ABSTRACT
OBJECTIVES: to estimate the role of maternal overweight and obesity before pregnancy as predictors of childhood asthma in a population of Peruvian children under five years.
METHODS: we carried out a retrospective cohort study of children aged five years or less and their mothers from the Regional Hospital of Ayacucho and the María Auxiliadora Hospital in Lima, Peru. We included children who were born between 2013 and 2014 and follow them up until 2018 and 2019, respectively. The diagnosis of overweight and obesity of the mother before pregnancy and asthma in the child were registered in their clinical histories. Crude (cRR) and adjusted relative risks (aRR) and 95% confidence intervals (CI95%) were obtained using a generalized lineal model of the Poisson family with link log and robust variances.
RESULTS: we evaluated 431 medical records and found that 20.9% of the children had asthma, 26.7% of the mothers were overweight, and 20.2% were obese before pregnancy. In the adjusted regression model, overweight (aRR=2.94; CI95%= 1.54-5.60) and maternal obesity (aRR=5.10; CI95%= 2.73-9.51) were predictors of an increased risk of childhood asthma.
CONCLUSIONS: maternal overweight and maternal obesity increased the risk of her children developing asthma three- and five-fold, respectively.
Keywords:
Asthma, Overweight, Obesity, Child, Pregnancy
RESUMO
OBJETIVOS: estimar el papel del sobrepeso y la obesidad materna antes del embarazo como predictores de asma infantil en una población de niños peruanos menores de cinco años.
MÉTODOS: realizamos un estudio de cohorte retrospectivo de niños de cinco años o menos y sus madres del Hospital Regional de Ayacucho y del Hospital María Auxiliadora de Lima, Perú. Se incluyeron niños nacidos entre 2013 y 2014 y se les dio seguimiento hasta 2018 y 2019, respectivamente. El diagnóstico de sobrepeso y obesidad de la madre antes del embarazo y asma en el niño fueron registrados en sus historias clínicas. Los riesgos relativos crudos (cRR) y ajustados (RRa) y los intervalos de confianza del 95% (IC95%) se obtuvieron mediante un modelo lineal generalizado de la familia de Poisson con log de enlace y varianzas robustas.
RESULTADOS: se evaluaron 431 historias clínicas y se encontró que el 20,9% de los niños tenían asma, el 26,7% de las madres tenían sobrepeso y el 20,2% eran obesas antes del embarazo. En el modelo de regresión ajustada, el sobrepeso (aRR=2,94; IC95%= 1,54-5,60) y obesidad materna (RRa=5,10; IC95%= 2,73-9,51) fueron predictores de un mayor riesgo de asma infantil.
CONCLUSIONES: el sobrepeso materno y la obesidad materna aumentaron tres y cinco veces el riesgo de que sus hijos desarrollaran asma, respectivamente.
Palavras-chave:
Asma, Sobrepeso, Obesidad, Niño, Embarazo
IntroductionOverweight and obesity are multifactorial chronic conditions due to changes in lifestyle.
1 Both conditions are considered a public health problem and in the case of obesity, the prevalence tripled between 1975 and 2016, affecting more than 650 million adults worldwide in 2016.
2 According to a study carried out in 2019, in Peru, 20.6% of the female population over the age of 18 was obese.
3 Overweight and obesity are a health problem in women of reproductive age and even affect pregnant women.
4 In our country, a study carried out by the National Center for Food and Nutrition showed that more than half of the Peruvian women evaluated during the years 2009 and 2010 were overweight or obese at the beginning of their pregnancy.
5In pregnant women, overweight and obesity are related to arterial hypertension, gestational diabetes, miscarriage, intrauterine fetal death, fetal macrosomia, and increased maternal and fetal mortality.
6 In addition, they are related to an increase in inflammatory markers such as cytokines and adipokines which, in the long term, cause physiological modifications leading to alterations in respiratory function due to the proinflammatory state and can condition the appearance of respiratory diseases in their children.
7-9Respiratory diseases are common in pediatrics, with asthma being the most common chronic disease in childhood.
