ABSTRACT
OBJECTIVES: to analyze the donation of human milk at the Banco de Incentivo e Apoio a Amamentação (BIAMA) (Breastfeeding Incentive and Support Bank) from 2018 to 2020.
METHODS: normative assessment, descriptive and exploratory character, with a quantitative approach and focus on the Donabedian Model. Study with a locus at BIAMA at Dom Malan Hospital, in the city of Petrolina-PE, based on registrations from the online platform of the Rede Brasileira de Bancos de Leite Humano (Brazilian Network of Human Milk Banks), with data from BIAMA from 2018 to 2020 and field activities.
RESULTS: in 2020, there was a decrease in the number of group assistance and medical consultations, in contrast to the increase in nursing consultations. Most of the milk supply comes from the external public, and in 2020 there was a reduction number of donors and in the volume of human milk collected.
CONCLUSIONS: COVID-19 pandemic had a negative impact on BIAMA activities and on milk donation, however, the use of new means of communication for patient care was observed. Even so, new donor recruitment strategies must be implemented. Regarding the main norms that regulate the operation of Human Milk Banks, most of the items listed are obeyed by BIAMA.
Keywords:
Breastfeeding, Human milk banks, Evaluation of the processes and results in health care
RESUMO
OBJETIVOS: analisar a doação de leite humano no Banco de Incentivo e Apoio a Amamentação (BIAMA) no período de 2018 a 2020.
MÉTODOS: avaliação normativa, de caráter descritivo e exploratório, com abordagem quantitativa e enfoque no Modelo Donabedian. Estudo com lócus no BIAMA do Hospital Dom Malan, na cidade de Petrolina-PE, a partir de registros da plataforma online da Rede Brasileira de Bancos de Leite Humano, com dados do BIAMA de 2018 a 2020 e atividades de campo.
RESULTADOS: em 2020, houve um decréscimo no número de atendimentos em grupo e de consultas médicas, em contrapartida, ao aumento das consultas de enfermagem. A maior parte do abastecimento de leite advém do público externo, e em 2020 foi observado uma redução no número de doadoras e no volume de leite humano coletado.
CONCLUSÕES: a pandemia de COVID-19 repercutiu de forma negativa em atividades do BIAMA e na doação de leite, no entanto, foi observado a utilização de novos meios de comunicação para atendimento dos pacientes. Ainda assim, novas estratégias para recrutamento de doadoras devem ser implementadas. Em relação às principais normas que regulamentam o funcionamento de Bancos de Leite Humano, a maioria dos itens elencados são obedecidos pelo BIAMA.
Palavras-chave:
Aleitamento materno, Bancos de leite humano, Avaliação de processos e resultados em cuidados de saúde
IntroductionExclusive breastfeeding up to six months of age provides the mother and the infant with many advantages. From the first hour of life, the elements present in breast milk protect the newborn (NB) against infections and reduce the risk of neonatal mortality. These benefits occur because this milk is a source of energy and contains high-quality nutrients that ensure food security for the infants.
1,2 Therefore, the World Health Organization and the Ministry of Health recommend exclusive breastfeeding until six months of age. Thus, the introduction of complementary food before the recommended age may be harmful to the child's health.
3,4Children who are breastfed have a lower risk of developing diseases such as infantile paralysis and urinary tract infection, as well as enterocolitis, autoimmune diseases, and especially respiratorial and gastrointestinal diseases. In addition, the infants perform better in school and are less likely to be overweight and obese. As for the mothers' benefits, breastfeeding contributes to her physical and psychological health, as well as strengthening the mother-baby bond. It is also possible to observe a better efficiency in decreasing the weight before the pregnancy and reducing the risk of developing ovarian and breast cancer.
