ABSTRACT
OBJECTIVES: to estimate the detection rate of syphilis in pregnant women, the occurrence of congenital syphilis, and the rate of mother-to-child transmission of syphilis, in addition to analyzing missed opportunities in the prevention of mother-to-child transmission in the indigenous population.
METHODS: descriptive study of cases of pregnant indigenous women with syphilis resulting or not in a case of congenital syphilis. The data were obtained from the Sistema de Informação de Agravos de Notificação (Information System of Notifiable Diseases), the records of the Infecções Sexualmente Transmissíveis do Distrito Sanitário Especial Indígena (Sexually Transmitted Infections in the Special Indigenous Health District), and the medical records of pregnant indigenous women in 2015. The database and the calculation of syphilis rates in pregnant women, congenital syphilis, and mother-to-child transmission were carried out. Data on prenatal, diagnosis and treatment of syphilis during pregnancy were collected from the medical records.
RESULTS: the detection rate of syphilis in pregnant women reached 35.2/1,000 live births (LB), the occurrence of congenital syphilis encompassed 15.7/1.000 LB, and the rate of mother-to-child transmission was 44.8%. Six (24%) pregnant women started prenatal care in the first trimester and seven (28%) attended seven or more consultations. The diagnosis of syphilis was late and only nine (36%) women were properly treated.
CONCLUSIONS: failures in the diagnosis and the adequate treatment of pregnant women with syphilis compromised the prevention of mother-to-child transmission of the disease.
Keywords:
Health of indigenous populations, Prenatal care, Mother-to-child transmission of infectious disease, Congenital syphilis, Syphilis
RESUMO
OBJETIVOS: estimar a taxa de detecção de sífilis em gestantes, a incidência de sífilis congênita e a taxa de transmissão verticalda sífilis e analisar as oportunidades perdidas na prevenção da transmissão vertical na população indígena.
MÉTODOS:estudo descritivo de casos de gestantes indígenas com sífilis que tiveram ou não como desfecho um caso de sífilis congênita. Os dados foram obtidos do Sistema de Informação de Agravos de Notificação, dos registros da área de Infecções Sexualmente Transmissíveis do Distrito Sanitário Especial Indígena e dos prontuários de gestantes indígenas, no ano de 2015. Realizou-se o relacionamento da base de dados e cálculo de taxas de sífilis em gestantes, sífilis congênita e de transmissão vertical. Nos prontuários, coletaram-se dados do pré-natal, diagnóstico e tratamento da sífilis na gestação.
RESULTADOS: a taxa de detecção de sífilis em gestantes foi de 35,2/1.000 nascidos vivos (NV), a incidência de sífilis congênita, 15,7/1.000 NV e a taxa de transmissão vertical, 44,8%. Evidenciou-se que seis (24%) gestantes iniciaram o pré-natal no primeiro trimestre e sete (28%) realizaram sete ou mais consultas. O diagnóstico de sífilis foi tardio e apenas nove (36%) realizaram adequadamente o tratamento.
CONCLUSÕES: falhas no diagnóstico e no tratamento adequado de gestantes com sífilis comprometeram a prevenção da transmissão vertical da doença.
Palavras-chave:
Saúde das populações indígenas, Cuidado pré-natal, Transmissão vertical de doença infecciosa, Sífilis congênita, Sífilis
IntroductionCongenital syphilis (CS) is caused by the bacteria
Treponema pallidum and transmitted transplacentally or by the contact of the baby with active injuries through the birth canal. If not diagnosed or properly and timely treated, syphilis in pregnant women may lead to the risk of mother-to-child transmission (MCT) of the etiological agent.
1In 2014, the World Health Organization (WHO) defined the criteria to validate the elimination of mother-to-child transmission of syphilis and HIV. For syphilis, the impact encompasses a rate of congenital syphilis of ≤50/100,000 live births (LB). The process indicators address goals for a coverage reach of ≥ 95% of pregnant women with at least one prenatal consultation, the test of HIV/syphilis at the start of pregnancy, and adequate treatment – the latter is defined as at least one intramuscle application of 2.4 million benzylpenicillin benzathine units, at least 30 days before childbirth.
2In 2016, the WHO estimated the occurrence of over half a million (approximately 661 thousand) cases of congenital syphilis worldwide. Even though syphilis in pregnant women remained stable between 2012 and 2016, the number of cases among pregnant women and newborns remains unacceptably high.