10-11 Childhood asthma is a chronic inflammatory disease of the airways that produces recurrent episodes of wheezing, dyspnea, and dry cough.
9 In the United States, asthma affects approximately 6.8 million children, which causes a considerable burden of hospitalizations and an estimated loss of 13.8 million days annually due to the management of patients who suffer from it.
12-13 Other data show the overall highest prevalence in the Puerto Rican population (17.0%) and the lowest prevalence in the Mexican American population (3.9%).
13 In Peru, it is estimated that 20% of the child population has this disease, which makes Peru the country with the highest prevalence of childhood asthma in Latin America.
14 The main risk factors associated with childhood asthma are male gender, family history, and allergies.
15 Additionally, it is suggested that maternal overweight and obesity could also be risk factors for this disease.
16 Obesity is associated with increased respiratory effort and impaired functional lung capacity, as well as a systemic proinflammatory state with increased cytokines and chemokines, being especially of note in women due to the bronchoconstrictive action of the aromatase enzyme.
16-19 In this sense, a systematic review of 145,574 mother-child pairs suggested that both maternal overweight and obesity before pregnancy increase the risk of children presenting childhood asthma and wheezing. However, no study has included Hispanic mothers and children as a sample.
20 Taking into account that according to the World Health Organization (WHO) the Hispanic ethnic group has a higher prevalence of obesity and childhood asthma, we considered it necessary to evaluate this possible association in our population in order to identify possible potentially preventable risk factors against the development of childhood asthma.
21 Therefore, the objective of this research was to estimate the role of maternal overweight and obesity before pregnancy as predictors of childhood asthma in a population of Peruvian children under five years.
MethodsWe developed a retrospective cohort study. The population was children under five years of age and their mothers from the María Auxiliadora Hospital in Lima and the Ayacucho Regional Hospital. We included children who were born between 2013 and 2014 and follow them up until 2018 and 2019, respectively. We excluded children and the mothers with incomplete medical records or those that did not have the variables of interest, as well as children with medical histories of lung disease, cancer, human immunodeficiency virus infection, or congenital and genetic diseases.
We estimated the sample size considering the incidence of asthma in children of mothers who were not overweight before pregnancy and of mothers who were overweight before pregnancy (49.8% and 26.4% respectively).
20 A power of 80% and a confidence level of 95% were considered. The final calculated sample size was 143 mother-child pairs. A percentage of data loss from medical records of 30% was considered, for which the final sample size was 204.
The outcome variable was the diagnosis of childhood asthma made by a pediatrician and recorded in the medical record using the ICD-10 code J45. In these hospitals, diagnosis is based on a parental history of atopic disease (asthma or atopic dermatitis), a history of atopic disease (recurrent episodes of wheezing, coughing, shortness of breath, and chest tightness), a physical examination confirming obstruction of the respiratory tract and the absence of an alternative explanation.
22,23.The exposure variable was maternal body mass index (BMI) prior to pregnancy recorded in medical records. Overweight and obesity were defined if the mother had a BMI between 25 and 30 kg/m
2 and greater than 30 kg/m
2, respectively.
In addition, the following variables were collected: age and sex of the child, age of the mother, area of residence (coast, mountains, jungle) and educational level of the mother (primary, secondary, and higher). Likewise, gestational age was considered (premature with less than 37 weeks, at term between 37 to 41 weeks and post term with more than 41 weeks) and birth weight (extremely low weight with less than 1000 g, very low weight with less than 1500 g, low weight with less than 2500 g, insufficient birth weight between 2500 and 2999 g, normal weight between 3000 and 4000 g and macrosomia with more than 4000 g). Prematurity was also included if the child was born before 37 weeks, as well as the type of delivery (natural or cesarean section) and the APGAR score at 5 minutes after birth (severe depression from 0-3, moderate depression from 4-6 and normal if was from 7-10). Additionally, the Silverman and Anderson Test was evaluated at birth (without respiratory distress if the score was 0, mild respiratory distress from 1-3, moderate respiratory distress from 4-6 and severe respiratory distress from 7-10); the family history of atopy in the child and the time of diagnosis of childhood asthma (0-12 months, 1-2 years, and 2-5 years). The age of the first childhood asthma attack (0-12 months, 1-2 years, and 2-5 years) and the number of childhood asthma attacks in the last year (0-5 attacks, 5-10 attacks and 10 or more attacks) were also evaluated.
