ABSTRACT
OBJECTIVES: measuring the prevalence of interventions and/or complications based on the Maternity Safety Thermometer (MST) criteria and verifying associations with sociodemographic, clinical, and obstetric factors.
METHODS: prospective observational study conducted with postpartum women admitted to the maternity ward of a tertiary hospital, from October 10th to December 30th, 2020. Data were collected from medical records and self-administered questionnaires from 260 patients.
RESULTS: harm-free care was detected in 17.7% of participants, 66.9% had low-temperature damage (one or less intervention/complication) and 33.1% of patients had elevated temperature damage (two or more intervention/complication). The most frequent intervention was the “scar”, given that 38.5% had abdominal scarring (cesarean section) and 26.5% had perineal scarring (2nd-degree tear or greater – spontaneous or by episiotomy). The second most frequent MST item was related to the perception of safety (30%), followed by complications to the newborn (12.3%), infection (11.2%), and hemorrhage (9.2%). Factors related to high temperature were: being of social class A or B, having a previous cesarean section, and being hospitalized during pregnancy.
CONCLUSIONS: one-third of the participating women had two or more complications/interventions (high temperature by the MST), factors that are related to this temperature were: being of social class A or B, having a previous cesarean section, and being hospitalized during pregnancy.
Keywords:
Postpartum, COVID-19, Patient safety
RESUMO
OBJETIVOS: mensurar a prevalência de intervenções e/ou complicações a partir dos critérios estabelecidos pelo Termômetro de Segurança da Maternidade (TSM) e avaliar associações com fatores sociodemográficos, clínicos e obstétricos.
MÉTODOS: estudo observacional prospectivo realizado com puérperas internadas na maternidade de hospital terciário, de 10 de outubro a 30 de dezembro de 2020. Foram coletados dados do prontuário e de questionários autoaplicáveis de 260 pacientes.
RESULTADOS: um cuidado livre de intervenções/complicações foi detectado em 17,7% das participantes, 66,9% apresentaram baixa temperatura (até uma intervenção/complicação) e 33,1% tiveram alta temperatura de intervenções/complicações (2 ou mais). A intervenção mais frequente foi a denominada “cicatriz”, sendo que 38,5% tiveram cicatriz abdominal (cesariana) e 26,5% tiveram “cicatriz” perineal (laceração de 2º grau ou mais – espontânea ou por episiotomia). O segundo dano mais frequente foi o relacionado à percepção de segurança (30%), seguido de complicações do recém-nascido (12,3%), infecção (11,2%), e hemorragia (9,2%). Houve associação de ter alta temperatura com ser de classe social A ou B, ter cesárea anterior e ser internada na gestação.
CONCLUSÕES: das mulheres participantes, um terço teve duas ou mais complicações/intervenções (alta temperatura no TSM), estiveram relacionados a essa temperatura: ser de classe social A ou B, ter cesárea anterior e ser internada ao longo da gestação.
Palavras-chave:
Período pós-parto, COVID-19, Segurança do paciente
IntroductionThe assistance to labor has been through several modifications in the last decades. There was an increase in the use of various practices in order to regulate and monitor a physiological process.
1 The main objective of these practices would be to improve perinatal results. However, there are such interventions that, when performed without clinical indication, negatively compromise the experience of childbirth by women,
1 and lead to worse maternal-fetal outcomes.
2It is a challenge to assess how many and what interventions are performed, as well as assessing complications, since most studies are focused in a single intervention, for example, cesarean delivery rates,
3 in a complication, for example hemorrhage
4 or infection
5 or in severe maternal morbidity or near miss.
6 It is necessary to adopt instruments that allow the assessment of interventions and complications simultaneously, since these events are related to each other, that is, more interventions increase the number of complications, but also pregnant women with more complications usually need more interventions.
The Maternity Safety Thermometer (MST) is an assessment tool proposed in England that monitors “temperature of complications/interventions” of groups of patients, services or region.
7-9 This instrument is part of a program created in 2010, denominated Quality, Innovation, Productivity and Prevention National Program (QIPP), that aims to improve health assistance and reduction of costs.
10 This initiative was created due to data reporting that approximately 10% of England population has experienced some lesion provoked by health assistance, generating adverse effects in regard to physical, mental and social wellbeing.