3 In Brazil, the overview of syphilis is also worrying with a detection rate in pregnant women of 21.6/1.000 LB and an occurrence rate of congenital syphilis of 7.7 cases/1.000 LB in 2020.
4The prenatal care of pregnant women with syphilis encompasses serological detection, correct and timely treatment, and stimulus to the father or partner’s participation throughout the prenatal care and eventual syphilis treatment.
1 These interventions are promoted by the
Atenção Primária à Saúde (APS) (Primary Healthcare) and demand low-cost technologies that are admittedly efficient and cost-effective, with fewer adverse effects for the pregnancy, as well as reduced stillbirths, neonatal deaths, and complications for the health of the baby with congenital syphilis (CS).
5Despite the expansion of prenatal coverage in Brazil, access to consultations is unequally distributed, revealing difficulties of facing social and ethno-racial inequalities, especially among women with lower schooling living in the North and Northeast of the country and women of black and indigenous race/ skin color.
6,7 Such unequal access to prenatal care and syphilis exams represent difficulties in the implementation of protocols to reduce mother-to-child transmission of the infection.
8In Brazil, the indigenous populations experience a situation of vulnerability and epidemiological invisibility characterized by an underreporting of syphilis cases in pregnant women and congenital syphilis, in addition to a low percentage of prenatal actions and tests for syphilis diagnosis among indigenous women compared with non-indigenous populations.
7,9,10Such a scenario reveals ethno-racial inequalities experienced by the indigenous population and the challenges related to the institution of culturally sensitive routines for the diagnosis and adequate treatment of Sexually Transmitted Infections (STIs) in the scope of
Distritos Sanitários Especiais Indígenas (DSEI) (Special Indigenous Health Districts) carried out by the
Equipes Multidisciplinares de Saúde Indígenas (EMSI) (Multidisciplinary Teams of Indigenous Health) in the villages.
7,11,12In this sense, this article aims to estimate the detection rate of syphilis in pregnant women, the occurrence of congenital syphilis, and the mother-to-child transmission rate of syphilis, in addition to analyzing the missed opportunities in the prevention of mother-to-child transmission of syphilis in the indigenous population in Mato Grosso do Sul.
MethodsThis is a descriptive study on cases of pregnant indigenous women with syphilis resulting or not in a reported case of early congenital syphilis attended by the EMSI in Mato Grosso do Sul in 2015.
The state indigenous population is composed of 73,295 self-declared individuals,
13 representing the second largest in Brazil. Prenatal care is promoted by the EMSI acting in 75 villages and 26 indigenous settlements linked to 14 Reference Centers and the
Distrito Sanitário Especial Indígena de Mato Grosso do Sul (DSEI/MS) (Special Indigenous Health District of Mato Grosso do Sul) responsible for the Primary healthcare and the operational units of the
Subsistema de Atenção à Saúde Indígena (SASI) (Indigenous Health care Subsystem , linked to the
Sistema Único de Saúde (SUS) (Public Health System).
The cases of syphilis in pregnant women and congenital syphilis were separately identified through a nominal search on the
Sistema de Informação de Agravos de Notificação (Sinan) (Information System of Notifiable Diseases) and the IST/DSEI/MS base. From the Sinan, we selected cases of syphilis during pregnancy and congenital syphilis in individuals of indigenous
race/skin color between January 1, 2015, and December 31, 2015. On the IST/DSEI/MS base, which is supplied by the transference of records of services of the EMSIs in indigenous villages and settlements to manage the IST/DSEI/MS, we searched the records of syphilis in pregnant women and congenital syphilis, both for the same period. It is worth to highlight that the EMSIs also fills out the notification form for syphilis in pregnant women and/or congenital syphilis to be sent to the municipal epidemiological surveillance where the indigenous lands are located.
The classification of women as cases of syphilis during pregnancy also considers the newborn’s (NB) mother with a report of congenital syphilis, which was neither reported on the Sinan nor appeared in the records of the IST/DSEI/MS.
We performed the linkage
and
visual inspection of the database for pregnant women with syphilis by adding those without a record or report of syphilis during pregnancy whose NB was reported as a case of congenital syphilis. The linkage was performed based on a key composed of the following aggregation for pregnant women with syphilis: “pregnant women’s name”, “pregnant women’s date of birth”, “date of diagnosis”, and “date of the report”, and the aggregation “mother’s name” and “date of newborn’s birth” for early congenital syphilis. After linking the Sinan and IST/DSEI/MS databases and excluding three cases of congenital syphilis with duplicate reporting on different dates on the Sinan, we proceeded with the aggregation of the cases contained in only one of the databases, with 67 cases of pregnant women with syphilis and 30 cases of NBs with congenital syphilis.