Other variables were a maternal family history of diabetes, arterial hypertension, and cardiovascular disease; if the pregnant woman presented any respiratory disease during pregnancy and the consumption of harmful substances (tobacco, alcohol, drugs, or none) recorded in her medical history.
Data in the Excel program was exported to STATA v17.0 software (College Station Stata Corp). For the description of numerical variables, we presented means and standard deviation or medians and interquartile ranges, as appropriate. For the categorical variables, we calculated frequencies and percentages.
We used Chi-square and Fisher exact tests for the bivariable analysis comparing categorical variables. For the comparison of mean/medians between two groups, we used the Student's-t and Mann Whitney U tests, as appropriate.
For the multivariable analysis, we used a generalized linear model of the Poisson family with logarithmic link function and robust variances to estimate the relative risk (RR) with their respective 95% confidence intervals (CI95%) of the association of interest. We performed two models, one crude and the other adjusted for potential confounders. Likewise, we evaluated the assumptions of the chosen regression model, as well as collinearity problems. Values of
p less than 0.05 were considered significant.
This study was approved by the Ethics Committee of the Peruvian University of Applied Sciences with approval number FCS-CEI 572-07-2 and permission to access information from the Maria Auxiliadora Hospital and the Regional Hospital of Ayacucho.
ResultsWe evaluated 431 clinical histories of children: 66.8% being boys. The histories of the children showed that 10.4% were premature and 18.6% had a family history of atopy. Among the mothers, 26.7% were overweight and 20.2% were obese. The rest of the characteristics are shown in Table 1.
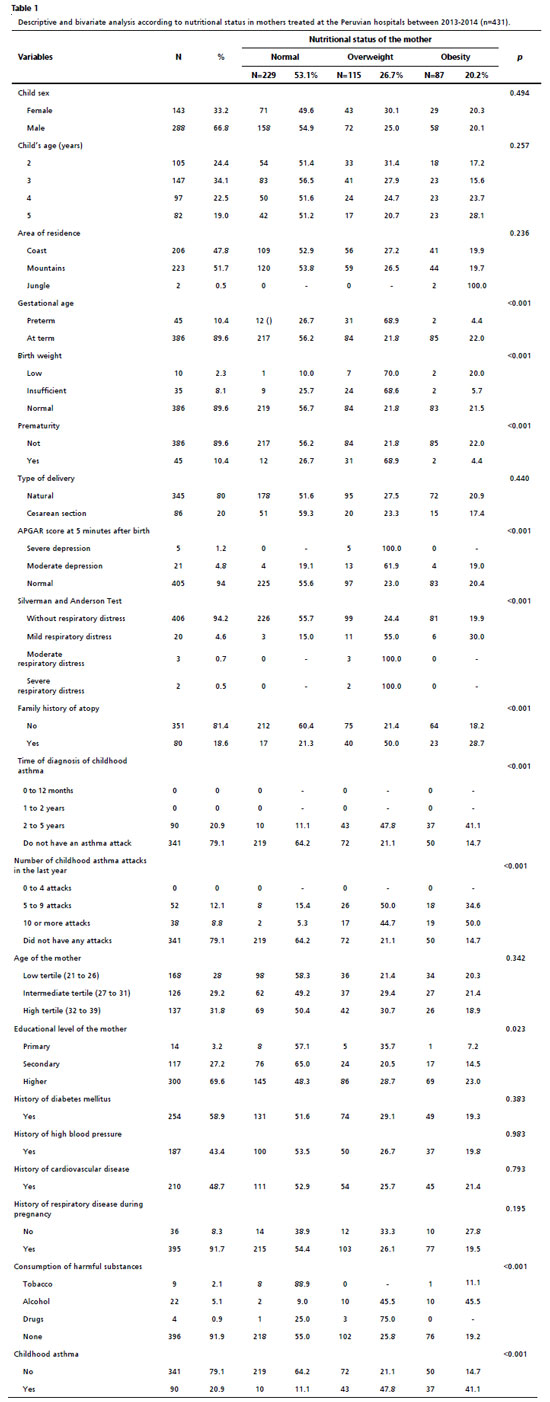
In the bivariable analysis of the characteristics of the children and the BMI categories of the mothers, we found a significant association with gestational age, birth weight, prematurity, the APGAR score at 5 minutes, the Silverman Anderson score, the family history of atopy, age at first asthma attack, and number of attacks in the last year (Table 1). Similarly, in the bivariable analysis of the general characteristics of the children according to the incidence of childhood asthma, there was a significant association with gestational age, birth weight, prematurity, the APGAR at 5 minutes, the Silverman Anderson score, the family history of atopy, the age of the first asthmatic attack and the number of attacks in the last year (Table 2).