8,10The MST was already translated and validated in Portuguese.
9 Topics that were measured with the tool include perineal trauma (episiotomy or spontaneous trauma) and abdominal (cesarean or laparotomy), postpartum hemorrhage, maternal infection, baby’s health (Apgar score below 7 at the fifth minute and admission in Neonatal Unit) and perception of safety by women.
9 “High temperature” obstetric assistance occurs when women and neonates are submitted to more interventions and/or suffer more complications, compared to an assistance with “low temperature”, in which these events occur less oftenly.
8,9 The tool allows to compare these temperatures over time and in diverse institutions and to identify characteristics of patients that are prone to have complications or interventions. The thermometer, nonetheless, does not assess the indication of each measured intervention, nor if the presented complication was preventable or not, it only assesses the prevalence of items analyzed.
8,9The COVID-19 pandemic brought new challenges to health assistance in general, also to assistance to pregnant and puerperal women. For instance, there were modifications in functioning of places of care, difficulties in the access to healthcare system, including at prenatal period, decrease of the number of available health professionals in obstetric assistance, due to reallocation of workforce to act directly in pandemic and dismissals, scarcity of funding, materials, beds in hospitals and ICUs.
11-13 Furthermore, infection by COVID-19 itself had a significant impact on maternal health, increasing maternal mortality and the need for hospitalization of pregnant and puerperal women in ICUs.
14 However, the impact of pandemic on childbirth assistance, particularly in non-infected women, still was not studied.
Knowing the intervention and/or complication rates in diverse topics proposed by the MST and characteristics of women subject to a higher amount of damage and interventions may help to plan specific health policies in order to modify indicators.
8 It is also necessary to establish the frequency of these interventions/complications in the obstetric population non-infected by COVID-19, attended in pandemic period. This study aimed to assess obstetric interventions and complications of a Teaching Hospital in the South of Brazil using the Maternity Safe Thermometer, during COVID-19 pandemic in non-infected women.
MethodsProspective observational study conducted with puerperal women hospitalized in Polydoro Ernanide São Thiago Teaching Hospital of the Federal University of Santa Catarina (HU-UFSC – Portuguese acronym). It is a tertiary reference hospital, attached to EBSERH network and that attends exclusively for the Unified Health System. The hospital was not a reference center for COVID-19 cases. Data were collected from October 10, 2020 to December 30, 2020 (COVID-19 pandemic in force and no available vaccines at the time).
Were considered as eligible for the study: puerperal women that had their children in HU with concepts weighing >500g and/or gestational age >22 weeks, hospitalized in the rooming-in nursery or gynecological nursery. Women with severe mental illness, who gave birth outside the facility or refused to participate in the study were excluded.
For the sample calculation, an approach of population parameter estimate was adopted, with CI95%, margin of error of 5% and an expected proportion in the harm-free population of 18.6%,
9 and a necessary sample of 233 women was calculated. In order to assure higher safety, in case of exclusion of participants, inconsistency and/or non-fill of variables, we opted to include every woman that met the inclusion criteria at the data collection period.
After selection by inclusion and exclusion criteria, reading and signing of free and informed consent form, a questionnaire built for the research was sent to be fulfilled, and it was pre-tested with a sample similar to that of the study population. The questionnaire had open-ended and multiple-choice questions for answer. The questionnaire was applied at the time the patient had hospital discharge and was in Portuguese in case of being fluent in this language, or within the tool, translated into English, Spanish or French for patients that were non-speakers of Portuguese.
Data were collected from this self-made questionnaire and from data from medical records, collected by researchers during the hospitalization of pregnant women. Collected data were typed into an Excel 2007 software spreadsheet, using double validation of data from medical records in order to reduce the possibility of errors. Data were checked for inconsistencies and variables without fulfillment were excluded from the analysis. If the questionnaire or the spreadsheet had more than 50% of variables non-filled, the case would be excluded from the analysis.
