ABSTRACT
OBJECTIVES: evaluate the association between the maternal near miss rate (TNMM) and sociodemographic and health care factors.
METHODS: this is an aggregated, cross- sectional epidemiological survey, with regression analysis and spatial analysis, with the units of analysis being the 399 municipalities that make up the four health macro- regions in the state of Paraná, Brazil. Data from the years 2018 to 2021 were obtained through the state maternal near miss report and monitoring system.
RESULTS: the state's total TNMM was 6.4 per 1,000 live births, with an increasing trend during the studied period (p<0.001). Sociodemographic and healthcare factors were not associated with TNMM, except for municipalities with a higher degree of urbanization (β adjusted=0.022; CI95%=0.002-0.041) and located in the northern health macro-region (β adjusted=12.352; CI95%= 10.779-15.099), demonstrated by clusters with high and positive associations (high-high).
CONCLUSION: the lack of association with sociodemographic and care factors may be due to their low effect on near miss, or the underreporting of near miss cases in the state. The differences found can be justified by the organization of health services and the intense regionalization of municipalities belonging to the macronorth, which have a better near miss report culture.
Keywords:
Near miss, Sociodemographic factors, Quality, access and evaluation of health care, Regionalization of health, Report
RESUMO
OBJETIVOS: avaliar a associação existente entre a taxa de near miss materno (TNMM) com fatores sociodemográficos e assistenciais de saúde.
MÉTODOS: trata-se de uma pesquisa epidemiológica agregada, transversal, com análises de regressão e análise espacial, sendo as unidades de análise os 399 municípios que compõem as quatro macrorregiões de saúde do estado do Paraná, Brasil. Os dados provenientes dos anos de 2018 a 2021 foram obtidos por meio do sistema estadual de notificação e monitoramento do near miss materno.
RESULTADOS: a TNMM total do estado foi de 6,4 por 1.000 nascidos-vivos, com tendência de aumento no período estudado (p<0,001). Fatores sociodemográficos e assistenciais não se associaram com a TNMM, exceto municípios com maior grau de urbanização (β ajustado=0,022; IC95%= 0,002-0,041) e localizados na macrorregião norte de saúde (β ajustado=12,352; IC95%= 10,779; 15,099), demonstrado por clusters com associações altas e positivas (high- high).
CONCLUSÃO: a ausência de associação com os fatores sociodemográficos e assistenciais podem decorrer do baixo efeito dos mesmos sobre o near miss, ou à subnotificação de casos de near miss materno no estado. As diferenças encontradas podem ser justificadas pela organização dos serviços de saúde e intensa regionalização dos municípios pertencentes à macronorte, os quais apresentam melhor cultura de notificação de near miss.
Palavras-chave:
Near miss, Fatores sociodemográficos, Qualidade, acesso e avaliação da assistência à saúde, Regionalização da saúde, Notificação
IntroductionThe Sustainable Development Goals institute mother and child care as one of their principal goals.
1 Although the reduction of mortality is more emphasized, the improvement of maternal care constitutes a more complex challenge, passing through morbidity indicators, especially in low income countries and/or countries with unfavorable sociodemographic conditions.
2,3 In this way, investigations on maternal near miss (MNM) stood out, due to its potential in helping the understanding of the maternal mortality phenomenon. Also, the capability of generating evidence that can be used for establishing strategies of reduction of both occurrences.
4,5MNM can be understood as a near death situation during pregnancy, delivery or up to 42 days after the end of pregnancy,
6 which is characterized by the presence of clinical, management and laboratory criteria, as instituted by the World Health Organization (WHO).
7 Many of the MNM criteria are avoidable, mainly due to the improvement of social and economic conditions, as well as those related to healthcare.
8 Therefore, as well as occurs with maternal mortality, the MNM rates (MNMR) are higher in developing countries than in developed countries.
5Since it is a subject not yet consolidated in health services, broad and standardized surveys regarding MNM are infrequent. Studies from countries with better social conditions and health care indicate lower MNMTs,
9,10 however, without the comprehension of the effect of each factor, such as income, education, health and prenatal assistance. This gap impairs the adoption of policies and actions that may prevent MNM, mainly when considering the need for optimization of resources in developing countries.
In this regard, considering the importance of the improvement of maternal care and the need of broad surveys concerning MNM, the present study aimed to assess the association of MNMR with sociodemographic and assistance factors in the state of Paraná, in the period between 2018 and 2021.