1,2Given the importance of breastfeeding, Brazil stands out as a country that fosters actions to promote, protect, and support breastfeeding. Since the
Bancos de Leite Humano (BLH) (Human Milk Banks) was created after the establishment of
Rede Brasileira de Bancos de Leite Humano (rBLH-BR) (Brazilian Network on Human Milk Banks) throughout the country, with the purpose of assisting the mother-baby binomial and strengthening breastfeeding. Currently, Brazil has 224 BLHs distributed in all regions, and they are responsible for the actions to consolidate breastfeeding.
5The
Banco de Incentivo e Apoio a Amamentação (BIAMA), (Incentive and Support for Breastfeeding), founded more than 25 years ago, is part of this network. It is located in
Hospital Dom Malan in the city of Petrolina-PE, a maternal-infant unit that is a reference for 53 cities located in the IV Macro-region of Health in Pernambuco and in the North Region in Bahia. All the cities are part of the
Rede Interestadual de Saúde do Vale do São Francisco (Rede PEBA) (São Francisco Valley Interstate Health Network). BIAMA was the first to be implemented in the countryside of Pernambuco, and assists the population in the hospital by spontaneous demand and is a referral of other health services. In addition to collecting and processing donated milk, individual care (milking, treatment of mastitis, breast obstruction, and other breast complications) and group care (guidance and lectures), the bank offers primary support to newborns admitted at the hospital.
6The entire process of milk collection, selection, classification, processing, quality control, and distribution must follow the norms presented in the RDC No. 171 on September 4, 2006, BLH of the
Agência Nacional de Vigilância Sanitária (Anvisa), (National Health Surveillance Agency), which provides the technical regulations for the BLH operation and the Manual entitled "
Banco de leite humano: funcionamento, prevenção e controle de riscos", (Human milk bank: operation, prevention and risk control"), prepared by ANVISA in 2008. This manual provides professionals with information about the physical infrastructure, human resources, equipment, and instruments for the BLH operation and the collection centers.
7,8Given the relevance of the BLH, for its proper functioning and supply for the neonatal units, it should have mechanisms to recruit donors to engage volunteers to donate milk. Thus, according to the aforementioned standards, nursing mothers are considered suitable for donation when they are healthy, have a lactate production that exceeds the infant's needs, and do not use medications excreted in the milk which cause side effects in the child, among other criteria.
7,8In the context of the COVID-19 pandemic, in spite of the doubts concerning the safety of breastfeeding and human milk donation, the
Rede Brasileira de Bancos de Leite Humano (Brazilian Human Milk Banks Network) recommended to maintain breastfeeding even if the nursing mother is infected with COVID-19; however, hygiene and cleanliness standards should be followed to reduce the risk of virus transmission by respiratory droplets to the baby.
9However, in relation to milk donation, symptomatic mothers compatible with influenza syndrome, respiratory infection, or in case of a positive test for SARS-CoV-2, are considered unsuitable for donation during the period of viremia (14-day period from the first day of symptoms). In addition, women who have had home contact with patients diagnosed with SARS-CoV-2 flu syndrome are also subject to this restriction.
10Thus, the actions of recruitment, the carefulness selection of donors, and the quality of the milk offered give rise to manage responsibilities in order to protect infants and nursing mothers' health. In view of this, the present research aimed to analyze the donation of human milk in the period 2018 to 2020 in BIAMA, in the city of Petrolina-PE.
MethodsThis study is a normative evaluation, considering the management purpose, with a descriptive and exploratory character, through a quantitative approach.
11,12 The evaluation approach used refers to the Donabedian Model, focused on the classical management concepts.
13-15 The study was carried out at BIAMA of Dom Malan Hospital, in the city of Petrolina-PE.
The study was developed from secondary sources of records in reports of the online platform of the
Rede Brasileira de Bancos de Leite Humano (rBLH-BR) (Brazilian Network of Human Milk Banks) and field activities. The online platform provides data on: group activity, individual activity, collection, home visit, human milk collected (HMC), human milk distributed (HMD), microbiological examination, crematocrit, and Dornic acidity. The data collected were related to BIAMA in the period of 2018 to 2020, organized in spreadsheets and compared with the productivity of each year.
