Petkovic J,
et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2018; 9 (9): CD005528.
11. Alcantara LLM, Almeida NKO, Almeida RMVR. Pattern of Live Births in Rio de Janeiro State, Brazil, According to Robson Groups and the Kotelchuck Index Classification - 2015/2016. Rev Bras Ginecol Obstet. 2020; 42 (7): 373-9.
12. World Health Organization (WHO). Robson Classification: Implementation manual [
Internet]. Geneva: WHO; 2017 [access in 2023 Out 10]. Available from:
http://apps.who.int/iris/bitstream/handle/10665/259512/9789241513197-eng.pdf13. Robson M, Hartigan L, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Pract Res Clin Obstet Gynaecol. 2013; 27 (2): 297-308.
14. Robson M. Classification of caesarean sections. Fetal Matern Med Rev. 2001; 12 (1): 23-39.
15. Souza JP, Betran AP, Dumont A, Mucio B, Pickens CMG, Deneux-Tharaux C,
et al. A global reference for caesarean section rates (C-Model): A multicountry cross-sectional study. BJOG. 2016; 123: 427-36.
16. Bergholt T, Skjeldestad FE, Pyykönen A, Rasmussen SC, Tapper AM, Bjarnadóttir RI,
et al. Maternal age and risk of cesarean section in women with induced labor at term: a Nordic register-based study. Acta Obstet Gynecol Scand. 2020; 99: 283-9.
17. Abreu LP, Lira Filho R, Santana RL. Obstetric characteristics of pregnant women undergoing cesarean section, by the Robson Classification. Rev Enferm UERJ. 2019; 27: e37858.
18. Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L,
et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018; 392 (10155): 1341-8.
19. Faisal-Cury A, Menezes PR, Quayle J, Santiago K, Matijasevich A. The relationship between indicators of socioeconomic status and cesarean section in public hospitals. Rev Saúde Pública. 2017; 51 (14): 1-11.
20. Einarsdóttir K, Sigurðardóttir H, Bjarnadóttir RI, Steingrímsdóttir Þ, Smárason AK. The Robson 10-group classification in Iceland: Obstetric interventions and outcomes. Birth. 2019; 46 (2): 270-8.
21. Vargas S, Rego S, Clode N. Robson Classification System Applied to Induction of Labor. Rev Bras Ginecol Obstet. 2018; 40 (9): 513-7.
22. Soares KB, Klein VCG, Lima JARF, Gadenz L, Paulo LE, Konopka CK. Gestational Risk as a Determining Factor for Cesarean Section according to the Robson Classification Groups. Rev Bras Ginecol Obstet. 2021; 43 (2): 84-90.
23. Rudey EL, Leal MC, Rego G. Cesarean section rates in Brazil: Trend analysis using the Robson classification system. Medicine (Baltimore). 2020; 99 (17): e19880.
24. Paz LDC, Banegas RC, Luz AG, Costa ML. Robson's Ten Group Classification System to Evaluate Cesarean Section Rates in Honduras: the relevance of labor induction. Rev Bras Ginecol Obstet. 2022; 44 (9): 830-7.
25. Gama SGN, Viellas EF, Medina ET, Tuesta AA, Silva CKRT, Silva SD,
et al. Atenção ao parto por enfermeira obstétrica em maternidades vinculadas à Rede Cegonha, Brasil – 2017. Ciênc Saúde Colet. 2021; 26 (3): 919-29.
26. Vargas S, Rego S, Clode N. Cesarean Section Rate Analysis in a Tertiary Hospital in Portugal According to Robson Ten Group Classification System. Rev Bras Ginecol Obstet. 2020; 42 (6): 310-5.
27. Begum T, Nababan H, Rahman A, Islam MR, Adams A, Anwar I. Monitoring caesarean births using the Robson ten group classification system: a cross-sectional survey of private for-profit facilities in urban Bangladesh. PLoS One. 2019; 14 (8): e0220693.
28. Manny-Zitle AI, Tovar-Rodríguez JM. Incidence of cesarean section according to Robson's classification in the Department of Gynecology and Obstetrics of the General Hospital Dr. Fernando Quiroz Gutiérrez, ISSSTE. Cir Cir. 2018; 86: 232-9.
29. Lavender T, Cuthbert A, Smyth RMD. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev. 2018; 2018 (8): CD0054.
30. De Leo R, La Gamba DA, Manzoni P, De Lorenzi R, Torresan S, Franchi M,
et al. Vaginal Birth after Two Previous Cesarean Sections versus Elective Repeated Cesarean: a Retrospective Study. Am J Perinatol. 2020; 37: 84-8.
Authors' contribution: Patuzzi GC, Schuster RV, Dornfeld D, Luz CB, Canassa CCT, Neutzling AL: conception, structuring, data analysis and interpretation, writing and critical revision of the manuscript.
All the authors have approved the final version of the article and declare no conflicts of interest.
Received on June 29, 2023
Final version presented on April 26, 2024
Approved on May 29, 2024
Associated Editor: Melânia Amorim
Approved in September 30, 2025
Erratum
In “Robson classification to evaluate cesarean section rates in a public hospital: a cross-sectional study”. Rev Bras Saúde Matern Infantil. 2024; 24: e20230027, RBSMI corrects the DOI.
In Page 1, Where it reads:
http://dx.doi.org/10.1590/1806-9304202400000027-en
Reading:
http://dx.doi.org/10.1590/1806-9304202420230027-en |
 ; Raquel Vieira Schuster2
; Raquel Vieira Schuster2 ; Dinara Dornfeld3
; Dinara Dornfeld3 ; Camila Borba da Luz4
; Camila Borba da Luz4 ; Carolina de Castilhos Teixeira Canassa5
; Carolina de Castilhos Teixeira Canassa5 ; Agnes Ludwig Neutzling6
; Agnes Ludwig Neutzling6