ABSTRACT
OBJECTIVES: to analyze the level of anxiety in high risk pregnant women admitted in the maternity ward of the Hospital Universitário Lauro Wanderley (HULW) of the Federal University of Paraíba.
METHODS: an observational, descriptive, cross-sectional study of quantitative character, with a sample composed of 100 pregnant women diagnosed as high risk interned at HULW. Data collection was performed using the Beck Anxiety Inventory (BAI), used to assess the level of anxiety the patient is in and the existing symptoms. For the statistical analysis, the Mann Whitney, Kruskal Wallis and Spearman correlation tests were used, considering p<0.05.
RESULTS: it was observed that 68% of pregnant women have moderate to high anxiety, with heat, fear of the worst happening, faster heartbeat, emotional instability and nervousness listed as the most common symptoms. The presence of an anxious condition was independent of maternal age, marital status or parity, however the gestational trimester, history of abortions and length of hospital stay were identified as risk factors for anxiety.
CONCLUSION: pregnant women with a high risk diagnosis hospitalized at HULW presented anxiety, thus identifying the need for a multiprofessional support network, such as family assistance.
Keywords:
Anxiety, Hospitalization, High risk pregnancy
RESUMO
OBJETIVOS: analisar o nível de ansiedade em gestantes de alto risco internadas na maternidade do Hospital Universitário Lauro Wanderley (HULW) da Universidade Federal da Paraíba.
MÉTODOS: estudo observacional, descritivo, transversal de caráter quantitativo, com amostra composta por 100 gestantes com diagnóstico de alto risco internadas no HULW. A coleta de dados foi realizada por meio do Inventário de Ansiedade de Beck (BAI), utilizado para avaliar o nível de ansiedade do paciente e os sintomas existentes. Para a análise estatística, foram utilizados os testes de Mann Whitney, Kruskal Wallis e correlação de Spearman, considerando p<0,05.
RESULTADOS: observou-se que 68% das gestantes apresentam ansiedade moderada a alta, com calor, medo do pior acontecer, batimento cardíaco acelerado, instabilidade emocional e nervosismo listados como os sintomas mais comuns. A presença de ansiedade foi independente da idade materna, estado civil ou paridade, porém o trimestre gestacional, história de aborto e tempo de internação foram identificados como fatores de risco para ansiedade.
CONCLUSÃO: gestantes com diagnóstico de alto risco internadas no HULW apresentaram ansiedade, identificando-se a necessidade de uma rede de apoio multiprofissional, como o atendimento familiar.
Palavras-chave:
Ansiedade, Hospitalização, Gravidez de alto risco
IntroductionMental Disorders (MD) involve changes in the individual’s behavior, emotion and cognition, with symptoms such as irritability, somatic complaints and feelings of worthlessness.
1 According to the World Health Organization (WHO), about 450 million people suffer from some type of MD, which is responsible for 8.8% of mortality and 16.6% of disability among diseases in low or middle income countries.
2The incidence of MD is higher in women, and one of the predisposing factors is the pregnancy cycle
3. Due to the physical changes of pregnancy and the hormonal action in mood modulation, it is possible to observe a high prevalence of anxiety and depression.
4 In this scenario, symptoms present in the perinatal period range from mild to severe. Previous studies analyzed levels of anxiety and indicated an increase in the possibility of exposing pregnant women to episodes of stress and the presence of psychiatric comorbidities.
5High-risk pregnancy concerns all situations that can intervene in the normal evolution of pregnancy, focusing both on aspects related to both maternal and fetal health, and the psychological profile can be altered, thus causing possible complications that they can be expanded if the pregnant woman is in a hospital.
6Anxiety is defined as a warning sign in the face of an unknown and conflicting threat, in which it indicates an imminent danger, and this prompts the organism to react and enables it for the best response. However, when this hormonal reaction is excessive and disproportionate to the real risk, it changes from physiological anxiety to pathological anxiety.
7Added to the feeling of apprehension, nervousness and tension, anxiety causes physiological responses in the body, such as cardiovascular, endocrine, sensory excitement and variation in the musculoskeletal system.
8 In addition to these visceral and motor effects, anxiety affects thinking, perception and learning, and is a conditioned response to a specific environmental stimulus. The classification of a mother as a high-risk pregnant woman is enough stimulus to trigger the state of anxiety.