In addition, technical visits were made to BIAMA in the period from May to August 2021, applying the non-participant systematic observation method. The visits occurred on random days, chosen by drawing, to observe the procedures performed by different teams. The researcher witnessed the milk handling process, evaluated the organizational aspects that involve the recruiting and the selection of donors, and examined the data referring to milk donation highlighting positive points and critical nodes.
This set was observed in accordance with aspects established by the manual of ANVISA BLH operation, Technical Norms 09.21 and 10.21 (PCF-BLH-SUS)
16,17 and RDC 171/2006, reaching all environments involved in the milk processing and the population's care, through a collection of instrument prepared by the researchers themselves. This instrument presents criteria based on cited documents, classifying characteristics in agreement, in part, or in disagreement with the norms.
This research is part of a larger project entitled "
Estrutura e processos de banco de leite humano: referência para o Sertão do São Francisco-Pernambuco e Macrorregião Norte-Bahia" (Structure and processes of a human milk bank: reference for the Sertão do São Francisco-Pernambuco and North-Bahia Macroregion) approved by the Ethics Committee on Human Research at the
Instituto de Medicina Integral Prof. Fernando Figueira CEP-IMIP, opinion number 4.583.708 and CAAE 44104721.4.0000.5201.
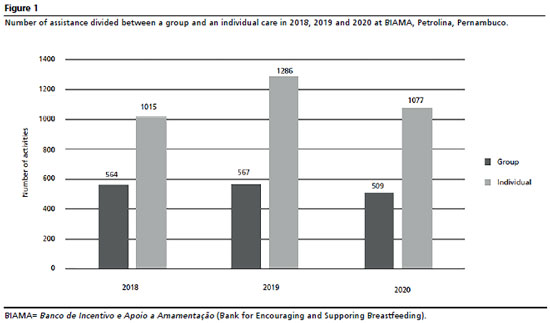
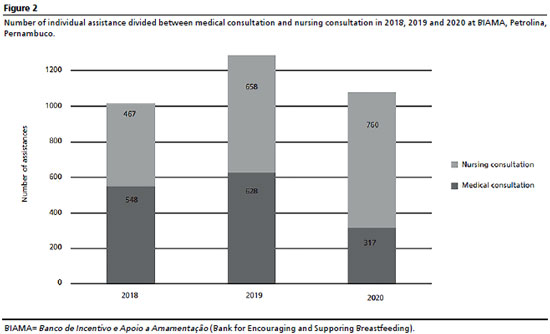
ResultsThe strategies to recruit breast milk donors of the BLHs involve individual and group consultations. In this sense, BIAMA obtained a total of 1,577 donors in the three years analyzed, and for this it performed 1,640 group consultations and 3,370 individual consultations divided between medical and nursing consultation (Figure 1). Considering the impact of the COVID-19 pandemic in 2020, we observed a decrease in relation to 2018 of 9.75% in group attendances and 42.1% in medical consultations. However, in relation to nursing consultations, a 62.7% increase in attendances was noted (Figure 2).
The breastfeeding promotion, protection, and support actions and the execution of activities to recruit donors carried out by BIAMA largely contemplate the items listed in the regulatory documents, among them, the pre and post natal guidance carried out in the outpatient clinic and in service sectors for pregnant and puerperal women, the post natal follow-up on pathologies related to breastfeeding, and the health network services such as basic health units, family health strategy, childbirth centers, and maternities, which are performed when requested. The activities and demands of the Human Milk Bank are advertised on radio, television, newspapers, and events; however, it does not reach schools as stated in the manual.
As for the individual care offered at BIAMA, it provides assistance to the external public, to puerperal women, hospitalized babies, and mothers who are in the support house at the hospital. This care is provided by a physician, nurse, or the technical nursing team. Regarding to the external public, the demand can be spontaneous or by appointment, and the service aims to address complaints in breastfeeding and/or to monitor the growth and development of children who seek the service for not presenting adequate weight gain. For hospitalized mothers and babies, the Milk Bank works 24 hours a day to fully assist this public.