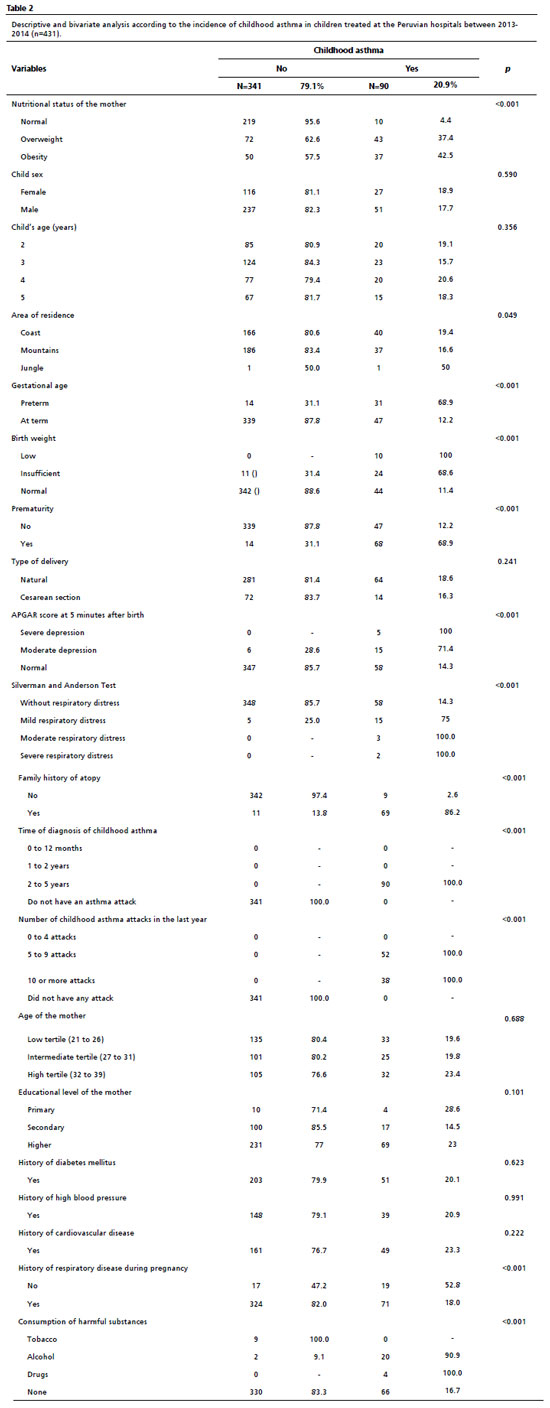
In the crude multivariable analysis, we found that overweight (cRR=8.56; CI95%= 4.46-16.42) and maternal obesity (cRR=9.74; CI95%= 5.06 -18.73) were predictors of an increased risk of childhood asthma incidence (Table 3). This association was maintained in the adjusted analysis after including confounding variables such as child sex, age, prematurity, type of delivery, family history of atopy, and mother age tertiles, both in the case of overweight (aRR=2.94; CI95%= 1.54-5.60) and maternal obesity (aRR=5.10; CI95%= 2.73-9.51) (Table 3).