The detection rate of syphilis in indigenous pregnant women in 2015 was calculated based on the ratio between the total number of reported cases in both data sources and those not identified but whose NBs had congenital syphilis by the number of live births of indigenous mothers from villages and settlements, multiplied by 1.000.
The occurrence rate of congenital syphilis was based on the total number of reported cases of early congenital syphilis in both data sources by the total number of live births by indigenous mothers living in villages and settlements multiplied by 1.000.
The number of live births was extracted from records of the
Áreas Técnicas de Saúde da Mulher e da Criança do DSEI/MS (Technical Areas of Woman and Child Health of the DSEI/MS) encompassing only the live births in villages and settlements of indigenous communities attended by the district, differently from the
Sistema de Informação de Nascidos Vivos (Sinasc) (Live Births Information System), which contains all live births of residents in indigenous communities, both urban and villages.
The rate of mother-to-child transmission of syphilis was calculated considering the number of cases of early congenital syphilis in indigenous women as the counter and the cases of pregnant indigenous women with syphilis registered on the Sinan and the technical area of the IST/DSEI/MS as the denominator, as well as those that were not reported or registered whose NBs had a diagnosis of congenital syphilis.
We collected data from 25 medical records of indigenous pregnant women whose pregnancy resulted in a case of congenital syphilis. It was not possible to analyze five medical records, four of those were not found and one contained no prenatal data.
The medical records were sent to the Reference Centers and analyzed from May 2 to August 31, 2018, using an instrument prepared based on the
Protocolo Clínico e Diretrizes Terapêuticas para a Prevenção da Transmissão Vertical da Sífilis14 (Clinical Protocol and Therapeutic Guidelines for the Prevention of Mother-to-child transmission of Syphilis), addressing the following variables: pregnant women’s age , number of pregnancies, diagnosis and treatment of syphilis in previous pregnancies, gestational age at the beginning of the prenatal, and the number of consultations attended. The treponemal tests – Rapid Test (RT) and ELISA – are performed at the first prenatal consultation, and the latter is available at the 1
st Screening phase of the
Triagem do Programa Estadual de Proteção à Gestante do Instituto de Pesquisas, Ensino e Diagnósticos da Associação de Pais e Amigos dos Excepcionais (PEPG/Iped-Apae) (State Program of Protection to Pregnant Women of the Research, Teaching, and Diagnosis Institute of the Association of Parents and Friends of Special Children). In the PEPG, pregnant women with reagent results in the ELISA are recalled for a blood sample collection via peripheral venipuncture to confirm the diagnosis through a non-treponemal test at the Venereal Disease Research Laboratory
(VDRL).
According to Table 1, the variables related to the treatment of syphilis were clinical classification of syphilis and the treatment of pregnant women and partners.
The data from the medical records were inserted and arranged on Microsoft Office Excel 2010 and analyzed through descriptive statistics to be presented in tables with absolute values to characterize the trajectories of indigenous pregnant women with syphilis in 2015.
This study was approved by the Research Ethics Committee and National Research Ethics Commission (CONEP), Document number no. 2,155,788.
ResultsIn 2015, 1.900 live births of indigenous residents of the state villages and settlements were registered. Out of these LBs, 30 were reported as congenital syphilis, represented by an occurrence rate of 15.7/1.000 LB. There were 67 cases of syphilis in pregnant indigenous women, corresponding to a detection rate of 35.2 /.,000 NV and a mother-to-child transmission (MCT) rate of 44.8%.
Only ten cases (14.9%) of syphilis in pregnant women and 15 (50%) of congenital syphilis were detected on the Sinan. The IST/DSEI/MS showed records of other 23 (34.3%) cases of syphilis in pregnant women and six (20%) of early congenital syphilis. Thirty-three cases of syphilis in pregnant women (49.2%) and nine (30.0%) of congenital syphilis were reported on both databases. One case (1.5%) of a mother of NB with congenital syphilis appeared neither in the Sinan report nor the records of the IST/DSEI/MS (Table 2).