In the questionnaire, were collected the variables: age, skin color, nationality, schooling, socioeconomical status, (from “Brazil criterion” from Brazilian Association of Research Enterprises – ABEP
15 – Portuguese acronym), marital status, work situation, if had COVID-19 during pregnancy, obstetric and personal/clinical history, information on prenatal (adequacy assessed according to Kessner index
16), use of antibiotics after vaginal or cesarean delivery and opinions of the puerperal woman about labor, delivery and postpartum, including questions necessary to the “perception of safety” criterion of the thermometer, described below. Other variables were collected from the medical record, being: obstetric history (previous vaginal and cesarean deliveries), data on prenatal, hospitalizations during pregnancy and present complications (clinical or obstetric), body mass index (posteriorly classified as normal or overweight/obesity), data from assistance to current delivery (presence of labor induction and variables related to maternity safe thermometer, described below).
The maternity safe thermometer, originally written in English, uses the word “Harm” to define both intervention and complication. In this research, we used the words “
intervenção” and “
complicação” (intervention and complication), for the word
“Dano” (Harm) may lead to a misunderstanding, in Portuguese language, of a bad assistance practice or a malicious intervention by the assistant professional. The criteria used by the instrument to “measure temperature” are, hemorrhage, infection, trauma (abdominal or perineal), complications with the newborn and negative perception of safety in delivery and postpartum.
For the complication “hemorrhage” were considered women who used the protocol of postpartum hemorrhage (use of oxytocin beyond prophylactics, methylergometrine, misoprostol and hemoderivatives) or had description of hemorrhage intra or postpartum – datum collected in the medical record.
For the complication “infection” were considered women that mentioned having used antibiotics after delivery and/or those who had any infection described in the medical record.
For the complication related to the neonate were considered women that had stillbirths and/or neonates with Apgar below 7 at the fifth minute and/or baby referred to NICU (data collected in the medical record).
For the complication related to “perception of safety”, were considered women who answered “yes” to any of the proposed questions on this subject in the adopted tool
9: “Were you alone at any time in which you felt worried in labor” and/or “Were you alone at any time in which you felt worried after delivery?” and/or answered “no” to “The assistance team dealt seriously any concern that you had mentioned during labor?” and/or “The assistance team dealt seriously any concern that you had mentioned after delivery?”
For the variable “scar”, data were collected from the medical record and were considered women that underwent cesarean section or postpartum laparotomy (abdominal trauma). The variable “perineal trauma” has different interpretations – whilst Melo
9 considers perineal injury only severe lacerations – 3
rd and 4
th degree, Salgado
et al.
7 considers those who had episiotomy or any perineal laceration regardless of de need for suture. Assuming that the thermometer was developed for measuring lacerations and complications, considering only severe lacerations or considering every perineal laceration would avoid the study of relevance of episiotomies.
Initially, the prevalence of each intervention and/or complication was calculated, and the proportion of women who had each temperature proposed by the thermometer – from zero to five. For this assessment, perineal injury was calculated in three different manners – considering any laceration or suture (spontaneous or episiotomy), considering only 2
nd degree lacerations or more (spontaneous or episiotomy) and considering only severe lacerations.
Posteriorly, it was conducted an association analysis between having “high temperature” of interventions/complications and the sociodemographical, clinical, obstetric and assistance variables. For these analyses, was considered as perineal injury any laceration of 2º degree or more – spontaneous or performed by the health professional.
For association analysis, was considered as dependent variable “high temperature” of complications/interventions (2 or more). The dependent variables were: maternal age, ethnicity, nationality, schooling, economical status, living with partner, working during gestation, had COVID-19 during gestation, adequate prenatal, previous vaginal delivery, previous cesarean delivery, overweight/obesity, hypertensive syndrome, labor induction, hospitalization during pregnancy.
Finally, for a better comprehension of characteristics that turned out to be related to “high temperature”, the association of these characteristics with each complication or harm from the safety thermometer was analyzed.
Data were analyzed by means of statistical pack IBM SPSS, version 27. All variables were analyzed by means of descriptive statistics (absolute and relative frequency, median and standard deviation). In order to evaluate the relationship between diverse categories of intervention and/or complication and association of characteristics that showed significance in the logistic regression model as “high temperature”, the chi-square test was performed, and when applicable, Fisher’s exact test. To assess the association between sociodemographical, clinical and obstetric variables with the presence of “high temperature” the odds ratio was calculated. For binary logistic regression analysis, all variables with
p<0.10 were considered. For all analyzes, a 5% significance level was adopted.