DiscussionThe main finding of our study was that maternal overweight and obesity before pregnancy increased the risk of the children developing asthma by almost three- and five-fold, respectively. Although with some methodological and sociodemographic differences, other studies have described similar results. Research in Danish children found that maternal obesity during pregnancy was associated with an increased risk of asthma and wheezing in children.
24 Similarly, in the Netherlands, another study found that children with a predisposition to asthma may have an increased risk of developing the disease during childhood if their mothers were overweight before pregnancy.
25 Another study also conducted in Dutch children concluded that maternal obesity before pregnancy was associated with increased risks of asthma in their offspring.
26 Finally, in the United States, it was found that extremely low or extremely high gestational weight gain in the mother were risk factors for the development of asthma in early childhood due to the long-term impact of intrauterine exposure in children.
20The reasons why overweight and obesity are related to the development of childhood asthma are not fully understood; however, they are believed to be multifactorial and include the relationship between these diseases and respiratory symptoms. In this sense, they are associated with an alteration of lung functional capacity and with the development of respiratory symptoms, which appear because of a hardening of the airways, a reduction in lung compliance and an increase in alveolar surface tension in the lungs in patients with overweight and especially in those with obesity.
16 The increase in adiposity around the rib cage and abdomen produces an increase in intra-abdominal pressure, which compresses the diaphragm, being considered the equivalent of a chronic abdominal compartment syndrome that gives rise to a decrease in lung volume.
18 Although our study was not designed to assess differences by sex, it has been reported that the association between obesity and the development of asthma is greater in women than in men.
17 This is due to the role of estrogens, since by increasing the percentage of body fat, the aromatase enzyme present in adipose tissue also increases and is responsible for transforming androgens into estrogens.
19 These hormones have bronchoconstriction action, which worsens the respiratory condition.
27Additionally, increased fatty tissue in people with obesity results in a systemic pro-inflammatory state in which cytokine and chemokine aggregation is increased.
28 These inflammatory intermediaries are created and secreted by fat cells and include interleukin IL-6, IL-10, tumor necrosis factor (TNF), C-reactive protein, leptin, and adiponectin.
28 TNF is in the cells of fatty tissue and is directly related to the increase of fat in the body, and its concentrations increase in asthmatic pathology and are closely connected with the production of TH2 cytokines (IL-4, IL-6) in the bronchi tissue. Likewise, elevated IL-6 levels in the bloodstream are present in subjects with obesity and are associated with the severity of asthma.
28 On the other hand, obese women are more likely to have low levels of vitamin D, which have been associated with an elevated risk of childhood infections and wheezing.
29 Likewise, obesity is related to altered microbial colonization, which during pregnancy alters infant intestinal colonization, increasing the later risk of asthma.
29Our results suggest an association that raises the need to prevent overweight and obesity in pregnant women to not only reduce the probability of developing asthma in their children but also prevent other complications associated with these diseases. Overweight or obese mothers are more likely to require an emergency cesarean delivery, develop gestational diabetes, postpartum hemorrhage, preeclampsia, premature rupture of membranes, as well as have a predisposition to surgical site infection.
30 On the other hand, newborns born to overweight or obese mothers are at increased risk of neonatal intensive care unit admission, 5-minute APGAR scores less than 7, macrosomia, extreme preterm delivery, fetal congenital anomalies, and perinatal death.
30Our study has some limitations. First, there is a selection bias of the population since we only considered patients of 5 years of age attended in the previously mentioned hospitals. Second, information recorded in medical records was collected, and its quality could not be verified. Third, the diagnosis of childhood asthma is a limitation, since no pulmonary function test such as spirometry was used and the diagnosis was made by the child's clinic, which may have a margin of error. Fourth, we only had permission to access the information of the patients who were treated in hospitals on the coast and in the mountains, and the jungle would have been a variable of interest to observe the development of the study in the Peruvian state. Lastly, some confounding variables could not be measured due to lack of data, such as prenatal care, medical history of the child, exposure to cigarette smoke or allergens at home, and laboratory tests such as the maternal lipid profile.