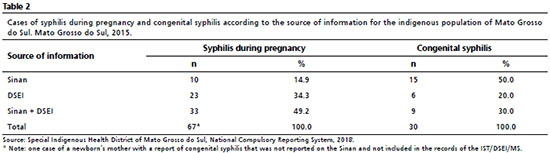
Table 3 summarizes the trajectory of the 25 medical records of pregnant indigenous women resulting or not in a case of congenital syphilis in 2015. The age interval ranged from 12 to 40 years, with an average age of 24 years, nineteen (76%) were multiparous (from one to seven children), three (12%) were nulliparous, and three (12%) showed no information in the medical records. As for the diagnosis and treatment of syphilis in previous pregnancies, 12 (48%) had no previous history of syphilis, eight (32%) had a record of diagnosis and treatment of syphilis, and five (20%) showed no information (data not included in the table).
Regarding the current pregnancy, only six (24%) had started prenatal care in the first trimester and seven (28%) attended seven or more consultations (Table 3).
As for the treponemal tests, the medical records of the UBSI had a record of eight (32%) rapid tests (four with reagent results and other four non-reagents) and 21 (84%) exams of 1
st Screening phase from the PEPG/Iped-Apae (sixteen reagents and five non-reagents). In turn, the non-treponemal test had a record of eighteen (72%) VDRL (ten with titration higher than or equal to 1:4, two with non-reagent results, and six with low titrations (1:1, 1:2) – the latter can be a serological scar of pregnant women with the previous diagnosis of syphilis (Table 3).
As for the diagnosis of syphilis, eighteen (72%) received the diagnosis during prenatal care (five in the first trimester of pregnancy, nine in the second, and four in the third), and six (25%) had a record of syphilis at the admission in the maternity (three with reagent result in the rapid test in the maternity, two with low titration of VDRL – one 1:1 and another 1:4 –, and one showed no exam result information) (Table 3). For the women with the diagnosis of syphilis during the prenatal, there was an average time interval of approximately five weeks between the first prenatal consultation and the date of syphilis diagnosis.
Despite appearing the adequate treatment of pregnant women and partners, the newborns in cases 3 and 10 were considered cases of congenital syphilis for presenting a reagent result at birth. The medical records of cases 12, 13, and 24 contained records of non-reagent results or not informed neither for prenatal nor childbirth, despite the diagnosis of the gestational trimester or puerperium, as well as the adequate or inadequate treatment of pregnant women, respectively. Cases 14 and 15 showed reagent results for the 1
st Screening phase from the PEPG/Iped-Apae, inadequate or adequate treatment of pregnant women and partners, untreated or without a record of treatment, respectively. Case 23 had neither report of prenatal care nor childbirth of newborn with congenital syphilis both on the Sinan and the IST/DSEI/MS.
Only nine (36%) pregnant women were properly treated and eleven (44%) were improperly treated (two quit the treatment and nine started the treatment less than 30 days before childbirth), and five (20%) had no record of treatment in the records (Table 3).
Three (12%) medical records of pregnant women contained a record of adequate treatment of the partner, and ten (40%) showed a lack of treatment for the partner. As for the pregnancy outcome, all were live births, with three premature NBs and two NBs with low weight at birth (< 2,500 grams) (Table 3).
DiscussionPrenatal care among indigenous pregnant women that resulted in a case of congenital syphilis revealed failures in the effort to start prenatal care in the first trimester and the number of consultations for normal-risk pregnancy. It is worth to highlight that the clinical care for the management of syphilis presented some important barriers to the control of mother-to-child transmissions, such as late laboratory diagnosis with a large interval between the exam, the diagnosis, and the treatment establishment (around five weeks), which could partly explain the missed opportunities of preventing the transmission.
Herein, the detection rate of syphilis in pregnant indigenous women was superior to the national (21.6/1.000 LB) and the state of Mato Grosso do Sul (30.8/1.000 LB) rates registered in 2020. The occurrence rate of congenital syphilis in the indigenous population was also high, around twice as high as the national (7.7/1.000 LB) and the state (5.4/1.000 LB) rates for 2020.
4Tiago
et al.,
9 found different results when investigating the indigenous population of Mato Grosso do Sul, with higher rates of syphilis in pregnant women than between 2011 and 2014, with the highest record in 2014 (41.1/.1000 LB). In contrast, the rates of congenital syphilis were lower for the same period, with the lowest record in 2011 (6.0/.1000 LB). The high rate of congenital syphilis found in our study may indicate that women with gestational syphilis were not properly treated to block fetal transmission.