Therefore, the group activity is a daily moment when pregnant women, hospitalized puerperal women, newborns, and companions are brought together into a lecture room, on different occasions, to talk about the main challenges and benefits of breastfeeding. In addition, the mothers who need individual care are identified at the Milk Bank are identified, whether it is for engorgement, breast emptying, mastitis, fissures, among others. With the COVID-19 pandemic, these group meetings stopped and the information and clarification of doubts about breastfeeding started to be given at each patient's bed, in three sectors of the hospital, namely: High Risk, Gynecology and Joint Accommodation.
In this process, the focus of these actions carried out by BIAMA is to encourage pregnant and puerperal women to become voluntary donors of human milk. When a donor is recruited, a registration form is filled out during the screening process. However, it was observed in BIAMA the lack of information considered mandatory, such as: place where prenatal care was performed, number of consultations, weight at the beginning and end of pregnancy, prenatal complications, and treatment.
The selection of the donor is made by the nursing team, as opposed to the normative that brings as the physician's responsibility. Still, to be considered as a human milk donor, all the requirements are met in BIAMA, which are: being healthy, breastfeeding or milking for their own child, presenting pre or post natal exams (hemogram, VDRL, anti-HIV, and other serologies usually researched at prenatal care) compatible with milk donation, smoking no more than ten cigarettes a day, not using medications incompatible with breastfeeding, and not consuming alcohol or illicit drugs.
However, the officialization of the registration and the validation of the information is not performed by the physician as determined in the normative. Due to the demand of the bank, there is no physician on duty daily, and the registration is done by the technical nursing team and the nurse of the sector.
Donation of human milkAfter the registration stage of the nursing mother is concluded, the first collection is monitored by a professional from BIAMA, and, whenever possible, the child's breastfeeding is observed, corrections are made, and guidance is given on the contraindication to the use of pacifiers, bottles, and nipples, in addition to offering water, tea, and other liquids before the age of six months.
In subsequent donations, in case of complication occurrence to the health of the nursing mother or the child, the nurse evaluates whether the donated product can be pasteurized. In simple cases, the nurse makes the necessary referrals to health services for treatment, in agreement with the physician, and in complex situations the physician defines the conduct to be taken. This routine goes against what is stated in the manual, which brings the responsibility to the physician's function to analyze the donation as adequate or not for pasteurization and evaluate the need to forward the donor to a health service.
As for checking the health status of the nursing mother at each donation of milk and checking the follow-up of the donor's child in the health units, and updating the vaccination schedule, these are not performed at BIAMA, as stated in the ANVISA BLH Operational Manual.
In Figure 3, it is possible to see that in 2020 there was a 17.3% decrease in the volume of human milk collection compared to 2019. With regard to donors, four hundred and sixty-one mothers donated milk during 2020, compared to six hundred and thirty-one donors in 2019, representing a 27.3% decrease. Despite these results, the bank showed similar productivity in proportion of liters collected per donor when comparing 2020 to 2018.
Milk donors from BIAMA are grouped between external and internal mothers (hospitalized, accompanying the hospitalized baby or in a support home, accompanying patients or with hospitalized children in other sectors of the hospital). The donated milk is collected at BIAMA or at home, following all technical and hygienic-sanitary procedures. The donors receive a kit for milk collection with containers, caps, and masks, and are instructed about the importance of its use, hand and breast hygiene, and sterilization of materials.
The receptors are newborns who have a stock of milk produced by their mothers, in addition to preterm and low birth weight NBs, or babies who have some indication according to the criteria, who are hospitalized at Dom Malan Hospital, in the Delivery Room, Surgical Block, Neonatal Intensive Care Unit (NICU), Pediatric Emergency, Outpatient Nursery, Conventional Intermediate Care Units (UCINCo) and Kangaroo Intermediate Care Unit (UCINCa).