MethodsAggregate epidemiological survey, cross-sectional, with spatial analysis and regression analyses. The analysis units of the study were the 399 municipalities of the state of Paraná, located in the South Region of Brazil, with an estimated population of 11.8 million inhabitants in 2022. The state is organized into 22 Health Regions (HR) and these, in turn, are organized into 4 health macro-regions (HM).
Secondary data related to MNM reports, executed in the period between January 2018 and December 2021, were extracted from the Research Electronic Data Capture platform (REDCap). The REDCap is used by the secretariat of health of the state of Paraná for the organization of the information system of reports of MNM. The monitoring started in 2017, after qualifications and trainings in the whole state, and nowadays it is implemented in every health institution, private or public. Obtained data were screened for identification of repeated reports, using as criterion the number of the national health card of the patient. The number of live births (LB) of each municipality was obtained from the Liver Births Information System (Sinasc – Portuguese acronym), from the Department of Informatics of the Unified Health System (DATASUS – Portuguese acronym).
The dependent variable, MNMR, was calculated by means of the division of the number of MNM reports of women residing in each municipality, by the number of live births of women residing in the respective municipality, multiplied by 1000.
8 Besides the MNMR of each municipality, the calculation was performed in the entire state. The rates were calculated by year (2018, 2019, 2020 and 2021) and for all the period of analysis (2018-2021). The alteration of the MNMR was evaluated with the chi-square test for linear trend (Mantel-Haenszel), with the OpenEpi software.
The size of municipality; the degree of urbanization (DU) – which is the percentage of inhabitants living in the urban area; the Human Development Index (HDI);Gini Index (GI); the distance traveled by the woman from the municipality of origin to the hospital of MNM report; the coverage of Basic Care (BC) and the quality of prenatal care, measured by the amount of pregnant women with six or more consultations were considered as independent variables.
The variables size of municipality, DU, total HDI and respective dimensions were obtained at the Paraná Institute of Social and Economic Development (IPARDES – Portuguese acronym), referring to the year 2010, the most recent available datum. The Gini Index was extracted from the DATASUS databases, being also the most recent available datum, from the year 2010. The size of the municipality was categorized based on the residing population into size 1) <25,000 inhabitants, size 2) 25,000 to 99,999 inhabitants and size 3) ≥ 100,000 inhabitants. The distance between the municipality of residence and the notifying hospital was estimated by the Google maps software, considering data from the municipality of residence and the hospital available on REDCap.
The coverage of BC comprehended the percentage of the population of each municipality that possessed coverage of the Family Health Team and the Basic Care, based on data from January 2020 (half of the period of data collection). The coverage of pregnant women with six or more prenatal consultations was calculated by means of the division of the number of pregnant women with ≥ 6 consultations by the number of live births, and then multiplied by 100%. The BC coverage for January 2020 and the number of pregnant women with ≥ 6 prenatal consultations per each year of study were obtained from the Information and management system of the basic care – E- manager.
11The description of study variables was made by means of the presentation of the mean and total standard deviation and was stratified by size and MR, which were submitted, for non parametric data, in the Kolmogorov-Smirnov test, the Kruskal-Wallis test with pairwise comparison, and the Bonferroni correction. The analysis of factors associated with MNMR (from the total period of collection, 2018-2021) was performed by means of linear regression in order to obtain the beta quotient (β) and 95% confidence interval (CI95%). Adjusted analysis was performed by the statistically significant variables in the crude model (Gini index, degree of urbanization, coverage of ≥6 prenatal consultations and macro-regional) for achieving the adjusted β. The regression analyses were performed with the SPSS version 25.0 software.
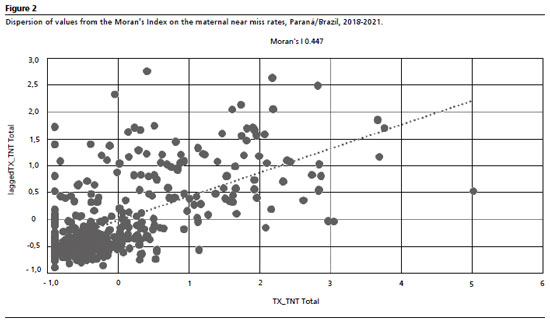
The spatial analysis aimed to verify the presence of possible spatial clusters from the Moran Index (ANSELIN, 2020) applied to MNMR for the period between 2018 and 2021. The spatial analyses were performed with the GeoDa version 1.18.10 software. The results of the Moran's Index varied from -1 to 1, being the positive values indicators of positive self-correlation (high-high) and the negative values, of negative self-correlation (low-low). All results passed by pseudo-significance tests, in which permutations were performed in order to verify the
p-value for
p<0.001.