In conclusion, being overweight tripled and maternal obesity quintupled the risk of developing asthma in a population of Peruvian children under five years. Weight control measures should be established in pregnant women to prevent the development of asthma and other complications.
Our results reinforce the need to measures to prevent obesity. In this sense, there are recommendations for preconception care of pregnant women with obesity that include receiving information about the risks of weight gain, as well as the benefits of losing weight prior to pregnancy, diet advice and exercises. In, childhood obesity, successful strategies included both parental and family-based interventions in conjunction with modifying the child's diet and physical activity behaviors.
References1. Rodrigo-Cano S, Soriano del Castilho JM, Merino-Torres JF. Obesity's causes and treatment. Nutr Clin Diet Hosp. 2017; 37 (4): 87-92.
2. Pérez MA, Blasco EF. Los costes económicos de la obesidad y el sobrepeso. [
Internet]. França: Université de Lyon; 2018. [access in 2021 Jun 5]. Available from:
https://halshs.archives-ouvertes.fr/halshs-01764899/document3. Paz-Krumdiek M, Rodriguez-Vélez SG, Mayta-Tristán P, Bernabe-Ortiz A. Association between sitting time and obesity: A population-based study in Peru. Nutr Diet. 2020 Apr; 77 (2): 189-95.
4. Pacheco-Romero J. Gestación en la mujer obesa: consideraciones especiales. An Fac Med. 2017; 78 (2): 207-14.
5. Pacheco-Romero J. From the Editor on Obesity in Pregnancy. Rev Peru Ginecol Obstet. 2016; 62 (4): 347-53.
6. Bustillo AL, Melendez WRB, Urbina LJT, Nuñez JEC, Eguigurems DMO, Pineda CVP,
et al. Sobrepeso y obesidad en el embarazo: complicaciones y manejo. Arch Med. 2016; 12 (3): 11.
7. Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev. 2015; 16 (8): 621-38.
8. Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L. The association between maternal body mass index and child obesity: A systematic review and meta-analysis. PLoS Med. 2019 Jun; 16 (6): e1002817.
9. Kliegman RM, Stanton B, St Geme JW, Schor NF, Behrman RE, Nelson WE. Nelson Textbook Pediatrics. 21
st ed. In: Pediatric Asthma. 2020; 5 (3): 1146–67. [
Internet]. Philadelphia: Elsevier; 2020. [access in 2023 Nov 30]. Available from:
https://www.clinicalkey.com/#!/browse/book/3-s2.0-C2016101712110. Martínez-Montilla JM, Amador-Marín B, Guerra-Martín MD. Family coping strategies and impacts on family health: a literature review. Enferm Glob. 2017; 16 (47): 592-604.
11. Organización Mundial de la Salud (OMS). 10 datos sobre el asma. [
Internet]. Geneva: OMS; 2017. [access in 2021 Apr 17]. Available from:
https://www.who.int/es/news-room/facts-in-pictures/detail/asthma12. Booster GD, Oland AA, Bender BG. Psychosocial factors in severe pediatric asthma. Immunol Allergy Clin North Am. 2016 Aug; 36 (3): 449–60.
13. Loftus PA, Wise SK. Epidemiology and economic burden of asthma. Int Forum Allergy Rhinol. 2015 Sep; 5 (Suppl. 1): S7-10.
14. Seguro Social de Salud (EsSalud). EsSalud: Uno de cada cinco niños sufre de asma en el Perú. [
Internet]. Lima: EsSalud; 2017. [access in 2021 Apr 17]. Available from:
http://www.essalud.gob.pe/essalud-uno-de-cada-cinco-ninos-sufre-de-asma-en-el-peru/15. Nicholson A, Pollard SL, Lima JJ, Romero KM, Tarazona-Meza C, Malpartida-Guzmán G. Serum folate concentrations, asthma, atopy, and asthma control in Peruvian children. Respir Med. 2017 Dec; 133: 29-35.
16. Estela B, Navarro R, Eslava AB, Luis JJ, Monge S. Relación de la obesidad con el asma y la función pulmonar. Bol Med Hosp Infant Mex. 2011; 68: (3): 171-83.