In the period studied, the number of receptors is always higher than the number of donors (Figure 4). In 2019, the difference between donors and receptors was only 3.35%, while in 2020 this difference was 33.6%. The decrease in the number of donors between 2019 and 2020 was 27.28%. Given this, we realize the need for the use of strategies to recruit donors and the importance of the milk bank for the survival of hospitalized infants at the hospital.
With the objective of reaching donors who live in distant places, home visits are carried out when the nursing team collects the milk that has been taken from the donor, and intervenes on the mothers' complaints about breastfeeding and care during milking and storing milk.
Analyzing Figure 5, it is possible to observe that most of the milk supply toBIAMA comes from the external public, either during individual consultations at the bank or during home visits. Despite this, comparing the years 2018 and 2020, this volume of external HMC suffered a decrease of 2.7% and 11.6% compared to the internal HMC.
DiscussionStrategies for care in the milk bank in the pandemic periodAs previously observed, the decrease in the number of medical consultations at BIAMA in the year 2020 (Figure 1) can be justified by the progress of the COVID-19 pandemic, which led to a restriction in care to the external public, which represents the greatest demand in medical assistance. In this period, the alternative of real-time teleconsultations was sought, by video calls and phone calls on children's follow-ups or resolution of breastfeeding complaints. However, these tools have been used for assistance, they were not enough to recover the average annual assistance.
As a strategy to maintain breastfeeding in a pandemic context, some milk banks have also adopted assistance in a distance, through teleconsultations, in order to follow the recommendations in avoiding crowds. In Brazil, the
Centro de Referência Estadual de Banco de Leite Humano do Hospital Universitário Cassiano Antônio Moraes (CRE-BLH/HUCAM) (State Reference Center of Human Milk Bank of Cassiano Antônio Moraes University Hospital) adopted teleconsultation by videoconference and observed a positive result in the participation of puerperal women.
18 And in the international context, as in Poland, the lactation consultations of the Regional Milk Bank had made some alterations for the outpatients to make contact it had to be done by phone.
19Regarding nursing consultations, there was a significant increase in the assistance in 2020 (Figure 2). In this same period, care continued to be provided to spontaneous demand, to internal public in the hospital, and home visits. This highlights the nursing work as fundamental work from BIAMA, the time of adjustments in the routines and implementation of new health protocols. Marchiori
et al. ,
20 study evaluated the nursing actions in human milk banks during COVID-19, and observed the nursing coordination plan in minimizing the impacts of the pandemic on the HMB activities and digital media were allies for maintaining the policy of promoting, protecting, and supporting breastfeeding.
Regarding the actions carried out by BIAMA, the group activity corresponds to the moment of orientation and clarification of doubts about breastfeeding, and recruiting milk donors. Studies have shown that interventions and training to support breastfeeding resulted in an increase in mothers' level of knowledge, the duration of breastfeeding, and the rate of exclusive breastfeeding for six months.
21,22 In 2020, this collective activity of BIAMA became individual, which represented a difficult factor when added to the incomplete team due to health statements and other demands from the HMB. On the other hand, it also proved to be an opportunity to resolve complaints and particular doubts. However, despite the restrictions imposed by the pandemic, BIAMA made the necessary adjustments and continued the service.
Observation of the norms and approximation with Primary Health CareAs previously discussed, it was seen that some information considered mandatory in the norms are not yet registrated in BIAMA, for example, the lack of data in the donor's file, as the place where the donor had prenatal care, number of consultations, weight at the beginning and at the end of the pregnancy, complications during prenatal care and treatment. It was also found that, regarding to the donor's child, BIAMA did not observe the follow-up in the health units and the child's vaccination booklet. Considering this, it was realized that these data are sensitive to Primary Health Care (PHC)
23,24 and demonstrated the distance that can exist between PHC and HMB. Moreover, the absence of these data on pregnancy and follow-ups in the health unit can be justified by the number of professionals working in BIAMA and that may represent a limitation for the service.