The study was approved by the Research and Ethics Committee of the State University of Londrina (opinion number 4.793.951, CAAE: 46693821.4.0000.5231 of June 21, 2021) and the Research and Ethics Committee of the Health Secretariat of Paraná State (opinion number 4.952.539, CAAE: 46693821.4.3001.5225, September 3, 2021).
ResultsIn the study period, 3926 MNM reports were performed, which after the exclusion of the repeated ones, resulted in a 3893 MNM reports sample. Of the 399 municipalities of the state, in 72 municipalities, no resident was notified as MNM case in the four years of study, being all of them size 1 municipalities, with less than 18,000 inhabitants in the 2022 census.
The total MNMR of the state was 6.4MNM/1000LB. The MNMRs were 3.71/1000LB, 6.6/1000LB, 7.0/1000LB and 8.5/1000LB, in the years 2018, 2019, 2020 and 2021, respectively. It was observed an increasing trend in the study period (
p<0.001), including between the years 2019 to 2021 (
p<0.001).
The stratification of research variables by the size of municipalities evidenced important differences in relation to the sociodemographic and assistance factors, in which, in comparison with municipalities of size 1, the municipalities of sizes 2 and 3 demonstrated, generally, higher DU (
p<0.001) and better total HDI indicators (
p<0.001), however, with less coverage in the basic care (
p<0.001). Still in comparison with municipalities of size 1, the municipalities of size 2 demonstrated lower coverage for prenatal consultations (
p<0.002) (Table 1). In turn, the stratification by HM indicated higher heterogeneity, especially for MNMR, which was higher in the North HM than in the other HMs (
p<0.001) (Table1). Differences were also found between DU, basic care coverage and coverage of ≥6 prenatal consultations. In adjusted analyses, the North and West HMs demonstrated higher MNMR, compared to East HM, in which the capital of the state is located (Table 2).
The spatial analysis of the MNMRs demonstrated that, with the exception of the rates referring to 2018 (non-demonstrated data), the North macro-region presented the highest MNMR registries for the four years analyzed (Figure 1).
The analysis of the Moran's Index evidenced the spatial dependence between municipalities and neighboring areas (Figure 2). That is, municipalities with high MNMR also presented neighboring municipalities with high MNMR (high – high) and still, municipalities with low MNMR are also neighbored by municipalities with low MNMR (low-low). The analysis over the years of study (supplementary material) identified an increase in the self-correlation index over time, being considered low (0.187) in 2018, with an increasing trend in the following years (0.214, 0.377 and 0.344, respectively, in 2019, 2020 and 2021).
Lastly, the spatial distribution of the Moran's Index about the MNMR of the municipalities identified positive (high-high) and negative (low-low) spatial associations, in agreement with the Health Regionals (HR), especially with consolidated data from 2018 to 2021 (Figure 3), but also in the analyses of each year (data not shown). We highlight the clusters with high and positive associations referring to the municipalities of the North HM, encompassing the 17
th and 18
th HRs, besides part of the 19
th HR. Similarly, 59 municipalities composed clusters of low-low correlation, in four HRs that compose East HM (1
st, 2
nd, 3
rd and 5
th) and one HR (10
th HR) that composes the West HM.
DiscussionThe present study verified an increasing trend on the MNM reports during the 4 years of study, with mean MNMR of 6.4 MNM/1000LB. Sociodemographic and economic variables such as HDI, Gini Index, distance from the municipality of origin to the municipality of report, size of the municipality, coverage of basic care and prenatal consultations were not associated with MNMR, however higher MNMR were observed in municipalities with higher DU located in the North health macro-region.
The increase of MNMR over the period of data collection is a phenomenon observed in another study of temporal analysis,
12 and may be explained due to the greater discussion about the subject, the diffusion of the MNM conceptualization and the execution of qualifications and training for health professional teams. Considering that the phenomenon of the increase of reports occurs due to cultural issues related to training, it is expected that the same would occur homogeneously in the entire study region, obtaining similar values than other surveys about the subject in developing countries.
However, the values found were more approximated to that of surveys carried out in countries of medium income (mean MNMR of 7.8/1000LB), than those found in low/medium income countries (mean MNMR of 15.9/1000LB)
5, or in Brazil (MNMR varying from 9.4 to 10.2/1000LB).