The study is part of the research “Obstetric and puerperal complications during COVID-19 pandemic’, under number 5543120.7.0000.0121, approved by the Research Ethics Committee of UFSC (Portuguese acronym for Federal University of Santa Catarina).
ResultsBetween October 10 and December 30 2020, 351 women that had their children in HU-UFSC were eligible to participate in the research. Of these, 91 did not participate: 53 did not want to fill the questionnaire and 38 agreed, but did not answer the questionnaire for many reasons (involved with baby care, multidisciplinary consultations or did not have time before hospital discharge). Therefore, the number of analyzed cases was 260.
The mean age of study population was 28.6 years (SD 6.4). The mean gestational age was 38.57 weeks (SD 2.36). The sample demonstrated a high percentage of women with some obstetric risk and 10% of women were hospitalized during gestation (hospitalizations that had birth as outcome were excluded) (Table 1).
Of women who had vaginal delivery, 16.3% had intact perineum. Those who had spontaneous lacerations were: 40.6% of 1º degree; 39.4% of 2º degree; 1.3% of women had 3º degree laceration; there were no 4º degree laceration in this sample. Episiotomy was performed in 4 (2.5%) women, none of them had severe laceration. No woman that underwent cesarean section had perineal complication and no women with perineal complication underwent laparotomy after delivery.
Table 2 shows that the number of women with “high temperature” varies according to the considered perineal injury. When considering any perineal laceration, it was detected that 43.5% of patients had 2 or more interventions/complications, while 56.5% of women had one complication/intervention or didn’t have any, which is considered “low temperature”, when 5% of women had harm-free care. When considering only 2º degree lacerations (spontaneous or episiotomy), 33.1% had “high temperature”, 66.9% had “low temperature” and, of the latter, 17.7% had care free of complications or interventions. Considering perineal injury, only in women that had severe laceration, the percentages are 26.1% and 76.8%, respectively, with 34.2% of care free of complications or interventions.
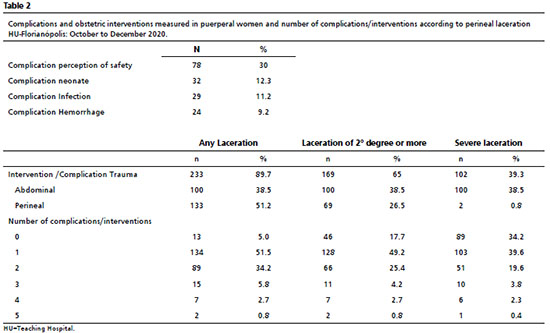
The most frequent complication was the scar complication, followed by harm in relation to the perception of safety, infection complication, neonate complication and those related to hemorrhage (Table 2). Among neonates, 29 (10.9%) were preterm.
Having a higher social status, previous cesarean section and being hospitalized during pregnancy were variables associated with “high temperature” of complications or interventions that showed significance in the adjusted model. That did not occur in primiparous, variable that did not maintain significant association with “high temperature” in the adjusted analysis, as well as age older than 35 years and presence of hypertensive disorder. The model showed good adjustment by Hosmer-Lemeshow test = 0.94 (Table 3).
The other variables analyzed: being younger than 19 years or older than 35 years; being black, brown or indigenous; being foreign; having completed high school; having had COVID-19 during pregnancy; having already gave birth; having adequate prenatal; having overweight or obesity or have been submitted to labor induction did not influence the outcome (Table 3).
In order to have a better comprehension about the factors related to “higher temperature” between women of higher social status, those who had cesarean delivery and those hospitalized during pregnancy, each of these variables were analyzed according to complications/interventions of the safety thermometer. Being of social class A/B was associated with complication “perception of safety”. Having cesarean delivery history and being hospitalized during pregnancy were associated with abdominal scar (cesarean repetition) and neonate complication. (Table 4).
Five twin pregnancies occurred in the sample. Of these, four had cesarean delivery as outcome and one woman had vaginal delivery with 2
nd degree laceration. Three had hemorrhage as complication (
p=0.006 Fisher’s exact test) and the same three women had neonate complication (
p=0.01), one had infection complication and two had perception harm (non-listed data).