9Anxiety and depression during the gestational period are indicative of these same conditions in the puerperium, being associated with unfavorable maternal outcomes, such as the threat of abortion,
10 lower weight and length of the child after birth,
11 shorter duration of exclusive breastfeeding, and it can also cause a delay in child development.
10Under risky conditions, hospitalization may be necessary for the welfare of the mother and fetus, and the insertion in the hospital environment may affect the maternal psychological profile, causing possible complications in the clinical condition of the maternal-fetal binomial; therefore, this study aimed to analyze the level of anxiety in high-risk pregnant women admitted to the maternity hospital of the University Hospital Lauro Wanderley (HULW-UFPB).
MethodsAn observational, descriptive, cross-sectional study of quantitative character, carried out from August 2018 to July 2019, at the Hospital Universitário Lauro Wanderley (HULW), reference service in high-risk pregnancies.
The universe consisted of pregnant women diagnosed with high-risk pregnancies, interned at Hospital Universitário Lauro Wanderley (HULW). The pregnant women were pre-selected in a non-probabilistic manner through convenience sampling, following the inclusion criteria: being pregnant; age over 18 years; high-risk diagnosis; be admitted to HULW. The sample was recruited after collecting information from the patient’s medical records, excluding pregnant women at usual risk and/or using psychoactive drugs. During the period of study, and obeying the inclusion and exclusion criteria of the research, a total sample of 100 pregnant women was obtained.
The invitation to participate in the research took place during the approach of patients admitted to the maternity hospital at HULW, and the confidentiality and autonomy of the research participants were ensured by signing the Free and Informed Consent Form (FICF).
Two instruments were used for data collection: a sociodemographic and clinical form and the Beck Anxiety Inventory (BAI), applied with the translation already validated for Portuguese.
The sociodemographic and clinical questionnaire, self-authored, aimed to identify the pregnant woman concerning her social and clinical conditions with the possibility of drawing a profile of the high-risk pregnant woman interned at HULW. The variables analyzed were: mother’s age, place of birth, marital status, education level, with whom the pregnant woman lives, how many minimum wages are on average in her home and how is the relationship with the child’s father. Regarding the clinical characteristics, the following were analyzed: gestational age, parity, type of pregnancy, number of abortion(s), cesarean section(s) and normal delivery(s), date of collection and hospitalization, if the pregnancy was planned and what is the diagnosis for classification of high risk pregnancies.
The second instrument was the BAI, used to assess the state of anxiety. It consists of 21 items, each with four points that reflect levels of increasing severity of each of the symptoms. Among some of the symptoms evaluated at BAI, the following are observed: heat, tremor in the legs and hands, inability to relax, fear of the worst happening, dizziness, a beating heart faster, emotional instability, terrified or afraid, nervousness and weakness and vulnerability.
12 The classification of the indicative scores for anxiety is: minimal (0-10), mild (11-19), moderate (20-30) and high (31-63).
13The application was carried out by two evaluators, where the evaluator filled out the questionnaires individually according to the response of each pregnant woman. The average time to answer the questionnaires was 20 minutes, in which each step was described to the respondents in a simple way and through a clear and pertinent vocabulary. The collected data were treated statistically in the computer system Statistical Package for the Social Sciences (SPSS), version 25. Questionnaire variables were analyzed using the Mann-Whitney test and compared with each other via the Kruskal-Wallis test. A Spearman Correlation was also performed, to verify the presence and strength of the relationship between the variables and their direction. Statistically, a significant difference was considered when p<0.05 for all tests.
This study was approved by the Research Ethics Committee of the HULW, Federal University of Paraíba (Approval number: CAAE No. 88749518.2.0000.5183), following the ethical criteria established in Resolution 466/12 of the National Research Ethics Commission (CONEP). As this is a documentary research, the risks were restricted to the institution’s documentary heritage, as the data recorded in the patients’ medical records were used. However, some questions could be a source of embarrassment for the interviewee, therefore, in the event of this, the evaluation would be suspended. It is noteworthy that this study is an important instrument for the future planning of actions to prevent and treat anxiety in pregnant women.