13,14 These findings may be explained due to methodological differences, observing that Brazilian studies used incidence ratio to determine MNMR,
13,14 with a potential underreporting of MNMR cases in the system of report used in the present study, since the sociodemographic and economic conditions did not justify the differences found between the municipalities nor in relation to what is found in the literature.
8,12,15,16The non-association between MNMR with HDI and GI contradicted all results of analyses that associated higher income with lower MNMR, which is justified by the interaction of higher education and income, mainly in locations with low inequality, which may promote higher opportunities of care.
17-19 Possibly, the characteristics found in this study may be associated with higher late pregnancy and cesarean rates, confounding the benefic effects, besides limiting the sensibility of aggregate surveys carried out in more homogeneous locations, regarding such characteristics.
The distance to a high-complexity service,
20 the lower BC coverage (representative of the structuration of the health service)
21 and lower PN coverage
22 may represent higher risk of aggravation of health conditions of the pregnant/puerperal woman, and consequently higher MNMR.
20,22,23 Nevertheless, the structuration of the health service, with the regionalization and the early referral,
24 as well as the assistance coverage and priority care for regions with higher social vulnerability
25,25 may, as occurs with what is reported for economic and social variables, have diminished the effect of these variables about MNMR.
The DU of a given municipality represents, directly, the percentage of the population of the municipality residing in the urban area. However, the DU possesses several non-observable variables, such as economic structure of the municipality/region, presence or not of job opportunities in the urban area and, even not uniformly, the health assistance structure.
27 Notwithstanding, since municipalities with higher DU generally are central regional cities or neighbor of these, these municipalities tend to possess higher structure for healthcare.
28 Thus, considering that the performed analysis model adjusted the effect of DU by socioeconomic and assistance issues, the association found may come from a trend of MNM underreporting for women residing in municipalities with lower DU. In this case, since the analyses were adjusted by distance between the municipalities of residence and the report municipality, the association may be specifically due to the identification of these cases in rural areas, and not necessarily because of limitations of the referral of women.
The spatial analyses and those regarding HM, identified higher MNMR mainly in municipalities from the North macro-region of the state. Such differences seem to occur due to characteristics of the organization of health services,
29 since the analyses were adjusted for social and assistance confounding factors, and other spatial conditioning factors that may influence the occurrence of MNM were not identified. These findings demonstrate that municipalities belonging to North HM (18
th, 19
th and 22
th HR), present better structure for the collection of report of MNM cases, with potential underreporting for the other macro-regions, and, as mentioned above, in a more elevated rate in municipalities with lower DU.
We consider as a limitation in this study the fact of being carried out based on secondary data on MNM reports, which, as discussed above, may contain an important underreporting bias.
In addition, the study relied on a design that avoided a clear definition of causality (cross-sectional data) and the extrapolation of aggregate results for individuals (ecological fallacy), which lead the careful interpretation of findings to be necessary. However, we highlight the high number of reports performed, the adoption of international criteria for the identification of MNM, the execution of adjusted and spatial analyses, which tried to indicate explicative hypotheses for the results found.
Lastly, the results of the present study demonstrate that there was an increase in MNMR in the years between 2018 and 2021, which was strongly influenced by two demographic factors, the rate of urbanization of municipalities and residing in the North health macro-region.
MNM stands out as a sentinel event for the reduction of maternal deaths, since knowing the factors that determine it, as well as study the regions of occurrence, help managers in the decision making process regarding the elaboration of effective public policies for the reduction of this condition, that is still high, even though it is an unacceptable event nowadays.
References1. Maternal Health Task Force (MHTF).The sustainable development goals maternal and mortality. Boston: MHTF; 2017 [access in 2023 Jan 4]. Available from:
https://www.mhtf.org/topics/the-sustainable-development-goals-and-maternal-mortality2. World Health Organization (WHO). Fact sheet: maternal mortality. Geneva: WHO; 2019. [access in 2023 Jan 22]. Available from:
https://www.who.int/en/news-room/fact-sheets/detail/maternal-mortality3. Neves IAR, Maia MCW, Canto DF, Souza VS, Santarém MD, Oliveira JLC. Qualidade e segurança na assistência obstétrica: revisão integrativa da literatura. Rev Enferm UFPE. 2021; 15 (1): e245809.
4. Knight M, Acosta C, Brocklehurst P, Cheshire A, Fitzpatrick K, Hinton L,
et al. Beyond maternal death: improving the quality of maternal care through national studies of ‘near-miss' maternal morbidity. Southampton (UK): NIHR Journals Library; 2016.