DiscussionIn this study, 260 puerperal women were assessed with the maternity safety thermometer, which is a tool that allows measuring the temperature of interventions and/or complications. We highlight that the tool does not assess the necessity or indication of interventions (cesarean section and episiotomy) or the avoidability of complications (spontaneous perineal lacerations, neonate complications, hemorrhage, infections and harm related to perception of safety),
8,9 only their prevalence.
The studied sample showed care without any intervention/complication in 34.2% of cases, if perineal injury is considered only for severe lacerations. A similar study using the tool, conducted in Rio Grande do Norte, verified a prevalence of 18.6% of patients with assistance free of complications
9 and data from NHS England show assistance free of complications in circa 70% of analyzed binomials.
9 If the complication/intervention of perineal injury considers only lacerations of 2º degree or more, the percentage of women with harm-free care decreases to circa 18%. In addition, if it is considered any perineal injury (that is, including 1
st degree lacerations in perineal injury), the number of women without any complication/intervention drops to 5%. A low percentage, but higher than that shown with Brazilian data from 2012, when assistance without interventions occurred in 2% of the population.
7In this study, as well as other studies using the tool, the “scar” complication was the most prevalent. This complication considers the presence of abdominal scar (cesarean section or postpartum laparotomy) or perineal scar.
7-9 In this study, the prevalence of this item of the tool was 39.3% (considering only severe lacerations), 65% (considering severe lacerations and those of 2º degree) and 89.7% (considering any perineal laceration). In other Brazilian studies, the prevalence of “scar” complication was 77%
9 and 90%.
7Cesarean section rate in this sample was 38.4%, lower than the general cesarean rate in Brazil, which reached 56.3% in 2019. The cesarean rate registered in the hospital in the period of study is similar to that of 2019 in the same period,
17 demonstrating that the impacts of pandemic in the health system did not modify cesarean rates in the hospital studied.
In relation to perineal complication, the institution studied has a policy of restriction of episiotomies, following WHO guidelines and scientific evidence.
1,18 However, 2.5% of women were submitted to this procedure, a lower rate than that found in other institutions
9 and in the research Birth in Brazil, in which a 53.5% rate was reported.
2 In the service, the episiotomy rate was similar to the period of 2014 to 2018 (2.7%), showing that there was not modifications of protocol or care with pandemic. As demonstrated in a systematic review, the use of a policy restrictive to episiotomy did not increase the number of severe lacerations.
18The second most prevalent harm was the maternal perception of safety (30%). This is the only harm that uses women’s subjective perception about the care provided. The tool has specific questions about feeling alone and not having concerns taken into consideration.
7,9 The value was similar to that found in one of the hospitals studied by Melo,
9 but lower than the other described hospitals. Other possible manners of satisfaction or dissatisfaction with the experience were not measured. It is necessary to consider that the period of data collection of the current study was during COVID-19 pandemic, when a restriction for companions of puerperal women in the rooming-inoccurred, which may have influenced this perception.
Data related to neonate complication had prevalence of 12.3%, being preterm 10.8% of neonate. The item related to baby’s health presented lower prevalence than that found in Northeast (21.4%),
9 but higher than that described in Southeast (7.7), however, in the latter, only full term neonates. Data related to preterm birth are similar to those found in this study, the preterm birth rate is estimated at 10.6% and in Brazil, 11.2%.
19The infection complication was present in 11.2% of the sample. The value is discrepant to other studies, since in the studied hospitals in Northeast region the prevalence was 22.2%
9 and data from Southeast region showed a prevalence of 2.2%.
7To this moment, there is no absolute prevalence of puerperal infection in the entire Brazil, but isolated studies of several institutions. These data point puerperal infection rates of 2.2% to 7.5%, depending on characteristics of the study population,
20 and it should be considered that there is a trend of underreporting.
5 Current data can also be underestimated, mainly due to the lack of registration of professionals in the medical records, besides, the patients receive hospital discharge up to two days after birth, and most infections arise after this period. It may occur that patients do not return to the hospital where they gave birth when present puerperal infections, being attended in other institutions, increasing the gaps of registries.