A systematic review on the STIs in indigenous peoples and Afro-Brazilians in Latin America,
15 between January 2000 and April 2016 revealed a prevalence of syphilis of 7% in indigenous pregnant women from Bolivia, 1.6% in the Peruvian Amazon, and 2% in Brazil. The detection rate of syphilis found herein is within the interval of the prevalence values identified in the systematic review, varying from 1.6 to 7%.
The underreporting of cases of syphilis in pregnant indigenous women on the Sinan may be related to the identification of problems of data transference between the Reference Centers and the municipal epidemiological surveillance, where the indigenous lands are located, reflecting a difference in the total of cases between the DSEI/MS database and the city, state, and federal bases.
Additionally, some potential completeness mistakes of variables in the report form for pregnant women with syphilis and congenital syphilis are highlighted, especially concerning the indigenous variables race/skin color and case completion. The absence of records of congenital syphilis with negative perinatal outcomes, such as fetal death and neonatal death, may reflect the underreporting of cases and hamper the characterization of iniquity health situations and the establishment of strategies to face the morbimortality related to congenital syphilis in the indigenous population.
A study in the city of Recife (State of Pernambuco), between 2010 and 2016, addressed the underreporting of fetal and infant deaths by congenital syphilis on the Sinan and the
Sistema de Informação sobre Mortalidade (SIM) (Mortality Information System). The authors detected 80.9% of underreporting of death by congenital syphilis on the Sinan, with 29.5% unreported deaths and 51.4% of reports with no record of progression to death, and a 7% underreporting of fetal or infant death by congenital syphilis on the SIM.
16The mother-to-child transmission rate of syphilis in the indigenous population was higher than 40%, similarly to results found in other studies whose national transmission rates between 2011 and 2012 and in Rio de Janeiro, in 2007/2008, reached 34.3% and 34.8%, respectively.
17,18Combined with prematurity and low birth weight, the high rate of mother-to-child transmission indicates failures in prenatal care that may be related to the capacity of the service to attract indigenous women to an early prenatal start, as well as adequate and timely support and care for the treatment of pregnant women in an intercultural context that considers the articulation of the systems of indigenous and non-indigenous health.
19In addition to these barriers experienced by indigenous and non-indigenous women, there are other factors related to the management of syphilis during pregnancy that may be associated with the care failures resulting in congenital syphilis in women with low schooling, black race/skin color, pregnant women with the diagnosis of syphilis on the third gestational trimester or at the admission for childbirth, most with inadequate treatment,
20 fewer consultations, and serological exams.
17National data show that among the cases of congenital syphilis registered in 2020, 12.5% of the mothers received prenatal care, 33.6% had a diagnosis of the infection at childbirth/curettage, 50.6% were not properly treated, and 30.9% received no treatment at all.
4Redesigning the care trajectory of pregnant women has revealed situations of health vulnerability and inequalities (late prenatal care start, low number of pregnant women attending seven or more consultations, and previous history of syphilis) characterized by poor access to prenatal care and failures in the adequate monitoring of syphilis management in indigenous territories by the SASI-SUS. Garnelo
et al.,
7 also identified such a scenario, as well as Mesenburg
et al.,
21 in the
Inquérito Nacional de Saúde e Nutrição dos Povos Indígenas (National Survey of Health and Nutrition of Indigenous People), by comparing the ethnical groups of 16 countries in Latin America and Caribe.
The STIs in the indigenous villages of Mato Grosso do Sul have been investigated since 2012
22 gradually including the Rapid Tests (RTs) for HIV and syphilis. However, even after around two years of the RT implementation, its low record in the medical records and the large interval between the 1
st Screening phase from the PEPG/Iped-Apae and the delivery of results may partly explain the permanence of negative outcomes of congenital syphilis.
The RT availability to investigate syphilis in pregnant women in Latin America and Caribe has been increasing since 2010 favoring the treatment start when combined with the non-treponemal test on the same day in communities with difficult access to prenatal services.
23 In Brazil, it is recommended to use the RT during the first and third trimesters of pregnancy and at childbirth as a strategy to minimize missed opportunities for testing and treatment of pregnant women for syphilis.