In an integrative review, it was seen that in the Family Health Strategy, prenatal consultations are an important time to address issues such as breastfeeding and donation of human milk to the HMB and, moreover, the pregnant woman who was well oriented, understands better the importance of donating breast milk. However, the study found that many professionals are unaware of the main role in the HMB to promote breastfeeding, reporting to the bank only as an institution for collecting and distributing human milk.
25 Thus, it is necessary that intersectoral actions are being taken to promote strength and effective communication between these sectors.
Impact of the pandemic on milk bank productivityAs already exposed, the progress during COVID-19 pandemic had a negative impact on the productivity at BIAMA. Analyzing the last three years, the number of receptors was higher when compared to the number of donors (Figure 4), this deficit highlights the need to engage in strategies to recruit lactating mothers for milk donation, considering human milk as a vital element for hospitalized children.
Regarding the reduction in the number of donors and the volume of human milk collected in 2020 (Figure 3), studies have also reported a similar outcome in other milk banks. Thus, the lack of knowledge about virus transmission through human milk, travel limitations, and the insecurity of going to the hospital or receiving health professionals at home may have influenced this negative result.
26-28Some milk banks abroad used strategies to maintain milk collection during the pandemic. Among them, the implementation of home collecting system of donated milk and campaigns for milk donation was directed to mothers with hospitalized children and to the external public, through social networks and other means of communication.
26 In addition, information about the safety of donating milk was provided to donors and potential donors through phone calls, informative leaflets via e-mail, posts on Facebook and on the websites mentioning about the importance of breastfeeding in the midst of the pandemic.
29 These actions provided the maintenance of activities, the supply of milk banks, and the guarantee of supplying for neonatal units.
These strategies are already practiced by BIAMA and did not stop during the pandemic period; however, due to the restrictions, such as the reduction of in-person services to the external public and cancellation of group services, there was a decrease in donors and, consequently, in the number of HMC.
We conclude in this study that the limitations imposed by COVID-19 pandemic had a negative impact on most of the activities from BIAMA and its results related to milk donation. Still, despite the operational challenges experienced in this context, the nursing team stood out in the number of assistance and showed itself as a participating team in all stages related to the selection and recruiting donors and milk donation. Moreover, it was observed the use of new means of communication for remote management of patients and for medical appointments.
The results observed show that new strategies for recruiting donors should be implemented at BIAMA. It is suggested to bring the bank and the basic health network closer to the city, through visits, courses, and team training. In addition, the use of social networks that are currently increasing in reaching people, when compared to television, radio, and newspapers. This interaction in creating strategies to recruit donors is to justify the fact that the milk bank is vital for the survival of hospitalized newborns and infants.
Even in view of the information provided in this study, some limitations can be pointed out, such as the lack of research on the routine and productivity of HMB. It is also possible to emphasize that the evaluation of only one HMB presents a barrier to compare with other scenarios. Thus, it is suggested that further research with an analysis similar to this study will be carried out in other HMB to create strategies to recruit donors through the use of active methodologies.
Most of the items listed in both norms are complied by BIAMA. Thus, it is suggested that this studyshould be used as an adjustment tool for the aspects observed in the bank.
References1. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Saúde da criança: aleitamento materno e alimentação complementar. Brasília (DF); 2015. 2ª ed. [access in 2022 Dez 6]. Available from:
https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/s/saude-da-crianca/publicacoes/saude-da-crianca-aleitamento-materno-e-alimentacao-complementar/view2. Organização Pan-Americana da Saúde (OPAS). Benefícios da amamentação superam riscos de infecção por COVID-19, afirmam OPAS e OMS. Brasília (DF); 2020 [access in 2020 Out 15]. Available from:
https://www.paho.org/pt/noticias/1-9-2020-beneficios-da-amamentacao-superam-riscos-infeccao-por-covid-19-afirmam-opas-e-oms#:~:text=O%20risco%20de%20infec%C3%A7%C3%A3o%20pela,da%20OPAS%2FOMS%20no%20Brasil.3. World Health Organization (WHO). Guideline: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. Geneva: WHO; 2017. [access in 2020 Out 15]. Available from
https://www.who.int/publications/i/item/97892415500864. Carvalho MR, Gomes CF. Amamentação: bases científicas. 4ª. ed. Rio de Janeiro: Guanabara Koogan; 2017.