5Hemorrhage occurred in 9.2% of cases. A study that used data from Birth in Brazil reports a prevalence of 4.3%
7 and in Northeast, 10.4%.
9 A study conducted in Ethiopia demonstrated an incidence of 8.8% of postpartum primary hemorrhage.
4 According to World Health Organization, Postpartum Hemorrhage (PPH) afflicts about 2% of every women who gave birth and is associated with up to 25% of maternal deaths in the world.
21 This datum may also be underestimated, since similar difficulties were found in different studies in relation to data collection from medical records about hemorrhage and it may exist a difficulty of visually estimate blood loss, which may negatively interfere in this registry.
7,9,22A “high temperature” measured in the thermometer (two or more interventions/complications) occurred in 33.1% of cases, and the variables that presented higher risk in the adjusted model (which evidenced a good adjustment) were: history of cesarean section, being hospitalized during pregnancy and being from social class A or B.
Being hospitalized in pregnancy increased the risk of “high temperature” more than eight times. It is presumed that the pathology or complication that indicated hospitalization is related to complications found – for example, hospitalization for preterm labor, but it probably will be shown as “newborn complication”, since the preterm neonate should have intensive care. This fact can be verified by the increase of cesarean section risk (abdominal scar), also of newborn related complications. The increase of interventions/complications in the group of women that already underwent cesarean section was of more than 2.5 times, which can be explained by the higher prevalence of a new cesarean section in this group
23 (“scar complication”) and by the greater risk of other complications, such as abnormal placentation and uterine rupture, which also implied risks to neonates.
23 The studied maternity hospital is a tertiary reference service, with higher probability of one of its patients have higher propensity of initiating the mentioned events, which arise the “temperature”, both individual and that of the institution.
In contrast to what was expected, in this study, there was an association of “high temperature” from complications/interventions with belonging to higher income classes (A/B) with odds ratio 2.67. This finding can be explained because this group of women had in higher proportion the harm related to perception of safety. Women of higher social class may have further expectations and be more critical in relation to the attitudes of the assistance team.
24Other factors (schooling, skin color, overweight or obesity, living with partner) did not influence the “temperature” of the thermometer in this sample. Differences may be explained by the fact that the sample size is not sufficient to measure any difference, or perhaps, by the differences in study locations, because of different contexts of assistance.
The few twin pregnancies of the sample had association with the complications “scar”, “hemorrhage” and neonate related complications. Literature review showed data converging with that found in the current study, with increase of severe maternal morbidity, maternal near miss and morbimortality.
25Although the study locus is a hospital that attends 100% for SUS, the population in the sample was mostly white, with high schooling and belonging to social classes A and B. A factor to be considered is that it may have occurred selection bias, in which women with higher schooling were more prone to answer to the questionnaire.
As a limitation of the study, it was also conceived that the hypothesis of the registry of some complications is defective, mainly in relation to infections and hemorrhage, important causes of maternal death. Thus, mentioned complications may be underestimated, such as in other studies.
7,9 We suggest that educational institutional measures should be taken in order to improve these registries.
Besides, the number of assessed women and distribution of women between the groups with few women in each analysis branch may have impaired the statistical analysis. There are important differences between this study and other similar studies, such as the exclusion of preterm births in the study conducted by Salgado
et al.7 and the type of assessment of perineal complication of two similar studies,
7,9 impairing comparations.
Nonetheless, it was possible to find a rate of care free of interventions and complications higher than in other studies, a low rate of severe perineal lacerations, which may be reflex of a policy of a very restrict use of episiotomy, and a percentage of cesarean section similar to that of the year previous to the pandemic and lower than the Brazilian mean.
Data were collected during COVID-19 pandemic, but there is only data previous to pandemic regarding rate of cesarean section and episiotomy, which do not evidence differences. We suggest a new data collection after pandemic, in order to verify whether modifications occurred, both in interventions and in complications.
The search for care without interventions and complications and for women’s satisfaction achieved should be a goal in healthcare, particularly in obstetric care, since a non-satisfactory birth experience brings important risks to the binomial, which can remain for years. More studies are necessary to identify reasons and ways of solution for the perception of inadequacy of the care received by some women.