1Detecting a diagnosis of syphilis during pregnancy favors timely interventions to preserve the health of both the woman and the fetus. Thereby, it is worth emphasizing the importance of the records and prenatal communication instrument card by the professionals of the EMSI who monitor these women in the villages, as well as by the childbirth care teams regarding the diagnosis and conducts to prevent mother-to-child transmission.
The low number of pregnant women and partners who are properly treated is a worrying aspect that may increase the risks of early congenital syphilis, as indicated by Padovani
et al.
24The treatment of both pregnant women and their partners should be practiced in the
Unidades de Saúde da Família Indígena (Indigenous Family Health Units) in the villages during the prenatal care promoted by the EMSI. However, both the access and quality of prenatal care and the insufficient availability of diagnosis and monitoring exams for pregnant women seem to weaken the prevention actions of mother-to-child transmission of syphilis.
The number of women with the diagnosis of syphilis at admission in the maternity ward is also a cause of concern, as well as others whose pregnancy resulted in congenital syphilis even upon the diagnosis during prenatal care. Therefore, it is indispensable to question the quality of prenatal care since it may be associated with poor knowledge of the service protocols and difficulties in approaching STIs, requiring health professionals to have technical and specific knowledge of the sociocultural aspects of the community. Such a scenario also appeared in a study
25 addressing the perspective of nurses regarding clinical and laboratorial care, and health promotion actions in an intercultural context to prevent mother-to-child transmission of syphilis in the indigenous population in Mato Grosso do Sul.
Another important issue is that professionals must notify and treat cases of congenital syphilis even upon the uncertainty of the child’s care continuity in the health services network. It is essential to use reference and contra reference instruments and provide diagnosis exams that allow for both an adequate monitoring of the child until 18 months of age and a correct case report.
14,26Furthermore, it is worth to highlight some other important factors that may have contributed to such a situation, like the high proportion of indigenous women with a late initiation of prenatal, low use of rapid tests, delayed exam results, and a potential shortage of penicillin benzathine between 2014 and 2016 in several countries, including Brazil, which may have caused the disease to grow among the population. A study on the shortage of penicillin according to its temporal evolution and spatial distribution in Rio de Janeiro, from 2013 to 2017, detected that the shortage affected the inhabitants differently, being more intense in 2014, 2015, and 2017, especially in the poorest neighborhoods with higher rates of gestational and congenital syphilis.
27Herein, the adequate treatment of indigenous pregnant women and their partners was considered a criterion to define congenital syphilis and an essential measure to prevent congenital syphilis in indigenous villages, as pointed out by Victora
et al.
28 as a major challenge that persists in the mother-child health scope.
It is worth emphasize the change in the definition criteria for syphilis in 2017, excluding the simultaneous treatment of the sexual partner as a criterion to define the adequate treatment of pregnant women, considering only the complete treatment of pregnant women with penicillin, according to the clinical phase of the disease and started at least 30 days before childbirth.
29Despite the treatment of the sexual partner is relevant to control the transmission of syphilis and prevent the reinfection of pregnant women and mother-to-child transmission, it does not imply that cases of congenital syphilis are reported.
26The analysis of secondary data represents a limitation of this study and is related to the lack of identification of pregnant women medical records, representing a loss of five cases of congenital syphilis (16.6%). Four medical records referred to pregnant indigenous women from state settlements and one had no records of prenatal care. The lack of physical structure to preserve the medical records in these locations may lead to tracking losses.
Another limitation may be associated with the lack of a link between the data from the Sinan and the SIM and data from the
Sistema de Informações Hospitalares (SIH) (Hospital Information System) to detect potential cases of miscarriage, fetal death, and neonatal death by syphilis.
The range of the detection rates of syphilis during pregnancy and the occurrence of congenital syphilis, the reduced prenatal care, and the failures in the diagnosis and treatment of syphilis highlight the need to improve the monitoring and definition of a routine to investigate the repercussions of the disease both for the mother and the newborn, in addition to enlarging prevention actions against mother-to-child transmission.
AcknowledgmentsWe are grateful for the financial support of the research carried out through the public notice FUNDECT/DECIT-MS/CNPq/SES/Nº03/2016 – Research Program for the SUS (PPSUS-MS).
References1. Domingues CSB, Duarte G, Passos, MRL Sztajnbok, DCN, Menezes MLB. Protocolo Brasileiro para Infecções Sexualmente Transmissíveis 2020: sífilis congênita e criança exposta à sífilis. Epidemiol Serv Saúde. 2021; 30 (Esp 1): e2020597.