17. Camargo CA, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult- onset asthma in women. Arch Intern Med. 1999 Nov; 159 (21): 2582-8.
18. Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. Vol. 108, J Appl Physiol. 2010; 108: 206-11 [cited 2021 Jun 19]. p. 206–11.
19. Cooper C, Kuh D, Egger P, Wadsworth M, Barker D. Childhood growth and age at menarche. Braz J Obstet Gynaecol. 1996 Aug; 103 (8): 814-7.
20. Polinski KJ, Liu J, Boghossian NS, Mclain AC. Maternal Obesity, Gestational Weight Gain, and Asthma in Offspring. Prev Chronic Dis. 2017 Nov; 14: E109.
21. Villalobos-Villalobos D, Osada-Liy J. Diagnostic value of the classification of obesity by race / ethnicity of reproductive-age women. Rev Cuerpo Med. 2014; 7 (3): 37-9.
22. Moral L, Vizmanos G, Torres-Borrego J, Praena-Crespo M, Tortajada-Girbés M, Pellegrini FJ. Asthma diagnosis in infants and preschool children: a systematic review of clinical guidelines. Allergol Immunopathol (Madr). 2019; 47 (2): 107-21.
23. Guidelines & Protocols Advisory Committee. Asthma in Children-Diagnosis and Management. [
Internet]. 2015 [access in 2021 Jul 3]. Available from:
http://www.bcchildrens.ca/Asthma-Site/Documents/CHBC%20and%20GPAC%20asthma-children-full-guideline.pdf24. Harpsøe MC, Basit S, Bager P, Wohlfahrt J, Benn CS, Nøhr EA. Maternal obesity, gestational weight gain, and risk of asthma and atopic disease in offspring: A study within the Danish National Birth Cohort. J Allergy Clin Immunol. 2013 Apr; 131 (4): 1033-40.
25. Harskamp-Van Ginkel MW, London SJ, Magnus MC, Gademan MG, Vrijkotte TG. A Study on Mediation by Offspring BMI in the Association between Maternal Obesity and Child Respiratory Outcomes in the Amsterdam Born and Their Development Study Cohort. PLoS One. 2015 Oct; 10 (10): e0140641.
26. Scholtens S, Wijga AH, Brunekreef B, Kerkhof M, Postma DS, Oldenwening M. Maternal overweight before pregnancy and asthma in offspring followed for 8 years. Int J Obes. 2010; 34 (4): 606-13.
27. Kaplowitz P. Delayed puberty in obese boys: Comparison with constitutional delayed puberty and response to testosterone therapy. J Pediatr. 1998; 133 (6): 745-9.
28. Shore SA. Obesity and asthma: cause for concern. Curr Opin Pharmacol. 2006 Jun; 6 (3): 230-6.
29. Rusconi F, Popovic M. Maternal obesity and childhood wheezing and asthma. Paediatr Respir Rev. 2017; 22: 66-71.
30. Simon A, Pratt M, Hutton B, Skidmore B, Fakhraei R, Rybak N. Guidelines for the management of pregnant women with obesity: A systematic review. Obes Rev. 2020; 21 (3): e12972.
Authors' contribution: Oviedo-Carquín V, Híjar-Zevallos C: Conceptualization, Data curation, Formal analysis, Methodology, Writing-original draft; Urrunaga-Pastor D: Formal analysis, Methodology, Writing-original draft; Herrera-Añazco P: Conceptualization, Methodology, Project administration and Supervision, Writing-original draft, Writing-review & editing.
All authors approved the final version of the article and declare no conflict of the interest.
Received on May 16, 2023
Final version presented on October 23, 2023
Approved on November 23, 2023
Associated Editor: Gabriela Buccini
 ; Cristhian Híjar-Zevallos2
; Cristhian Híjar-Zevallos2 ; Diego Urrunaga-Pastor3
; Diego Urrunaga-Pastor3 ; Percy Herrera-Añazco4
; Percy Herrera-Añazco4