According to criteria of the Maternity Safety Thermometer, the complications and interventions of the study population were: trauma 65%, being 38.5% abdominal trauma (cesarean) and 26.5% perineal trauma (considering perineal lacerations of 2º degree or more); complication related to the perception of safety by the person attended 30%; complications related to the newborn (12.3%); infection complication 11.2% and hemorrhage complication 9.2%. 33.1% of participants had a high temperature of interventions/complications (more than one).
References1. World Health Organization (WHO). WHO recommendations: Intrapartum care for a positive childbirth experience. Geneva: WHO; 2018. [access in 2022 jun 12]. Availble from:
https://www.ncbi.nlm.nih.gov/books/NBK513809/pdf/Bookshelf_NBK513809.pdf2. Leal MC, Pereira APE, Domingues RMSM, Filha MMT, Dias MAB, Nakamura-Pereira M,
et al. Intervenções obstétricas durante o trabalho de parto e parto em mulheres brasileiras de risco habitual. Cad Saúde Pública. 2014; 30 (Supl. 1): S17-32.
3. Knobel R, Lopes TJP, Menezes MO, Andreucci CB, Gieburowski JT, Takemoto MLS. Taxas de cesariana no Brasil de 2014 a 2016: Análise transversal utilizando a classificação de Robson. Rev Bras Ginecol Obstet. 2020; 42 (9): 522-8.
4. Tiruneh B, Fooladi E, McLelland G, Plummer V. Incidence, mortality, and factors associated with primary postpartum haemorrhage following in-hospital births in northwest Ethiopia. PLoS One. 2022 Apr; 17 (4): e0266345.
5. Axelsson D, Blomberg M. Prevalence of postpartum infections: a population-based observational study. Acta Obstet Gynecol Scand. 2014; 93 (10): 1065-8.
6. Herdt MCW, Magajewski FRL, Linzmeyer A, Tomazzoni RR, Domingues NP, Domingues MP. Temporal Trend of near Miss and its Regional Variations in Brazil from 2010 to 2018. Rev Bras Ginecol Obs. 2021; 43(2): 97-106.
7. Salgado HO, Queiroz MR, Santos HG, Andreucci CB, Diniz CSG. Using the Maternity Safety Thermometer to estimate harm‐free care in Southeast Brazil: A hospital‐based cohort. Birth. 2019; 46 (4): 583-91.
8. Salgado H, Souza J, Sandall J, Diniz C, Salgado HO, Souza JP,
et al. Patient Safety in Maternity Care in Brazil: The Maternity Safety Thermometer as a Tool to Improve the Quality of Care. Rev Bras Ginecol Obs. 2017; 39 (5): 199-201.
9. Melo CR. Adaptação transcultural do maternity safety thermometer para o português do Brasil. [tese] Florianópolis: Programa de Pós-graduação em Enfermagem da Universidade Federal de Santa Catarina; 2015.
10. Power M, Fogarty M, Madsen J, Fenton K, Stewart K, Brotherton A,
et al. Learning from the design and development of the NHS Safety Thermometer. Int J Qual Heal Care. 2014; 26 (3): 287-97.
11. Andreucci CB, Knobel R. Social determinants of COVID-19-related maternal deaths in Brazil. Lancet Reg Heal Am. 2021 Nov; 3: 100104.
12. Martin MM, Knobel R, Nandi V, Pereira JG, Trapani Junior A, Andreucci CB. Adequacy of Antenatal Care during the COVID-19 Pandemic: Observational Study with Postpartum Women. Rev Bras Ginecol Obstet. 2022; 44 (4): 398-408.
13. Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen Y-F, Choudhury NN,
et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health. 2020 Aug; 5 (8): e003042.
14. Siqueira TS, Silva JRS, Souza MR, Leite DCF, Edwards T, Martins-Filho PR,
et al. Spatial clusters, social determinants of health and risk of maternal mortality by COVID-19 in Brazil: a national population-based ecological study. Lancet Reg Health Am. 2021; 3: 100076.