5. Heitkamp A, Meulenbroek A, van Roosmalen J, Gebhardt S, Vollmer L, de Vries JI,
et al. Maternal mortality: near-miss events in middle-income countries, a systematic review. Bull World Health Organ. 2021 Oct; 99 (10): 693-707F.
6. Say L, Souza JP, Pattinson RC. Maternal near miss-towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009 Jun; 23 (3): 287-96.
7. World Health Organization (WHO). Evaluating the quality of care for severe pregnancy complications: the WHO near-miss approach for maternal health. Geneva: WHO; 2011. [access in 2023 Jan 4]. Available from:
https://apps.who.int/iris/bitstream/handle/10665/44692/9789241502221_eng.pdf?sequence=1&isAllowed=y8. Carvalho BAS, Andrade AGBF, Dantas AAS, Figueiredo IM, Silva JA, Rosendo TS,
et al. Temporal trends of maternal near miss in Brazil between 2000 and 2012. Rev Bras Saúde Mat Infant. 2019; 19 (1): 115-24.
9. O'Malley EG, Popivanov P, Fergus A, Tan T, Byrne B. Maternal near miss: what lies beneath? Eur J Obstet Gynecol Reprod Biol. 2016 Apr; 199: 116-20.
10. Donati S, Senatore S, Ronconi A, Regional Maternal Mortality Working Group. Obstetric near-miss cases among women admitted to intensive care units in Italy. Acta Obstet Gynecol Scand. 2012; 91 (4): 452-7.
11. Ministério da Saúde (BR). Secretaria de Atenção Primária à Saúde. E-Gestor AB- Informação e Gestão da Atenção Básica. Nota Técnica Nº 301/2022 CGESF/DESF/SAPS/MS. Nota Metodológica da Cobertura Potencial da Atenção Primária à Saúde no SUS. Brasília (DF): MS; 2022. [access in 2023 Jan 4]. Available from:
https://egestorab.saude.gov.br/image/?file=20221214_O_NT301-NotaMetodologicaCoberturaAPS_894545258772170154.pdf12. Herdt MCW, Magajewski FRL, Linzmeyer A, Tomazzoni RR, Domingues NP, Domingues MP. Tendência temporal do near miss e suas variações regionais no Brasil de 2010 a 2018. Rev Bras Ginecol Obstet. 2021; 43 (2): 97-106.
13. Oliveira FC Jr, Surita FG, Pinto e Silva JL, Cecatti JG, Parpinelli MA, Haddad SM,
et al. Severe maternal morbidity and maternal near miss in the extremes of reproductive age: results from a national cross- sectional multicenter study. BMC Pregnancy Childbirth. 2014 Feb; 14: 77.
14. Dias MAB, Domingues RMMD, Schilithz AOC, Nakamura-Pereira M, Diniz CSG, Brum IR,
et al. Incidência do near miss materno no parto e pós-parto hospitalar: dados da pesquisa Nascer no Brasil. Cad Saúde Pública. 2014; 30 (Supl. 1): S169-81.
15. Wasim T, Raana GE, Wasim M, Mushtaq J, Amin Z, Asghar S. Maternal near-miss, mortality and their correlates at a tertiary care hospital. J Pak Med Assoc. 2021 Jul; 71 (7): 1843-8.
16. Cecatti JG, Souza RT, Pacagnella RC, Leal MC, Moura EC, Santos LM. Maternal near miss among women using the public health system in the Amazon and Northeast regions of Brazil. Rev Panam Salud Publica. 2015 May; 37 (4-5): 232-8.
17. Andrade MS, Bonifácio LP, Sanchez JAC, Oliveira-Ciabati L, Zaratini FS, Franzon ACA. Morbidade materna grave em hospitais públicos de Ribeirão Preto, São Paulo, Brasil. Cad Saúde Pública. 2020; 36 (7): e00096419.
18. Chaves HLA, Gehlen VRF. Estado, políticas sociais e direitos sociais: descompasso do tempo atual. Serv Soc Soc. 2019; 135: 290-307.
19. Mattijssen L, Pavlopoulos D, Smits W. Does it pay off to specialize? The interplay between educational specificity, level and cyclical sensitivity. Soc Sci Res. 2023 Jan; 109 (1): 102782.