2. World Health Organization (WHO). Global guidance on criteria and processes for validation: elimination of mother-to-child transmission of HIV and syphilis. 2nd ed. Geneva: WHO; 2017. [access in 2017 abr 16]. Available from:
https://www.who.int/publications/i/item/97892400393603. Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané G, et al. Global burdenof maternal and congenital syphilis and associated adverse birth outcomes-Estimates for 2016 and progress since 2012. PLOS ONE. 2019; 14 (7): e219613.
4. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Boletim Epidemiológico da Sífilis Brasília (DF): Ministério da Saúde; 2021. [access in 2017 abr 16]. Available from:
https://www.gov.br/aids/pt-br/centrais-de-conteudo/boletins-epidemiologicos/2021/sifilis/boletim_sifilis_2021_internet.pdf/view5. Hawkes S, Matin N, Broutet N, Low N. Effectivenessofinterventionsto improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infec Dis. 2011;11:684-91.
6. Viellas EF, Domingues RMSM, Dias MAB, Gama SGN, Theme MM FA, Costa JV,
et al. Assistência pré-natal no Brasil. Cad Saúde Pública. 2014; 30 (Suppl. 1): S1-15.
7. Garnelo L, Horta BL, Escobar AL, Santos RV, Cardoso AM, Welch J,
et al. Avaliação da atenção pré-natal ofertada às mulheres indígenas no Brasil: achados do Primeiro Inquérito Nacional de Saúde e Nutrição dos Povos Indígenas. Cad Saúde Pública. 2019; 35 (Suppl. 3): e00181318.
8. Freitas CHSM, Forte FDS, Galvão MHRG, Coelho AA, Roncalli AG, Dias SMF. Inequalities in accessto HIV andsyphilistests in prenatalcare in Brazil. Cad Saúde Pública. 2019; 35 (6): e00170918.
9. Tiago ZS, Pícoli RP, Graeff S VB, Cunha RV, Arantes R. Subnotificação de sífilis em gestantes, congênita e adquirida entre povos indígenas em Mato Grosso do Sul, Brasil, 2011-2014. Epidemiol Serv Saúde. 2017; 26 (3): 503-12.
10. Benzaken AS, Sabidó M, Brito I, Bermúdez XPD, Benzaken NS, Galbán E,
et al. HIV and syphilis in the context of community vulnerability among indigenous people in the Brazilian Amazon. Int J Equity Health. 2017; 16 (1): 92.
11. Anderson I, Robson B, Connolly M, Al-Yaman, F,Bjertness E, King A, et al. Indigenous and tribal peoples’ health (The Lancet–Lowitja Institute Global Collaboration): a population study. Lancet. 2016 Jul; 388 (10040): 131-57.
12. Mendes APM, Leite MS, Langdon EJ, Grisotti, M. O desafio da atenção primária na saúde indígena no Brasil. Rev Panam Salud Publica. 2018 Nov; 42 (184): 1-6.
13. Instituto Brasileiro de Geografia e Estatística (IBGE). Os indígenas no censo demográfico 2010. Brasília (DF): IBGE; 2010. [access in 2017 abr 16]. Available from: http://
http://www.ibge.gov.br/indigenas/indigena_censo2010.pdf14. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância, Prevenção e Controle das Infecções Sexualmente Transmissíveis, do HIV/Aids e das Hepatites Virais. Protocolo Clínico e Diretrizes Terapêuticas para Prevenção da Transmissão Vertical de HIV, Sífilis e Hepatites Virais. Brasília (DF): Ministério da Saúde; 2015. [access in 2017 abr 16]. Available from: Preventing mother-to-child transmission of syphilis in the indigenous population Rev. Bras. Saúde Mater. Infant., Recife, 22 (4): 823-831 oct-dec., 2022 831 Received on July 21, 2021 Final version presented on June 8, 2022 Approved on June 10, 2022
http://antigo.aids.gov.br/pt-br/pub/2022/protocolo-clinico-e-diretrizes-terapeuticas-para-prevencao-da-transmissao-vertical-de-hiv15. Russell NK, Nazar K Pino S, Gonzalez MA, Bermúdez XPD, Ravasi G. HIV, syphilis, and viral hepatitisamongLatin American indigenouspeoplesand Afro-descendants: a systematic review. Rev Panam Salud Publica. 2019 Jan; 43: e17.