ResultsThe sample was characterized by 100 pregnant women, who had a mean age of 27.7 ± 5.78 years, with complete high school (55%), resident of João Pessoa (69%), single with a stable union (50%), multiparous (60%), with gestational age between 37-41 weeks (77%), living with a partner and child(ren) (43%) and with an average family income of one or more minimum wage (56%). In addition, 90% claimed to have a good/great relationship with the child’s father, 58% did not plan their current pregnancy and 78% had between 1 and 7 days of hospitalization.
Regarding the gestational markers and risk factors of the total sample evaluated for the high-risk condition, of which the pregnant woman may have one or more, 29% were classified by clinical history, 26% by obstetric history, 78% of women had diseases in the current pregnancy and 9% due to personal characteristics. Among the 29 pregnant women who had previous diseases, 11 of them had Chronic Systemic Arterial Hypertension (HASC), 6 had Diabetes Mellitus (DM); only 1 participant reported having both HASC and DM. Among 26 women classified as high risk for obstetric history, 25 had a history of abortion. Among the 78 women diagnosed with diseases in the current pregnancy, Gestational Systemic Arterial Hypertension (HASG) was present in 15, Gestational Diabetes Mellitus (GDM) in 23, and the presence of the two associated clinical conditions in 10 of them.
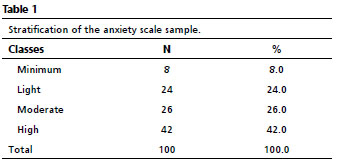
From the analysis of the anxiety profile by BAI, the results described in Table 1 were obtained. The average of the total score is 25.92 ± 11.6, so that 68% of the pregnant women presented an anxiety picture, in which 42% was high and 26% was moderate.
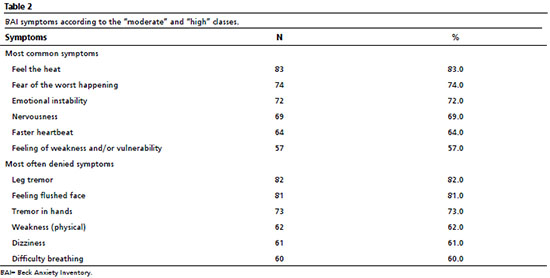
Among the symptoms of BAI, those that had a higher frequency and that was reported by pregnant women who felt them “sometimes” or “always” are shown in Table 2. The variables “feeling the heat” and “fear of the worst happen” were observed, respectively, in 83% and 74% of the sample. In this same table, the results of less frequent symptoms in BAI are observed, marked as “never” or “rarely” by pregnant women. Among these, the symptoms are “trembling in the legs” (82%), “feeling a flushed face” (81%) and “trembling in the hands” (73%).
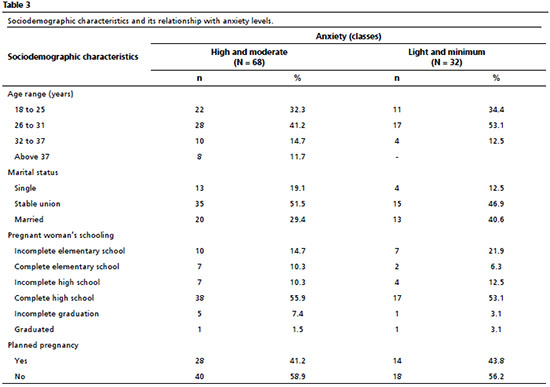
To obtain an assessment of the level of anxiety and the relationship with different social conditions of the pregnant women, a crossover was carried out between the sociodemographic and BAI questionnaires, the results of which are shown in Table 3. From this relationship, it was noted that in all women over 37 years old the level of anxiety was moderate to high, and 53.1% classified with the lowest level of anxiety (mild and minimal) were women between 26 and 31 years old. The level of anxiety classified as moderate to high was prevalent in the entire sample regardless of marital status. In the education variable, the anxious state was prevalent at all levels (Table 3), as in pregnancy planning. Regarding family support, of the pregnant women classified as having moderate to high anxiety, 90% (9) stated having a bad relationship with the child’s father, 63.6% (28) declared having one or less of a minimum wage and 71,4% had an income above two minimum wages.
In women classified as high-risk pregnant women based on their personal characteristics, all showed moderate to high anxiety. Among those with clinical and obstetric history, the distribution was similar between anxiety levels, differently from those classified due to a current pregnancy disease, in which the moderate and high anxiety levels predominated.