15. Associação Brasileira de Empresas de Pesquisa (ABEP). Criterio de Classificação Econômica Brasil. São Paulo; 2018. [access in 2022 jun 12]. Availble from:
https://www.abep.org/criterio-brasil16. Tomasi E, Fernandes PAA, Fischer T, Siqueira FCV, Silveira DS, Thumé E,
et al. Qualidade da atenção pré-natal na rede básica de saúde do Brasil: indicadores e desigualdades sociais. Cad Saúde Pública. 2017; 33(3): 1-11
17. Sens MLSM, Tiedje AR, Knobel R, Trapani Junior A. Avaliação do desfecho da via de parto na pandemia de COVID. In: Anais 59
o Congresso Brasileiro de Ginecologia e Obstetricia [
Internet]; 17- 20 nov 2021; Rio de Janeiro (RJ): FEBRASGO; 2021. [access in 2022 jun 12]. Availble from:
https://www.cbgo2021.com.br/evento/cbgo2021/trabalhosaprovados/naintegra/476 18. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017 Feb; 2 (2): CD000081.
19. Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D,
et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019; 7 (1): e37-46.
20. Agencia Nacional de Vigilância Sanitária (ANVISA). Medidas de Prevenção e Critérios Diagnósticos de Infecções Puerperais em Parto Vaginal e Cirurgia Cesariana. Brasília (DF): ANVISA; 2017. [access in 2022 jun 12]. Availble from:
http://antigo.anvisa.gov.br/documents/33852/3507912/Caderno+8+-+Medidas+de+Preven%C3%A7%C3%A3o+e+Crit%C3%A9rios+Diagn%C3%B3sticos+de+Infec%C3%A7%C3%B5es+Puerperais+em+Parto+Vaginal+e+Cirurgia+Cesariana/08dee73e-ffef-433f-8fb8-c5f7fc8053a021. Organização Mundial da Saúde (OMS). Recomendações da OMS para a prevenção e tratamento da hemorragia pós-parto. Geneva: OMS; 2014. [access in 2022 jun 12]. Availble from:
http://apps.who.int/iris/bitstream/handle/10665/75411/9789248548505_por.pdf22. Organização Pan-americana da Saúde (OPAS). Recomendações assistenciais para prevenção, diagnóstico e tratamento da hemorragia obstétrica. Brasília (DF); 2018. [access in 2022 jun 12]. Availble from:
https://iris.paho.org/bitstream/handle/10665.2/34879/9788579671241-por.pdf?sequence=1&isAllowed=y23. ACOG. ACOG Pract Bulletin Nº. 205 Vaginal Birth After Cesarean Delivery. Obstet Gynecol. 2019; 133 (2): e110-27.
24. Adnan FI, Noor NM, Mat Junoh NA. Associated factors of labor satisfaction and predictor of postnatal satisfaction in the north-east of Peninsular Malaysia. PLoS One. 2020; 15 (8): e0238310.
25. Scaranello Santana D, Garanhani Surita F, Guilherme Cecatti J. Multiple Pregnancy: Epidemiology and Association with Maternal and Perinatal Morbidity. Rev Bras Ginecol Obstet. 2018; 40: 554-62.
Received on April 7, 2022
Final version presented on June 13, 2022
Approved on August 10, 2022
Author’s contribution: Nandi VL and Pereira JG: project conceptualization, data collection and organization, data analysis and interpretation, writing of the manuscript. Knobel R e Martin MM: project conceptualization, data collection and organization, correction of inconsistencies, data analysis and interpretation, writing of the manuscript. Rocha MNMC and Arruda YLG: data collection and organization, correction of inconsistencies, data analysis and interpretation, writing of the manuscript. Trapani Junior A: project conceptualization, data analysis and interpretation, writing of the manuscript.
All authors approved the final version of the article and declared no conflict of interest.
 ; Roxana Knobel2
; Roxana Knobel2 ; Jéssica Goedert Pereira3
; Jéssica Goedert Pereira3 ; Marie Margot Martin4
; Marie Margot Martin4 ; Mariana Nunes Miranda Carasek da Rocha5
; Mariana Nunes Miranda Carasek da Rocha5 ; Yasmin Lima Gouveia Arruda6
; Yasmin Lima Gouveia Arruda6 ; Alberto Trapani Junior7
; Alberto Trapani Junior7