16. Belo MMA, Oliveira CM, Barros SC, Maia LTS, Bonfim CV. Estimativa da subnotificação dos óbitos por sífilis congênita no Recife, Pernambuco, 2010-2016: relacionamento entre os sistemas de informações sobre mortalidade e de agravos de notificação. Epidemiol Serv Saúde. 2021; 30 (3): e2020501.
17. Domingues RMM, Leal MC. Incidência de sífilis congênita e fatores associados à transmissão vertical da sífilis: dados do estudo Nascer no Brasil. Cad Saúde Pública. 2016; 32 (6). e00082415.
18. Domingues RMSM, Saraceni V, Hartz ZMA, Leal MC. Sífilis congênita: evento sentinela da qualidade da assistência pré-natal. Rev Saúde Pública. 2013, 47 (1): 147-57.
19. Ruffinen CZ, Sabidó M, Díaz-Bermúdez XP, Lacerda M, Mabey D, Peeling RW,
et al. Point-of-carescreening for syphilisand HIV in theborderlands: challenges in implementation in theBrazilianAmazon. BMC Health Serv Res. 2015;15: 495.
20. Heringer ALS, Kawa H, Fonseca SC, Brignol SMS, Zarpellon LA, Reis AC. Desigualdade na tendência da sífilis congênita no município de Niterói, Brasil 2007 a 2016. Rev Panam Salud Publica. 2020; 44: e8.
21. Mesenburg MA, Restrepo-Mendez MC, Amigo H, Balandrán AD, Barbosa-Verdun MA, Caicedo-Velásquez B,
et al. Ethnicgroupinequalities in coveragewithreproductive, maternal andchildhealthinterventions: cross-sectionalanalysesofnationalsurveys in 16 Latin American andCaribbean countries. Lancet Global Health. 2018; 6: e902-13.
22. Graeff SVB, Pícoli RP, Arantes R, Cunha RV, Castro VOL. Aspectos epidemiológicos da infecção pelo HIV e da aids entre povos indígenas. Rev Saúde Pública. 2019; 53: 71.
23. Benzaken AS, Sabidó M, Galban E, Pedroza V, Araújo AJ, Peeling RW,
et al. Field performance of a rapid point-of-care diagnostictest for antenatal syphilis screening in the Amazon region, Brazil. Int J STD AIDS. 2011 Jan; 22 (1): 15-8.
24. Padovani C, Oliveira RR, Pelloso SM. Syphilis in duringpregnancy: associationof maternal and perinatal characteristics in a region of southern Brazil. Rev Latino-Am Enferm. 2018; 26: e3019.
25. Pícoli RP, Cazola LHO. Ações de prevenção da transmissão vertical da sífilis ofertada à população indígena. Cogitare Enferm. 2020; 25: e69552.
26. Soares MAS, Aquino R. Associação entre as taxas de incidência de sífilis gestacional e sífilis congênita e a cobertura de pré-natal no Estado da Bahia, Brasil. Cad Saúde Pública. 2021; 37 (7): e00209520.
27. Araujo RS, Souza ASS, Braga JU. A quem afetou o desabastecimento de penicilina para sífilis no Rio de Janeiro, 2013–2017? Rev Saúde Pública. 2020; 54: 109.
28. Victora CG, Aquino EM, Leal MC, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 Mai; 377 (9780): 1863-76.
29. Ministério da Saúde (BR). Departamento de Vigilância, Prevenção e Controle das Infecções Sexualmente Transmissíveis, do HIV/AIDS e das Hepatites Virais. Secretaria de Vigilância em Saúde, Ministério da Saúde. Nota Informativa nº 2, de 19 de setembro de 2017. Altera os critérios de definições de casos para notificação de sífilis adquirida, sífilis em gestantes e sífilis congênita. Brasília (DF): Ministério da Saúde; 2017. [access in 2020 abr 16]. Available from:
http://antigo.aids.gov.br/pt-br/legislacao/nota-informativa-no-02-sei2017-diahvsvsmsReceived on July 21, 2021
Final version presented on June 8, 2022
Approved on June 10, 2022
Authors’ contribution: Pícoli RP contributed to the manuscript preparation with research design and planning; draft preparation, critical review of content, and final approval. Cazola LHO contributed to the manuscript preparation with data interpretation, draft preparation, critical review of content, and final approval.
All authors declare no conflict of interest.