Regarding parity, 61.8% that were in the moderate to high BAI classification are multiparous (Table 4). When observing the items in the BAI questionnaire, it is clear that the most discordant symptom is the heart beating faster, in which 58.3% (35) of the multiparous women claim to have it, compared to 72.5% (29) of the nulliparous women. The other most frequent symptoms are similar in both groups, such as fear of the worst happening with 77.5% (31) of nulliparous women and 71.6% (43) of multiparous women, and nervousness, with 65% (26) of nulliparous women and 71.6% (43) of the multiparous women.
In the present study, one in four women reported having had one or more abortions (25), and 56% (14) of these were classified as having an anxiety index between moderate to high levels according to the BAI. Besides, 58.8% (10) of those who had only one episode said they were afraid of the worst to happen, followed by 100% (8) of those who had more than one episode.
When analyzing the gestational trimester variable, the highest level of anxiety was among pregnant women in the third trimester. It is also observed that 72.7% (56) of the women who are in the last trimester identified themselves as nervous, 75.3% (58) were afraid of the worst to happen and 72.7% (56) had emotional instability. Regarding the length of hospital stay, 81% of pregnant women evaluated by the survey spent between 1 and 7 days hospitalized at HULW, restricted or not to bed, depending on the condition of the individual clinical picture.
Considering the BAI classes and characterizing them in a dichotomous variable about anxiety (minimal and mild, moderate and high), the Mann-Whitney test was used to compare also with the other variables related to the pregnant woman, and an association with the variables gestational trimester (U = 781.50;
p<0.05), number of days of hospitalization (U = 781.00;
p<0.05) and classification of high risk by personal characteristics (U = 944.00;
p<0.05), but showed no association with marital status (U = 938.50;
p<0.05) and number of abortions (U = 966.00;
p<0.05).
The total BAI score and its categorization into four classes were compared with the other sociodemographic variables, using the Kruskal-Wallis test, to verify the statistical difference in at least one of the groups, and the same was applied to the variable “fear the worst happen”.
The variables that showed a statistical difference concerning the total BAI score were gestational trimester and number of days of hospitalization, while the variables parity and maternal age did not have a significant p-value (Table 5). When comparing the sociodemographic and clinical questionnaire with the “fear of the worst happening”, it’s noticed the statistical significance in the marital status, family income and relationship with the child’s father.
Through Spearman’s Correlation it was possible to observe that there are weak correlations and inverse relationships between the variables of the present study. Among these, there is an association between the total BAI score divided by classes and the variables: gestational trimester (ρ=0.262;
p<0.05), days of hospitalization (ρ= - 0.291;
p<0.05), classification high risk due to personal characteristics (ρ = - 0.247;
p<0.05) and diseases in the current pregnancy (ρ= - 0.225;
p<0.05).
The “fear of worse happening” was correlated with the pregnant woman’s marital status (ρ = - 0.216;
p<0.05), relationship with the child’s father (ρ= - 0.208;
p<0.05), family income (ρ= 0.218;
p<0.05) and pregnancy planning (ρ = - 0.224;
p<0.05), in addition to the gestational trimester (ρ=0.206;
p<0.05) and days of hospitalization (ρ= - 0.344;
p<0.05).
DiscussionIn general, the results obtained clearly show that all women in high-risk pregnancies presented levels of anxiety in all age groups, regardless of education, marital status, parity and their clinical/obstetric conditions.
According to Kliemann
et al.,
14 pregnancy is recognized as a risk factor for the development and worsening of mental health problems and this psychological condition is more common in pregnancy than in postpartum. The pregnancy-puerperal period is considered a phase of greater subjection for the development of depression and anxiety due to the changes in hormonal, physical and emotional levels experienced by them.
15From the BAI analysis, in all the pregnant women evaluated there was some level of anxiety, and the classification from a moderate to high level was predominant. Among the symptoms evaluated by BAI, one of those that were most present was the fear of something bad happening, which is expected as a result, as the possibility that feelings of vulnerability occur comes to light due to the high risk pregnancy and, thus, therefore, they are more exposed to stressful feelings.
16Three situations can influence the emergence of anxiety during high-risk pregnancy, they are: concern about the course of the current pregnancy, the very high-risk condition and also factors associated with hospitalization. Such factors can also have repercussions on the clinical condition of the pregnant woman, such as a higher rate of prematurity, abortion, low birth weight, pre-eclampsia, postpartum depression and delay in the child’s neuropsychomotor development.