20. Menezes MO, Takemoto MLS, Nakamura-Pereira M, Katz L, Amorim MMR, Salgado HO,
et al. Risk factors for adverse outcomes among pregnant and postpartum women with acute respiratory distress syndrome due to COVID-19. Int J Gynaecol Obstet. 2020 Dec; 151 (3): 415-23.
21. García-Tizón Larroca S, Amor Valera F, Ayuso Herrera E, Cueto Hernandez I, Cuñarro Lopez Y, De Leon-Luis J,
et al. Human Development Index of the maternal country of origin and its relationship with maternal near miss: a systematic review of the literature. BMC Pregnancy Childbirth. 2020 Apr; 20 (1): 224.
22. Vaichulonis CG, Silva RR, Pinto AIA, Cruz IR, Mazzetti AC, Haritsch L,
et al. Evaluation of prenatal care according to indicators for the Prenatal and Birth Humanization Program. Rev Bras Saúde Mater Infant. 2021; 21 (2): 451-60.
23. Aleluia IRS, Medina MG, Almeida PF, Vilasbôas ALQ. Coordenação do cuidado na atenção primária à saúde: estudo avaliativo em município sede de macrorregião do nordeste brasileiro. Ciênc Saúde Colet. 2017; 22 (6): 1845-56.
24. Mendes EV. As redes de atenção à saúde. Brasília (DF): Organização Pan-Americana da Saúde; 2011. [access in 2022 Jan 4]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/redes_de_atencao_saude.pdf25. Bousquat A, Giovanella L, Fausto MCR, Medina MG, Martins CL, Almeida PF,
et al. A atenção primária em regiões de saúde: política, estrutura e organização. Cad Saúde Pública. 2019; 35 (Suppl. 2): e00099118.
26. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Gestação de alto risco: manual técnico. 5
th ed. Brasília (DF): Ministério da Saúde; 2012. [access in 2022 Jan 4]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/manual_tecnico_gestacao_alto_risco.pdf27. Santos Neto GC, Espírito Santo MM, Amaral TS, Fernandes DSO, Gomes AS, Pires MM. Pobreza e desigualdade de renda: uma análise para a região imediata de Ilhéus-Itabuna, Bahia, Brasil. Rev Bras Gestão Des Reg. 2021; 17 (1): 19-24.
28. Silva CR, Pinafo E. Macrorregião norte do Paraná: situação demográfica, socioeconômica e epidemiológica dos municípios. In: Carvalho BG, Almeida Nunes EFP, Cordoni Junior L, organizadores. Gestão da saúde em pequenos municípios: o caso do Norte do Paraná. Londrina: Eduel; 2018. p. 40-63.
29. Paraná. Secretaria de Estado da Saúde. Divisão de Atenção à Saúde da Mulher. Linha de cuidado materno infantil do Paraná: gestação. 8
th ed. Curitiba: SESA; 2022. [access in 20 Mai 2022]. Available from:
https://www.saude.pr.gov.br/sites/default/arquivos_restritos/files/documento/2022-03/linha_guia_mi-_gestacao_8a_ed_em_28.03.22.pdfAuthor's contribution: Curan FMS: study planning, data organization, elaboration of spreadsheets, data analysis, writing and critical reading of the manuscript.
Rodrigues R: elaboration of spreadsheets, data analysis, writing and critical reading of the manuscript.
Gioia TB: data analysis, critical reading of the manuscript.
Osis GG: study planning, data organization, writing and critical reading of the manuscript.
Pimenta RA, Pieri FM, Maciel SM and Pelloso SM: writing and critical reading of the manuscript.
Cardelli AAM: study planning, data analysis, reading and critical reading of the manuscript.
All authors approved the final version of the article and declare no conflicts of interest.
Received on April 17, 2023
Final version presented on February 9, 2024
Approved on February 15, 2024
Associated Editor: Luciana Dubeux
 ; Renne Rodrigues2
; Renne Rodrigues2 ; Thamy Bárbara Gioia3
; Thamy Bárbara Gioia3 ; Glaucia Gonçalves Osis4
; Glaucia Gonçalves Osis4 ; Rosângela Aparecida Pimenta5
; Rosângela Aparecida Pimenta5 ; Flavia Meneguetti Pieri6
; Flavia Meneguetti Pieri6 ; Sandra Mara Maciel7
; Sandra Mara Maciel7 ; Sandra Marisa Pelloso8
; Sandra Marisa Pelloso8 ; Alexandrina Aparecida Maciel Cardelli9
; Alexandrina Aparecida Maciel Cardelli9