5. Fundação Oswaldo Cruz (Fiocruz). História. Rede Global de Bancos de Leite Humano. [Internet] Rio de Janeiro; 2005 [access in 2020 Nov 13]. Available from:
https://rblh.fiocruz.br/quem-somos6. Secretaria Estadual de Saúde de Pernambuco. Biama convoca para doação de leite humano e potes de vidro. [Internet] Recife; 2021. [access in 2022 Jan 5]. Available from:
http://portal.saude.pe.gov.br/noticias/secretaria-executiva-de-atencao-saude/biama-convoca-para-doacao-de-leite-humano-e-potes-de7. Ministério da Saúde (BR). Resolução- RDC nº 171, de 4 de setembro de 2006. Dispõe sobre o Regulamento Técnico para o funcionamento de Bancos de Leite Humano [access in 2022 Fev 10]. Available from:
https://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2006/res0171_04_09_2006.html8. Agência Nacional de Vigilância Sanitária (ANVISA-BR). Banco de leite humano: funcionamento, prevenção e controle de riscos. Brasília (DF); 2008.
9. Rede Brasileira de Bancos de Leite Humano (rBLH-BR). Covid-19 e Amamentação - Recomendação técnica Nº01/20.170320. Rio de Janeiro; 2020. [access in 2022 Fev 10]. Disponível em:
https://rblh.fiocruz.br/covid-19-e-amamentacao-recomendacao-n012017032010. Rede Brasileira de Bancos de Leite Humano (rBLH-BR). Covid-19 e Doação de Leite Humano - Recomendação técnica Nº02/20.170320. Rio de Janeiro; 2020. [access in 2022 Fev 10]. Available from:
https://rblh.fiocruz.br/sites/rblh.fiocruz.br/files/usuario/80/recomendacao_tecnica_no.0220.170320_covid-19_e_doacao_de_leite_humanoo__0.pdf11. Pedrosa JIS. Perspectivas na avaliação em promoção da saúde: uma abordagem institucional. Ciênc Saúde Colet. 2004; 9 (3): 617-26.
12. Menezes AHN, Duarte FR, Carvalho LOR, Souza TES,
et al. Metodologia científica: teoria e aplicação na educação a distância. Petrolina: Fundação Universidade Federal do Vale do São Francisco-UNIVASF. Livro digital; 2019. [access in 2022 Fev 10]. Available from:
https://portais.univasf.edu.br/dacc/noticias/livro-univasf/metodologia-cientifica-teoria-e-aplicacao-na-educacao-a-distancia.pdf13. Akerman M, Nadanovsky P. Avaliação dos serviços de saúde: avaliar o quê?. Cad Saúde Pública. 1992; 8 (4): 361-5.