17 In the current study, it was possible to observe that situations such as diseases in the current pregnancy (HASG and DMG) can influence the prevalence of an anxious condition.
The concern with the course of the pregnancy and the complications that may exist for her or the fetus, added to the hospitalization, only increases the negative thoughts about the course of the pregnancy, making her vulnerable to feelings of anguish, fear and anxiety about the end of the pregnancy treatment that keeps her intern, due to the delivery and the arrival of the baby.
18 According to Saviani-Zeoti and Petean,
19 it is likely that the fact that they are exposed to an uncertain situation, such as changes in their own health or in the child’s health, can lead to consequences over which they are not always in control, and this will end cause an increase in these indexes.
Regarding the number of days of hospitalization, it was visible in the current study that anxiety decreased over time, since the woman was absorbing her risk condition, adapting to the service, the hospital environment and the responsible health team, which can directly impact the feeling of welcoming and humanization provided to the pregnant woman. Humanized assistance encompasses the provision of care, respect for the cultural and social aspects of women,
20 but care also includes that women have knowledge about what changes are happening in their own health and/or in child’s health and possibly reduce anxiety.
In this perspective, the role of prevention in mental health is of fundamental importance, being carried out within the gestational period through the Psychological Prenatal (PNP), concomitant with the Gynecological Prenatal, in which themes such as the emotional and psychosomatic repercussions of the pregnancy and the puerperium.
21 In a study by Almeida and Arrais,
22 it was found that the PNP exerts some protection during the gestational period, serving as a space for women to vent, where they can find emotional support and qualified listening.
The level of anxiety in the studied sample was dependent on age and parity. Women of reproductive age, with a high maternal age and multiparous women presented high levels of anxiety, when it would be expected that due to the experience with motherhood these rates would be lower. However, according to Arrais et al.,
21 anxiety disorders are very common in women of reproductive age, showing that one in four pregnant women suffer from MD, and 48% of them express anxiety.
These MDs showed no statistical difference between women with recurrent abortions in the study by Carvalho Júnior et al.,
23 a result different from that observed in the sample studied, where the prevalence of anxiety increased according to the number of abortions and the fear intensified with the occurrence more episodes. This can be justified by the psychological impact on the woman, even more on those who have a yearning for motherhood, and after the pregnant woman’s perception of the risk for herself and her baby, and the possible results of this complication, her instinct is inevitable maternal development will increase levels of uncertainty, psychological distress and reduced well-being.
24 To alleviate this situation, it is necessary to go beyond biological care, and see this woman as a person inserted in an existential context that needs physical and mainly mental support.
10In addition to these variables evaluated, pregnancy planning did not occur in more than half of the sample, an essential fact also observed in the study by Shiavo et al.,
10 and this may be due to the deficit in care infrastructure, causing the lack of information about contraception and the partner’s rejection for seeking pregnancy planning services. Such a condition is a factor that can influence the emergence of anxiety,
14 however this influence was not observed in the current study since anxiety was predominant regardless of the presence or absence of family planning; in addition, the family planning variable showed a correlation with the pregnant woman’s fear that the worst could happen.
Although anxiety is prevalent throughout the course of pregnancy, the level of anxiety presented itself differently throughout the gestational trimesters, in which it progressed gradually over the quarters. It is known that in the first trimester, there is a great concern in relation to fetal development and well-being, leading it to be overly concerned with its life habits
25; in the second trimester, with the beginning of the perception of fetal movements, feelings of personification of the baby emerge and in the third trimester, the level of anxiety tends to increase even more due to the proximity of delivery and the probable change in the life routine after delivery.
25The analysis of social variables with anxiety shows that there is a correlation between marital status, relationship with the child’s father and family planning with the variable fear of the worst happening. The pregnancy process itself is already considered a moment of vulnerability,
24 and its insertion in an emotionally unfavorable environment can be a predictor of the occurrence of anxiety.
14 The present study shows that a bad relationship with the child’s father causes a difference in the frequency of the feeling of fear that the worst happens, further emphasizing the need for emotional support to provoke feelings of understanding, care and security in the pregnant woman,
26 since family support is essential for women’s biopsychosocial well-being.
27In addition, in the hospital environment, the joint work of professionals from different areas is present, constituting the multidisciplinary work, which is extremely positive during the gestational period, since the broad assistance and qualified listening can help to increase the pregnant woman’s reliability, as well as its adaptation to the inpatient sector and, consequently, decrease its propensity to develop TMs.
22It is necessary to emphasize that despite the evidences of this study, it still has limitations such as the deficit of comparison between low-risk pregnant women or even high-risk mothers, to compare the data obtained and prove the anxiety in the sample proposed by the study. In addition, it would be relevant to assess the history of previous MT and/or anxiety diagnoses in this sample for comparison with the gestational period.
This study demonstrates the prevalence of moderate to high anxiety among high-risk pregnant women interned at HULW, in which some risk factors for this circumstance were noted, such as maternal age, gestational trimester, abortion history and length of hospital stay; and factors that were independent of anxiety, such as education, marital status and parity. The “fear of the worst happening” was a variable that was evident among the symptoms of BAI, given its correlation with sociodemographic conditions such as relationship with the child’s father and pregnancy planning. It is necessary to emphasize the importance of producing more studies in this area in order to ratify the prevalence of anxiety in high-risk pregnancies, particularly at the tertiary level of health care, since hospitalization is a predisposing factor to the existence of anxiety.
References1. Souza e Souza L, Barbosa B, Oliveira e Silva C, Souza A, Ferreira T, Siqueira L. Prevalência de transtornos mentais comuns em adultos no contexto da Atenção Primária à Saúde. Rev Portuguesa Enf Saúde Mental. 2017; 18: 59-66.
2. World Health Organization (WHO). People with mental disabilities cannot be forgotten. Geneva: WHO Press; 2010. [access in 2020 Nov 1]. Available from:
https://www.who.int/news/item/11-12-2010-people-with-mental-disabilities-cannot-be-forgotten3. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014 Abr; 43 (2): 476-93.
4. Lopes RS, Lucchese R, Souza LMM, Silva GC, Vera I, Mendonça RS. O período gestacional e transtornos mentais: evidências epidemiológicas. Hum Tecnol (FINOM). 2020; 19 (1): 35-54.
5. Silva MMJ, Nogueira DA, Clapis MJ, Leite EPRC. Anxiety in pregnancy: prevalence and associated factors. Rev Esc Enferm USP. 2017; 51: e03253.
6. Azevedo CCS, Hirdes A, Vivian AG. Repercussões emocionais no contexto da gestação de alto risco. Int J Dev Res. 2020; 10 (9): 40216-20.
7. Sadock BJ, Sadock VA, Ruiz P. Compêndio de Psiquiatria: ciência do comportamento e psiquiatria clínica. 11
th ed. Porto Alegre: Artmed; 2017. [access in 2020 Nov 1]. Available from:
https://oitavaturmadepsicofm.files.wordpress.com/2019/03/compecc82ndio-de-psiquiatria-kaplan-e-sadock-2017.pdf 8. Vidor LP. Associação da ansiedade com inibição intracortical e modulação descendente da dor na síndrome dolorosa miofascial [Tese]. Porto Alegre (RS): Faculdade de Medicina da Universidade Federal do Rio Grande do Sul; 2014.
9. Cunha MMH. As perturbações de ansiedade e a síndrome de hipermobilidade articular [Dissertação] Lisboa, Portugal: Faculdade de Medicina da Universidade de Lisboa; 2016.
10. Schiavo RDA, Rodrigues OMPR, Perosa GB. Variables Associated with Gestational Anxiety in Primigravidas and Multigravidas. Trends Psychol. 2018; 26 (4): 2105-118.
11. Pinto TM, Caldas F, Nogueira-Silva C, Figueiredo B. Maternal depression and anxiety and fetal-neonatal growth. J Pediatr (Rio J). 2017; 93 (5): 452-9.
12. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 Dez; 56 (6): 893-7.
13. Cunha JA. Manual da versão em português das Escalas Beck. São Paulo: Casa do Psicólogo; 2001.
14. Kliemann A, Boing E, Crepaldi MA. Fatores de risco para ansiedade e depressão na gestação: Revisão sistemática de artigos empíricos. Mudanças: Psicol Saúde. 2017; 25 (2): 69-76.