14. Medronho RA. Epidemiologia. São Paulo: Atheneu; 2006.
15. Pereira MG. Epidemiologia: Teoria e Prática. Rio de Janeiro: Guanabara Koogan; 2006.
16. Rede Brasileira de Bancos de Leite Humano (rBLH-BR). Normas Técnicas BLH-IFF/NT 09.21 - Doadoras: Triagem, Seleção e Acompanhamento. Rio de Janeiro; 2021. [access in 2022 Fev 10]. Available from:
https://rblh.fiocruz.br/sites/rblh.fiocruz.br/files/usuario/116/nt_09.21_-_doadoras_triagem_selecao_e_acompanhamento_0.pdf17. Rede Brasileira de Bancos de Leite Humano (rBLH-BR). Normas Técnicas BLH-IFF/NT 10.21 - Filho da Doadora: Acompanhamento. Rio de Janeiro; 2021. [access in 2022 Fev 10]. Available from:
https://rblh.fiocruz.br/sites/rblh.fiocruz.br/files/usuario/116/nt_10.21_-_filho_da_doadora_acompanhamento_0.pdf18. Azevedo EHM, Pontes MB, Martins SW, Nunes JA. Estratégias de intervenção na Rotina de Cuidados no Banco de Leite Humano diante da pandemia de COVID-19. [Cartas] CoDAS. 2020; 32 (5): e20200210.
19. Sinkiewicz-Darol E, Bernatowicz-Łojko U. Operation of the First Regional Milk Bank in Poland During a SARS-CoV-2 (COVID-19) Pandemic. J Hum Lact. 2020 Nov; 36 (4): 626-7.
20. Marchiori GRS, Alves VH, Pereira AV, Vieira BDG, Rodrigues DP, Dulfe PAM,
et al. Nursing actions in human milk banks in times of COVID-19. Rev Bras Enferm. 2020; 73 (Supl. 2): e20200381.
21. Renfrew MJ, McCormick FM, Wade A, Quinn B, Dowswell T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2012: CD001141.pub4. [access in 2022 Fev 14]. Available from:
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001141.pub4/full22. Yılmaz M, Aykut M. The effect of breastfeeding training on exclusive breastfeeding: a randomized controlled trial. J Matern Fetal Neonatal Med. 2021; 34 (6): 925-32.
23. Ministério da Saúde (BR). Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco. Secretaria de Atenção à Saúde. Brasília (DF): Ministério da Saúde; 2012. [access in 2023 Mar 6]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/cadernos_atencao_basica_32_prenatal.pdf24. Ministério da Saúde (BR). Departamento de Atenção Básica. Saúde da criança: crescimento e desenvolvimento. Brasília: Ministério da Saúde; 2012. [access in 2023 Mar 6]. Available from:
https://bvsms.saude.gov.br/bvs/publicacoes/saude_crianca_crescimento_desenvolvimento.pdf.25. Luna FDT, Oliveira JDL, Silva LRM. Banco de leite humano e estratégia saúde da família: parceria em favor da vida. Rev Bras Med Fam Comunidade. 2014; 9 (33): 358-64.
26. Romera MP, Caballero PM, Álvarez EM, López LS, Suazocal JAH. Impacto de la pandemia por SARS-CoV-2 en un banco de leche humana [Impact of the SARS-CoV-2 pandemic on a human milk bank]. Nutr Hosp. 2021 Jul; 38 (4): 710-4.
27. Sachdeva RC, Jain S, Mukherjee S, Singh J. Ensuring Exclusive Human Milk Diet for All Babies in COVID-19 Times. Indian Pediatr. 2020 Aug 15; 57 (8): 730-3.
28. Rigourd V, Lapillonne A. A Call to Ensure Access to Human Milk for Vulnerable Infants During the COVID-19 Epidemic. J Hum Lact. 2020 Nov; 36 (4): 624-5.
29. Jayagobi PA, Mei Chien C. Maintaining a Viable Donor Milk Supply During the SARS-CoV-2 (COVID-19) Pandemic [Letter]. J Hum Lact. 2020 Nov; 36 (4): 622-3.
Received on August 8, 2022
Final version presented on May 19, 2023
Approved on May 22, 2023
Associated Editor: Luciana Dubeux
Authors' contribution: Gonçalves SEMCS, Medeiros KG and Coelho GMP: conception and design of the study, data analysis and interpretation, writing and review of the manuscript. All authors approved the final version of the article and declare no conflict of interest.
 ; Kaliane Gomes Medeiros2
; Kaliane Gomes Medeiros2 ; Glória Maria Pinto Coelho3
; Glória Maria Pinto Coelho3