15. Borges ARF, Rocha AHG, Simões AO, Vitorino FO, Fernandes KB,Tavares RF, et al. Alterações dos hormônios cortisol, progesterona, estrogênio, glicocorticóides e hormônio liberador de corticotrofina na depressão pós-parto. Rev Ciênc Estud Academ Med. 2021; (14): 27-45.
16. Paz MMS, Diniz RMC, Almeida MO, Cabral NO, Mendes CKTT, Araújo JSS, et al. Ansiedade na gestação de alto risco: um reflexo da atenção básica no alto sertão da Paraíba. Rev Neurociênc. 2020; 28: 1–21.
17. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Atenção ao pré-natal de baixo risco. Brasília (DF): Ministério da Saúde; 2012. [access in 2020 Nov 1]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/cadernos_atencao_basica_32_prenatal.pdf18. Piveta V, Bernardy CCF, Sodré TM. Perception of pregnancy risk by a group of pregnant women hypertensive hospitalized. Ciênc Cuid Saúde. 2016; 15 (1): 61-8.
19. Saviani-Zeoti F, Petean EBL. Apego materno-fetal, ansiedade e depressão em gestantes com gravidez normal e de risco: estudo comparativo. Estud Psicol (Campinas). 2015; 32 (4): 675-83.
20. Vieira VCL, Barreto MS, Marquete VF, Souza RR, Fischer MMJB, Marcon SS. Vulnerabilidade da gravidez de alto risco na percepção de gestantes e familiares. Rev Rene. 2020. 20 (1): e40207.
21. Arrais AR, Araujo TCCF, Schiavo RA. Depressão e Ansiedade Gestacionais Relacionadas à Depressão Pós-Parto e o Papel Preventivo do Pré-Natal Psicológico. Rev Psicol Saúde. 2019; 11 (2): 23-34.
22. Almeida NMC, Arrais AR. O pré-natal psicológico como programa de prevenção à depressão pós-parto. Psicol Ciênc Prof. 2016; 36 (4): 847-63.
23. Carvalho Júnior A. Qualidade de vida, ansiedade e depressão em mulheres com aborto espontâneo recorrente [Tese] Campinas (SP): Faculdade de Ciências Médicas da Universidade Estadual de Campinas; 2019.
24. Barros AC. Ansiedade, traço e estado, risco para depressão e ideação suicida em gestantes de alto risco em Alagoas [Dissertação]. Maceió (AL): Universidade Federal de Alagoas; 2020.
25. Santos JCPCA. Ansiedade face à morte em idosos: Influência de variáveis sócio-demográficas e do bem-estar subjectivo [Tese]. Lisboa, Portugal: Instituto Superior de Psicologia Aplicada; 2005.
26. Soncini NCV, Oliveira CM, Viviani JC, Gorayeb R. Aspectos psicossociais em mulheres brasileiras com gestações de alto e baixo risco. Psicol Saúde Doenças. 2019; 20 (1): 122-36.
27. Costa DO, Souza FIS, Pedroso GC, Strufaldi MWL. Transtornos mentais na gravidez e condições do recém-nascido: estudo longitudinal com gestantes assistidas na atenção básica. Ciênc Saúde Colet. 2018; 23 (3): 691-700.
Received on February 23, 2021
Final version presented on October 8, 2021
Approved on July 8, 2022
Author’s contribution: Paz MMS, Diniz RMC and Assis TJCF designed the study and carried out the experiment. Paz MMS, Diniz RMC, Assis TJCF, Almeida MO, Cabral NO, Pontes VA, Borges NMS and Mendes CKTT wrote the manuscript. Paz MMS, Diniz RMC and Sena MF processed the data.
All authors approved the final version of the article and declare no conflicts of the interest.
 ; Raquel de Moura Campos Diniz2
; Raquel de Moura Campos Diniz2 ; Milene de Oliveira Almeida3
; Milene de Oliveira Almeida3 ; Nadine Oliveira Cabral4
; Nadine Oliveira Cabral4 ; Thais Josy Castro Freire de Assis5
; Thais Josy Castro Freire de Assis5 ; Milleny Fernandes de Sena6
; Milleny Fernandes de Sena6 ; Viviann Alves de Pontes7
; Viviann Alves de Pontes7 ; Natália Mota da Silva Borges8
; Natália Mota da Silva Borges8 ; Cristina Katya Torres Teixeira Mendes9
; Cristina Katya Torres Teixeira Mendes9